Abstract
Background
Cellulose acetate phthalate (CAP) has been used for several decades in the pharmaceutical industry for enteric film coating of oral tablets and capsules. Micronized CAP, available commercially as "Aquateric" and containing additional ingredients required for micronization, used for tablet coating from water dispersions, was shown to adsorb and inactivate the human immunodeficiency virus (HIV-1), herpesviruses (HSV) and other sexually transmitted disease (STD) pathogens. Earlier studies indicate that a gel formulation of micronized CAP has a potential as a topical microbicide for prevention of STDs including the acquired immunodeficiency syndrome (AIDS). The objective of endeavors described here was to develop a water dispersible CAP film amenable to inexpensive industrial mass production.
Methods
CAP and hydroxypropyl cellulose (HPC) were dissolved in different organic solvent mixtures, poured into dishes, and the solvents evaporated. Graded quantities of a resulting selected film were mixed for 5 min at 37°C with HIV-1, HSV and other STD pathogens, respectively. Residual infectivity of the treated viruses and bacteria was determined.
Results
The prerequisites for producing CAP films which are soft, flexible and dispersible in water, resulting in smooth gels, are combining CAP with HPC (other cellulose derivatives are unsuitable), and casting from organic solvent mixtures containing ≈50 to ≈65% ethanol (EtOH). The films are ≈100 µ thick and have a textured surface with alternating protrusions and depressions revealed by scanning electron microscopy. The films, before complete conversion into a gel, rapidly inactivated HIV-1 and HSV and reduced the infectivity of non-viral STD pathogens >1,000-fold.
Conclusions
Soft pliable CAP-HPC composite films can be generated by casting from organic solvent mixtures containing EtOH. The films rapidly reduce the infectivity of several STD pathogens, including HIV-1. They are converted into gels and thus do not have to be removed following application and use. In addition to their potential as topical microbicides, the films have promise for mucosal delivery of pharmaceuticals other than CAP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Polymers, used in the past as pharmaceutical excipients and in drug delivery, are increasingly being considered for specific therapeutic and prophylactic applications [1–5]. They appear promising for topical applications as microbicides to prevent infection by sexually transmitted disease (STD) pathogens, including the human immunodeficiency virus (HIV-1) [6]. One of these promising polymeric microbicides is cellulose acetate phthalate (CAP) [7–14]. CAP has been used for enteric film coating of tablets and capsules [15] and thus has a well-established safety record for human use. CAP is not soluble in water at pH <≈5.8. For this reason, it must be used in a micronized form for both tablet coating from water dispersions, and as a topical microbicide. Micronization is accomplished by pseudolatex emulsion processes [16–24]. A micronized form of CAP available commercially under the trade name "Aquateric" (FMC Corporation, Philadelphia, Pennsylvania, USA) (containing 63 to 70% CAP, Poloxamers and acetylated monoglycerides) in appropriate gel formulations was shown to inactivate HIV-1 and several other STD pathogens in vitro and in animal models [7–9, 14]. Micronized CAP was shown to be the only candidate microbicide having the capacity to remove rapidly by adsorption HIV-1 from physiological fluids and render the virus noninfectious.
Microbicidal gels with or without contraceptive activity have some disadvantages. They need applicators for topical delivery adding to cost [25] and generating disposal problems. Furthermore distinct applicator dimensions may be preferred by distinct populations, and their packaging and size may not be optimal for discretion related to purchase, storage and use. Microbicidal gel production and applicator manufacture are likely to occur at different sites, and high capacity applicator filling equipment is required for large volume production. These drawbacks can be overcome by unit dose biodegradable films dispersible in water and having the following properties: 1) the microbicidal activity is a built-in property of the films, i.e. the active ingredient is an integral structural component of the films; 2) the films absorb physiological fluids and then disintegrate; 3) infectious agents bind to the resulting structures and become rapidly inactivated; 4) the films are converted into a soft gel which does not have to be removed; 5) simplicity of use and no "messiness"; 6) small packaging, facilitating discretion related to purchase, storage and portability; 7) low production price and suitability for use in developing countries; 8) amenability to industrial mass production; 9) Integration of manufacture and packaging; 10) Low cost of transportation due to the small size and weight of a unit dosage; 11) capacity to augment a healthy acidic vaginal environment and 12) potential for modifications leading to their application as rectal microbicides. A device having most of these properties is a sponge prepared by freeze-drying a foam generated from a water suspension of Aquateric in a solution of bioadhesive partially substituted ethers of cellulose (e.g. hydroxypropyl methylcellulose, methylcellulose, hydroxyethyl cellulose and hydroxypropyl cellulose (HPC). Alternatively, the sponges can be prepared by freeze-drying a microemulsion [26] of CAP in ethyl acetate mixed with a water solution of one of the cellulose ethers. These sponges contained 34 to 40% of the active ingredient, CAP. The advantages of the unit dose sponges are extenuated by the relatively high cost of freeze-drying. This would limit their use as a microbicide in developing countries. Therefore, alternative approaches had to be explored, the objective being the development of a unit dose water dispersible device, the production of which does not require freeze drying.
Water soluble or dispersible films are being used for drug delivery onto mucosal surfaces [27–30]. Films are also an established delivery vehicle for the administration of vaginal products. Contraceptive films have been marketed since the 1980's and there have been no concerns about the safety of this method of administration. There was an 86% compliance with film use in a phase III human efficacy trial of a contraceptive film containing Nonoxynol-9 (N-9). Although the trial failed due to the undesirable properties of N-9, the very high compliance rate shows that films represent a microbicide delivery method which is easy and acceptable [31–34]. These findings have led us to develop CAP based microbicidal films.
The HIV-1 epidemic is maintained and progresses mostly due to sexual transmission of the virus [35] and is facilitated by prior infections with non-viral STD pathogens [36–40] and herpesviruses (HSV) [41–43]. The estimated annual worldwide incidence of non-viral STD pathogens is over 330 million [44]. About 20 % of the United States population has been infected with HSV-2, the prevalence of such infections being even higher in developing countries [45]. Organisms associated with bacterial vaginosis (BV) also increase the susceptibility to HIV-1 infection [46]. For these reasons, broad spectrum microbicides acting not only against HIV-1 but also against other STD pathogens would be expected to have the greatest impact in preventing STDs including AIDS. Micronized CAP was shown to act in vitro [7, 10–14, 47–49] and in some animal model systems [8, 9] as a compound with broad spectrum activities. This had to be confirmed for the film formulation of CAP.
Methods
Preparation and physical properties of CAP-HPC film
CAP, HPC (150–400 cps, NF, Spectrum, New Brunswick, New Jersey, USA), HPC (4,000–6,500 cps, NF, Spectrum) and glycerol were dissolved in acetone-ethanol (EtOH) 4:6 at final concentrations of 2, 1, 1, and 1 % (w/w), respectively. The viscous liquids were poured into Teflon® coated steel or aluminum foil dishes (0.425 g/cm2) which were subsequently kept for 16 hr at 40°C followed by 1 hr in a vacuum oven at 50°C to dry the films.
To measure the kinetics of film conversion into a gel, the film was shredded into ≈1 mm2 pieces in a Guardian Cross-Cut Shredder (Quartet GBC, Skokie, Illinois, USA) and added at 75 mg/ml to either water or human seminal fluid (New England Immunology Associates, Cambridge, Massachusetts, USA). Viscosity was measured in a DV-3 P R digital viscometer (Anton Paar GmbH, Graz, Austria) using a TR-8 spindle at speeds decreasing from 200 to 2 r.p.m.
Imaging of cast films was performed with a JEOL 6500 Field Emission scanning electron microscope (JEOL USA, Inc., Peabody, Massachusetts, USA) at a magnification of 5,000 ×. Scanning white light interferometric microscopy was performed on both sides of the film at a magnification of 25 × (Fig. 1b,1c). CAP particles obtained after complete dispersion of the film were pelleted by centrifugation at 10,000 × g for 5 min, washed with water to remove excess HPC, and freeze dried. The particles were dispersed in water and measured by automated scanning electron microscopy using a JEOL 6400 scanning electron microscope coupled with a NORAN Voyager system (NORAN Instruments, Inc., Middleton, Wisconsin, USA). Imaging of the particles on a carbon substrate was performed using the JEOL 6500 electron microscope.
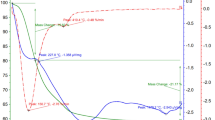
Morphology of CAP-HPC composite film H and of particles after film dispersion in water. a, Scanning electron microscopy of film H (side "A" exposed to air during drying). b, 3-dimensional (3-D) interactive display of side "A" of film H. c, 3-D interactive display of film H (side "B" in contact with the casting surface during drying). b, c, Color bar corresponds to elevation scale. d, Kinetics of conversion of shredded film H into a gel as measured by increase of viscosity. e, Scanning electron microscopy of CAP particles from the gel. f, Size distribution of the particles. Scale bar for a and e is 1 µ.
Measurements of infectivity of HIV-1 and herpesviruses (HSV)
To measure HIV-1 infectivity, virus was precipitated from tissue culture media containing 10% fetal bovine serum with polyethylene glycol 8000 (final concentration 10 mg/ml). The pellet containing virus was dissolved in 225 µl aliquots of 0.14 M NaCl, 0.01 M Tris(hydroxymethyl)aminomethane, pH 7.2 (TS). The aliquots were pre-warmed to 37°C and precut pieces of film H were added. After 5 min at 37°C, 1.225 ml of tissue culture medium was added and the mixtures were centrifuged for 1 hr at 14,000 r.p.m. in an Eppendorf 54156 microfuge (Brinkmann Instruments, Inc., Westbury, New York, USA) to pellet the virus. The virus was redissolved, serially diluted twofold (2 × to 2,048 ×), and the dilutions tested for infectivity using HeLa-CD4-LTR-ß-gal and MAGI-CCR5 cells for HIV-1 IIIB and HIV-1 BaL, respectively. Virus replication was quantitated by measuring ß-galactosidase (ß-gal) activity in cell lysates as described elsewhere in detail [14]. In a parallel series of experiments, residual film H was removed by centrifugation at 2,000 r.p.m. for 5 min from the film-virus mixtures before pelleting the virus at 14,000 r.p.m. The infectivities of control and film H treated HSV-1 and HSV-2, respectively, were measured under similar conditions as described for HIV-1 [7]. HSV-1 was a recombinant virus, vgCL5, in which the expression of ß-gal is under the control of the late gene C regulatory region. Vero cells were used for infection which was monitored by measuring ß-gal activity. ELVIS HSV cells (Diagnostic Hybrids, Inc., Athens, Ohio, USA), containing a LacZ gene placed behind an inducible HSV promoter, were used for infection by HSV-2. Infection was determined by measuring ß-gal.
Inactivation of non-viral STD pathogens and bacteria associated with bacterial vaginosis (BV)
The bacterial strains and the corresponding growth media were obtained from the American Type Culture Collection (ATCC, Manassas, Virginia, USA) and were the same as described earlier [7, 10]. Mycoplasma capricolum was ATCC #23205. Graded quantities of film H (0 to 150 mg/ml) were added to suspensions of the respective bacteria (8 × 108 to 1 × 109/ml in TS) pre-warmed to 37°C. After 5 min at 37°C, the suspensions were diluted 10-fold in the appropriate growth medium, centrifuged to pellet the bacteria which were then resuspended in the original volume of growth medium. Serial 10-fold dilutions in the appropriate growth media were made, and after incubation at 37°C (30°C for Haemophilus ducreyi) for 20 hr to 5 days, depending on the bacterial strain, turbidity was measured at 600 nm. Serial twofold dilutions (100 µl) of control and film H treated Chlamydia trachomatis were added to 9 × 104 McCoy cells plated into wells of 96-well microtiter plates. After 48 hr, the cells were fixed and stained with fluorescein isothiocyanate labeled monoclonal antibodies to Chlamydia (Diagnostic Hybrids) and the fluorescent inclusion bodies were counted following the procedures provided by the manufacturer. The percentages of residual infectivity for each film treated organism were calculated by comparing the respective dose response curves with readout vs. dilution curves corresponding to each of the respective control organisms.
Results
Casting of CAP films
CAP is moisture sensitive during long term storage [15]. Therefore, organic solvents had to be used for film casting. This appeared counterintuitive since CAP films cast from organic solvents are water resistant [15], and start dissolving only at pH > ≈5.8. Furthermore, none of the mucoadhesive cellulose ethers are soluble in organic solvents which dissolve CAP [15], except for HPC which is soluble in methylene chloride [50]. HPC is also one of the best bioadhesive polymers among cellulose ethers [51]. It was possible to prepare composite CAP (40%) – HPC (40%) – glycerol (20%) films cast from one of the following solvents: ethyl acetate; glacial acetic acid; methylene chloride; and acetone/EtOH 9:1 (v/v). The resulting films were hard, brittle and did not disperse in water. It has been reported that the properties of films cast from organic solvents may change by varying the composition of solvent mixtures even though the composition of the dried films is the same [52–56]. Using this approach, we found, surprisingly, that addition of EtOH (final concentrations 50 to 65%) to the casting solvents ethyl acetate, CH3COOH and acetone, respectively, resulted in films with dramatically altered properties. They were soft, flexible, and dispersed in water, resulting ultimately in smooth gels. The properties of a selected film (designated "H') consisting of 40% CAP, 40% HPC and 20% glycerol cast from acetone/EtOH 4:6 are described here.
Physical properties of CAP-HPC film H
Scanning electron microscopy of film H (thickness ≈100 µ) revealed a particle-accumulated layer on one side (A; exposed to air during drying) of the film (Fig. 1a) while the other side was more smooth (results not shown). Side A of the film was textured with alternating protrusions and depressions having a lateral dimension of ≈1 µ. The 3-dimensional interactive display of both sides of the film (Fig. 1b,1c), analogous to a geographic map showing peaks and valleys, provides a 3-dimensional image of the film. It covers a larger representative surface of the film than does Fig. 1a, and clearly indicates that the surface of the film is not smooth. This is important for the virus inactivating properties of the film before it disintegrates, since the effectiveness of the film in this regard depends on its total surface area accessible to bind viruses or other pathogens. This area is much larger for a film with elevations and depressions (which can accommodate virus particles) as compared with a film which is "truly" flat. Exposure of the film to water resulted in disintegration and formation of smaller particles ultimately convertible into a gel. Mixing of pieces of film in water at low speed resulted in generation of a smooth gel. The only method to measure objectively the kinetics of this transition is viscosimetry. The corresponding results are shown in Fig. 1d. The conversion to gel was faster in seminal fluid than in water. Scanning electron microscopy revealed particles of micronized CAP in the resulting gel (Fig. 1e). The particles had a size between 0.5 to 3 µ (Fig. 1f), similar to that of CAP particles in gel formulations which were shown to be efficacious against several STD pathogens in in vitro and in vivo experiments [7, 10–14, 47–49].
Microbicidal activities of CAP-HPC film
Micronized CAP was shown to inactivate within a few minutes the infectivity of HIV-1, HSV and several non-viral STD pathogens [7, 14]. CAP in micronized form is the only candidate topical microbicide having the capacity to remove rapidly by adsorption from physiological fluids HIV-1 of both the X4 and R5 biotypes and is likely to prevent virus contact with target cells [14]. The efficiency of adsorption is proportional to the total surface area of the adsorbent. For a given quantity of adsorbent the surface area is a function of particle size of the adsorbent, the total surface of the particles being inversely proportional to particle diameter, i.e. the smaller the particles, the larger is the total surface area of all particles. For this reason, it is desirable that the film disintegrates into the smallest particles possible.
It was of interest to determine whether film H, long before it completely disintegrates in the presence of water, and is converted into a gel, has effects similar to those of micronized CAP. Weighed film aliquots were added to suspension of the respective viruses. After incubation for 5 min at 37°C, the infectivity of the residual viruses was determined by serially diluting each virus preparation and adding the respective diluted samples to target cells. Virus production was assessed using a luminescence readout system. Film was not added to control virus preparations (for details see Methods section). Dose response curves (i.e. luminescence vs. virus dilution) for all film treated and control viruses are shown in Fig. 2. The percentages of virus inactivated by the film were calculated from calibration curves relating luminescence to dilutions of each control virus (=red curves for each virus; Fig. 2). At the highest dose of film (56 mg/ml) = 99% inactivation of HIV-1, HSV-1 and HSV-2 was observed within 5 min at 37°C (Fig. 2a,2b,2c,2d). Both HIV-1 IIIB and BaL, viruses utilizing distinct cellular coreceptors, CXCR4 and CCR5, respectively [12], were inactivated. As the film dose was reduced, the extent of virus inactivation diminished and was 89 ± 4, 82 ± 9, 99.7 ± 0.1, and 95 ± 2 % for HIV-1 IIIB, HIV-1 BaL, HSV-1 and HSV-2, respectively, at a dose of 7 mg/ml. The residual infectivity in all cases was recovered in supernatants after removing film and particles released from it by centrifugation, suggesting that only virus not adsorbed to the film material escaped inactivation. This was confirmed in separate experiments (data not shown). For comparison, the suggested unit dose of film as a microbicide is ≈ 1,000 mg. Furthermore, under in vivo conditions (when the virus concentrations are expected to be by one to four orders of magnitude lower than those used here under experimental conditions [57, 58], virus removal by adsorption onto the insoluble CAP would be expected to block the complex sequence of events leading to mucosal infection. This would be further augmented by the formation of "dead-end" HIV-1 gp41 six-helix bundles and stripping off of HIV-1 envelope glycoproteins resulting from virus contact with CAP [14].
Film H also inactivated several non-viral STD pathogens and bacteria associated with BV (Fig. 3). This effect can be attributed to low pH provided by CAP [7, 10], unlike the anti-HIV-1 and anti-HSV-1/-2 effects occurring at both acidic and neutral pH [7, 13, 14]. This is probably reflected in the diminishing activity of the film as its dose is decreased. While the residual infectivity of all organisms tested was = 0.1% for film doses = 75 mg/ml (= 27.7 mg/ml for Chlamydia trachomatis), smaller film doses were much less effective (notice the logarithmic scale of the ordinate). Gardnerella vaginalis appeared to be the most sensitive to CAP among all organisms tested. The dose effect was not seen for Haemophilus ducreyi, suggesting distinct mechanisms of CAP action on different bacteria.
Inactivation by film H of selected non-viral STD pathogens and bacteria associated with BV. The STD pathogens (Neisseria gonorrhoeae, Haemophilus ducreyi and Chlamydia trachomatis) and bacteria associated with BV (Gardnerella vaginalis, Mycoplasma capricolum and Mycoplasma hominis) were treated with graded quantities of film H for 5 min at 37°C. Note on the abscissa that film dosages for Chlamydia trachomatis were different from those used for the other bacteria.
Discussion
To the best of our knowledge, the CAP film is presently the first film formulation for a candidate microbicide after the failure of an N-9 containing contraceptive film in phase III clinical trials for efficacy against sexual transmission of HIV-1. The likelihood of genital lesions after vaginal application of this film has been reported [31, 59]. This has led to the misconception among some researchers in the microbicide field that films, rather than the film ingredients, are responsible for the untoward effects observed. In fact, undesirable proinflammatory effects induced by N-9 have been documented in in vitro experiments [60, 61] and in cervicovaginal lavages from women after application of an N-9 containing gel [60, 61]. Inflammatory responses induced by N-9 were seen in animal model experiments [62]{S. Hild personal communication} and in women after vaginal application of N-9 [32, 63, 64]. On the other hand, untoward effects have not been seen when CAP was used in in vitro [61] or animal model experiments [65] (S. Hild, personal communication). CAP based gels have received regulatory approval in the United Kingdom for phase I clinical trials based on the latter findings. Thus, there is a priori no reason to believe that CAP films will elicit undesirable effects.
Difficulties in applying the N-9 film have been reported anecdotically since the film appeared to stick to wet fingers. This does not seem to apply to CAP films. The optimization of CAP films in iterative human acceptance trials is expected to obviate problems of this kind.
The CAP-HPC composite film after contact with water or physiological fluids is progressively converted into a gel (Fig. 1d). Similar gels were shown earlier [7, 8, 12–14] to rapidly inactivate HIV-1, HSV and other STD pathogens. Upon contact with fluids containing STD pathogens, the film inactivated the respective viruses and/or bacteria rapidly, long before it was converted into a gel. Expected exposure to high sheer rates during physiological processes would result in more rapid disintegration and conversion of the film into a gel than shown in Fig. 1d. Tests in animal model systems and human clinical trials will be needed to determine whether the film is efficacious in vivo.
Similarly to CAP based gels [10], the CAP-HPC film was active against several bacteria associated with BV, known to increase susceptibility to HIV-1 infection [46]. Thus inserted CAP-HPC films might be candidates for treatment of BV.
In addition to their application as a topical microbicide the described bioadhesive CAP-HPC films could be useful for delivery of pharmaceuticals to mucosal surfaces, including oral and ophthalmic [66, 67] applications.
Scaling up the film production on continuous belts, the selection of optimal size, thickness, shapes, folding, and appropriate packaging of the films for distinct applications will require further studies.
The CAP-HPC composite can be dried from organic solvent mixtures containing EtOH (as described above) in physical forms other than a film, e.g. granules, combined with tablet disintegrants (Mannogem or Pharmaburst [SPI Pharma, Grand Haven, MI, USA]) and compressed into tablets. The tablets in contact with water disintegrate instantaneously and are subsequently converted into a smooth gel similar to that generated by the films (Fig. 1d). Such tablets extend the potential application of the CAP-HPC composite as a topical microbicide and drug delivery tool. In general, the described composite contributes to broadening the function of CAP from an enteric coating material to becoming a component of novel mucosal drug delivery systems with inherent anti-microbial properties.
Conclusions
Microbicidal gels are being widely considered and developed as tools to prevent the sexual transmission of HIV-1 and other STD pathogens. A CAP based gel for this purpose has been developed [7–14] and is advancing into phase 1 human clinical trials. Such gels require applicators for topical delivery. This adds to the cost of the final product and may cause disposal problems and environmental concerns. These disadvantages can be overcome by replacing the gels with unit dose biodegradable devices dispersible in physiological fluids. We describe here a novel method to produce composite films in which the active ingredient, CAP, is an integral structural component. The film absorbs water and disintegrates leading to the formation of micronized CAP particles which were shown to adsorb HIV-1 [14] and inactivate STD pathogens. The film is converted in contact with physiological fluids into a soft gel, thus obviating the need for delivery by applicators. The CAP-HPC composite film could be useful for delivery to mucosal surfaces of pharmaceuticals other than CAP. Combined with other excipients, the shredded composite film can be compressed into tablets which disintegrate instantaneously, providing an alternative microbicide and general drug delivery system.
Abbreviations
- CAP:
-
cellulose acetate phthalate
- HIV:
-
human immunodeficiency virus
- HSV:
-
herpes viruses
- STD:
-
sexually transmitted disease
- AIDS:
-
acquired immunodeficiency syndrome
- HPC:
-
hydroxypropyl cellulose
- EtOH:
-
ethanol
- ß-gal:
-
ß-galactosidase
- BV:
-
bacterial vaginosis.
References
Liao J, Ottenbrite RM: Biological effects of polymeric drugs. Controlled Drug Delivery. Edited by: ParkK. 1997, Washington,DC, American Chemical Society, 455-467.
Uglea CV, Panaitescu L: Synthetic polyanionic macromolecules with antiviral and antitumoral activity. Current Trends in Polymer Science. 1997, 2: 241-251.
Edited by: ChielliniE, SunamotoJ, MigliaresiC, OttenbriteRM and CohnD. 2001, Dordrecht, NL, Kluwer Academic/Plenum Publishers, 2001: Biomedical Polymers and Polymer Therapeutics, Proceedings of the Third International Symposium on Frontiers in Biomedical Polymers including Polymer Therapeutics: From Laboratory to Clinical Practice
Duncan R: The dawning era of polymer therapeutics. Nat Rev Drug Discov. 2003, 2: 347-360. 10.1038/nrd1088.
Kabanov AV, Okano T: Challenges in polymer therapeutics: State of the art and prospects of polymer drugs. Polymer drugs in the clinical stage. Edited by: MaedaH, KabanovA, KataokaK and OkanoT. 2003, New York, Kluwer Academic/Plenum Publishers, 1-27.
Stone A: Microbicides: A new apporach to preventing HIV and other sexually transmitted infections. Nat Rev Drug Discov. 2002, 1: 977-985. 10.1038/nrd959.
Neurath AR, Strick N, Li Y-Y, Lin K, Jiang S: Design of a "microbicide" for prevention of sexually transmitted diseases using "inactive" pharmaceutical excipients. Biologicals. 1999, 27: 11-21. 10.1006/biol.1998.0169.
Gyotoku T, Aurelian L, Neurath AR: Cellulose acetate phthalate (CAP): an 'inactive' pharmaceutical excipient with antiviral activity in the mouse model of genital herpesvirus infection. Antiviral Chem Chemother. 1999, 10: 327-332.
Manson KH, Wyand MS, Miller C, Neurath AR: The effect of a cellulose acetate phthalate topical cream on vaginal transmission of simian immunodeficiency virus in rhesus monkeys. Antimicrob Agents Chemother. 2000, 44: 3199-3202. 10.1128/AAC.44.11.3199-3202.2000.
Neurath AR, Li Y-Y, Mandeville R, Richard L: In vitro activity of a cellulose acetate phthalate topical cream against organisms associated with bacterial vaginosis. J Antimicrob Chemother. 2000, 45: 713-714. 10.1093/jac/45.5.713.
Kawamura T, Cohen SS, Borris DL, Aquilino EA, Glushakova S, Margolis LB, Orenstein JM, Offord RE, Neurath AR, Blauvelt A: Candidate microbicides block HIV-1 infection of human immature Langerhans cells within epithelial tissue explants. J Exp Med. 2000, 192: 1491-1500. 10.1084/jem.192.10.1491.
Neurath AR, Strick N, Li Y-Y, Debnath AK: Cellulose acetate phthalate, a common pharmaceutical excipient, inactivates HIV-1 and blocks the coreceptor binding site on the virus envelope glycoprotein gp120. BMC Infect Dis. 2001, 1: 17-10.1186/1471-2334-1-17.
Neurath AR, Strick N, Jiang S, Li YY, Debnath AK: Anti-HIV-1 activity of cellulose acetate phthalate: Synergy with soluble CD4 and induction of "dead-end" gp41 six-helix bundles. BMC Infect Dis. 2002, 2: 6-10.1186/1471-2334-2-6.
Neurath AR, Strick N, Li Y-Y: Anti-HIV-1 activity of anionic polymers: A comparative study of candidate microbicides. BMC Infect Dis. 2002, 2: 27-10.1186/1471-2334-2-27.
Goskonda SR, Lee JC: Cellulose Acetate Phthalate. Handbook of Pharmaceutical Excipients. Edited by: KibbeAH. 2000, Washington, D.C./London,U.K., American Pharmaceutical Association/Pharmaceutical Press, 99-101. 3
Banker GS: Pharmaceutical coating composition, and preparation and dosages so coated. US Patent 4,330,338 issued May 18 1982
McGinley EJ, Tuason DC Jr: Enteric coating for pharmaceutical dosage forms. US Patent 4,518,433 issued May 21 1985
McGinley EJ: Enteric coating for pharmaceutical dosage forms. European Patent 0 111 103 issued September 20 1989
Wu SHW, Greene CJ, Sharma MK: Water-dispersible polymeric compositions. US Patent 4,960,814 issued October 2 1990
Wu SHW, Greene CJ, Sharma MK: Water-dispersible polymeric compositions. US Patent 5,025,004 issued June 18 1991
Sakellariou P, Rowe RC: Phase separation and morphology in ethylcellulose/cellulose acetate phthalate blends. J Applied Polymer Science. 1991, 43: 845-855. 10.1002/app.1991.070430502.
Ibrahim H, Bindschaedler C, Doelker E, Buri P, Gurny R: Aqueous nanodispersions prepared by a salting-out process. Int J Pharm. 1992, 87: 239-246. 10.1016/0378-5173(92)90248-Z.
Quintanar-Guerrero D, Allemann E, Fessi H, Doelker E: Pseudolatex preparation using a novel emulsion-diffusion process involving direct displacement of partially water-miscible solvents by distillation. Int J Pharm. 1999, 188: 155-164. 10.1016/S0378-5173(99)00216-1.
Yuan J, Wu SHW: Process for production of polymeric powders. US Patent 6,541,542 issued April 1 2003
Stiasny K, Koessl C, Heinz FX: Involvement of lipids in different steps of the flavivirus fusion mechanism. J Virol. 2003, 77: 7856-7862. 10.1128/JVI.77.14.7856-7862.2003.
Kietzke T, Neher D, Landfester K, Montenegro R, Guntner R, Scherf U: Novel approaches to polymer blends based on polymer nanoparticles. Nat Mater. 2003, 2: 408-412. 10.1038/nmat889.
Heusser J, Martin M: Pharmaceutical, vaginal applicable preparation and a process for its preparation. US Patent 5,380,529 issued January 10 1995
Meyers M: Use of edible film to prolong chewing gum shelf life. US Patent 5,409,715 issued April 25 1995
Staab R: Dissolvable device for contraception or delivery of medication. US Patent 5,529,782 issued June 25 1996
Thombre AG, Wigman LS: Rapidly disintegrating and fast-dissolving solid dosage form. US Patent 6,497,899 issued December 24 2002
Roddy RE, Zekeng L, Ryan KA, Tamoufe U, Weir SS, Wong EL: A controlled trial of nonoxynol 9 film to reduce male-to-female transmission of sexually transmitted diseases. N Engl J Med. 1998, 339: 504-510. 10.1056/NEJM199808203390803.
Van Damme L, Ramjee G, Alary M, Vuylsteke B, Chandeying V, Rees H, Sirivongrangson P, Mukenge-Tshibaka L, Ettiegne-Traore V, Uaheowitchai C, Abdool Karim SS, Masse B, Perriens J, Laga M: Effectiveness of COL-1492, a nonoxynol-9 vaginal gel, on HIV-1 transmission in female sex workers. The Lancet. 2002, 360: 971-977. 10.1016/S0140-6736(02)11079-8.
Green G, Pool R, Harrison S, Hart GJ, Wilkinson J, Nyanzi S, Whitworth JA: Female control of sexuality: illusion or reality? Use of vaginal products in south west Uganda. Soc Sci Med. 2001, 52: 585-598. 10.1016/S0277-9536(00)00162-3.
Jones DL, Weiss SM, Malow R, Ishii M, Devieux J, Stanley H, Cassells A, Tobin JN, Brondolo E, LaPerriere A, Efantis-Potter J, O'Sullivan MJ, Schneiderman N: A brief sexual barrier intervention for women living with AIDS: acceptability, use, and ethnicity. J Urban Health. 2001, 78: 593-604. 10.1093/jurban/78.4.593.
Mann JM, Tarantola DJM, Netter TW: AIDS in the World. Edited by: MannJM, TarantolaDJM and NetterTW. 1992, Cambridge, Harvard University Press
Perine PL: Sexually transmitted diseases in the tropics. Medical Journal of Australia. 1994, 160: 358-366.
HIV prevention through early detection and treatment of other sexually trasmitted diseases -- United States Recommendations of the Advisory Committee for HIV and STD Prevention. Mor Mort Wkly Rep. 1998, 47: 1-24.
Over M, Piot P: Human immunodeficiency virus infection and other sexually transmitted diseases in developing countries: public health importance and priorities for resource allocation. J Infect Dis. 1996, 174: S162-S175.
Rottingen JA, Cameron DW, Garnett GP: A systematic review of the epidemiologic interactions between classic sexually transmitted diseases and HIV: how much really is known?. Sex Transm Dis. 2001, 28: 579-597.
Coggins C, Segal S: AIDS and reproductive health. J Reprod Immunol. 1998, 41: 3-15. 10.1016/S0165-0378(98)00045-X.
Holmberg SD, Stewart JA, Gerber AR, Byers RH, Lee FK, O'Malley PM, Nahmias AJ: Prior herpes simplex virus type 2 infection as a risk factor for HIV infection. JAMA. 1988, 259: 1048-1050. 10.1001/jama.259.7.1048.
Reynolds SJ, Risbud AR, Shepherd ME, Zenilman JM, Brookmeyer RS, Paranjape RS, Divekar AD, Gangakhedkar RR, Ghate MV, Bollinger RC, Mehendale SM: Recent herpes simplex virus type 2 infection and the risk of human immunodeficiency virus type 1 acquisition in India. J Infect Dis. 2003, 187: 1513-1521. 10.1086/368357.
Ramjee G, Gouws E, Van Dyke E, Williams B, Karim SA: Herpes simplex virus type II infection is a risk factor for HIV seroconversion. Medical Research Council Policy Brief. 2002, Durban, South Africa, Medical Research Council
Gerbase AC, Rowley JT, Heymann DHL, Berkley SFB, Piot P: Global prevalence and incidence estimates of selected curable STDs. Sex Transm Dis. 1998, 74 (Suppl 1): S12-S16.
Nahmias AJ, Lee FK, Beckman-Nahmias S: Sero-epidemiological and -sociological patterns of herpes simplex virus infection in the world. Scand J Infect Dis Suppl. 1990, 69: 19-36.
Martin H.L.,Jr., Richardson BA, Nyange P, Lavreys L, Hillier SL, Chohan B, Mandaliya K, Ndinya-Achola JO, Bwayo J, Kreiss J: Vaginal lactobacilli, microbial flora, and risk of human immunodeficiency virus type 1 and sexually transmited disease acquisition. J Infect Dis. 1999, 180: 1863-1868. 10.1086/315127.
Neurath AR: A microbicide for prevention of sexually transmitted diseases using a pharmaceutical excipient. AIDS Patient Care STDS. 2000, 14: 215-219. 10.1089/108729100317830.
Neurath AR, Stick N, Li Y-Y, Radigan L, Jiang S: A microbicide for the third millenium (cellulose acetate phthalate). XIII International AIDS Conference. 2000, 713-717.
Neurath AR, Strick N: Quantitation of cellulose acetate phthalate in biological fluids as a complex with ruthenium red. Anal Biochem. 2001, 288: 102-104. 10.1006/abio.2000.4890.
Harwood RJ: Hydroxypropyl cellulose. Handbook of pharmaceutical excipients. Edited by: KibbeAH. 2000, Washington,DC; London,UK, American Pharmaceutical Association, Pharmaceutical Press, 244: 244-248. Third
Tambweker KR, Gunjan VK, Kandarapu R, Zaneveld LJD, Garg S: Effect of different bioadhesive polymers on performance characteristics of vaginal tablets. Microbicides 2002 Conference Abstract. 2002, 15:
Arwidsson H, Johansson B: Application of intrinsic-viscosity and interaction constant as a formulation tool for film coating. 3. Mechanical studies on free ethyl cellulose films, cast from organic-solvents. Int J Pharm. 1991, 76: 91-97. 10.1016/0378-5173(91)90347-Q.
Jones DS, Medlicott NJ: Casting solvent controlled release of chlorhexidine from ethyl cellulose films porepared by solvent evaporation. Int J Pharm. 1995, 114: 257-261. 10.1016/0378-5173(94)00240-6.
Rosilio V, Roblot-Treupel L, De Lourdes Costa M, Baszkin A: Physicochemical characterization of ethyl cellulose drug-loaded cast films. J Control Release. 1988, 7: 171-180. 10.1016/0168-3659(88)90009-0.
Kovacs B, Nguyen VH, Racz I: Studies on drug film coatings. Part 2. Flexibiility of coatings. Acta Pharm Hungarica. 1985, 55: 205-211.
Vemba T, Gillard J, Roland M: Influence of solvents and plasticizers on the permeability and the rupture force of ethyl cellulose film coatings. Pharmaceutica Acta Helvetiae. 1980, 55: 65-71.
Dyer JR, Kazembe P, Vernazza PL, Gilliam BL, Maida M, Zimba D, Hoffman IF, Royce RA, Schock JL, Fiscus SA, Cohen MS, Eron J.J.,Jr.: High levels of human immunodeficiency virus type 1 in blood and semen of seropositive men in sub-Saharan Africa. J Infect Dis. 1998, 177: 1742-1746.
Chakraborty H, Sen PK, Helms RW, Vernazza PL, Fiscus SA, Eron JJ, Patterson BK, Coombs RW, Krieger JN, Cohen MS: Viral burden in genital secretions determines male-to-female sexual transmission of HIV-1: a probabilistic empiric model. AIDS. 2001, 15: 621-627. 10.1097/00002030-200103300-00012.
Rustomjee R, Abdool Karim A, Abdool Karim SS, Laga M, Stein Z: Phase 1 trial of nonoxynol-9 film among sex workers in South Africa. AIDS. 1999, 13: 1511-1515. 10.1097/00002030-199908200-00011.
Fichorova RN, Tucker LD, Anderson DJ: The molecular basis of nonoxynol-9-induced vaginal inflammation and its possible relevance to human immunodeficiency virus type 1 transmission. J Infect Dis. 2001, 184: 418-428. 10.1086/322047.
Fichorova RN, Zhou F, Spangler M, Strick N, Neurath AR: Effects of cellulose acetate phthalate on proinflammatory activation status of human cervicovaginal epithelial cells. Microbicides 2003 Conference Abstract. 2003, A49-
Milligan GN, Dudley KL, Bourne N, Reece A, Stanberry LR: Entry of inflammatory cells into the mouse vagina following application of candidate microbicides: Comparison of detergent-based and sulfated polymer-based agents. Sex Transm Dis. 2002, 29: 597-605.
Stafford MK, Ward H, Flanagan A, Rosenstein IJ, Taylor-Robinson D, Smith JR, Weber J, Kitchen VS: Safety study of nonoxynol-9 as a vaginal microbicide: evidence of adverse effects. J Acquir Immune Defic Syndr Hum Retrovirol. 1998, 17: 327-331.
Rosenstein IJ, Stafford MK, Kitchen VS, Ward H, Weber JN, Taylor-Robinson D: Effect on normal vaginal flora of three intravaginal microbicidal agents potentially active against human immunodeficiency virus type 1. J Infect Dis. 1998, 177: 1386-1390.
Ratterree M, Gettie A, Malenbaum S, Neurath AR, Blanchard J, Cheng-Mayer C: Safety, distribution and protective efficacy of CAP in vivo. Microbicides 2003 Conference Abstract. 2003, A48-
Gates KA, Grad H, Birek P, Lee PI: A new bioerodible polymer insert for the controlled release of metronidazole. Pharm Res. 1994, 11: 1605-1609. 10.1023/A:1018913921956.
Baeyens V, Kaltsatos V, Boisrame B, Fathi M, Gurny R: Evaluation of soluble Bioadhesive Ophthalmic Drug Inserts (BODI) for prolonged release of gentamicin: Lachrymal pharmacokinetics and ocular tolerance. J Ocul Pharmacol Ther. 1998, 14: 263-272.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2334/3/27/prepub
Acknowledgements
This study was supported by NIH grant (PO1 HD41761) and the Marilyn M. Simpson Charitable Trust and is dedicated to the memory of Dr. Maurice Cohen, in appreciation of his enthusiastic support of research on biodegradable devices. We thank Veronica Kuhlemann for preparation of the manuscript and Figures. Scanning electron microscopy experiments were done by Richard S. Brown, MVA, Inc., Norcross, Georgia, USA. CAP and the tablet disintegrants Mannogem and Pharmaburst were gifts from Eastman Chemical Company (Kingsport, Tennessee, USA), and SPI Pharma (Grand Haven, Michigan, USA), respectively. HeLa-CD4-LTR-ß-gal and MAGI-CCR5 cells were obtained from the AIDS Reagent and Reference Reagent Program (Rockville, Maryland, USA) contributed by Drs. M. Emerman and J. Overbaugh. HSV-1 vgCL5 was a gift from Dr. J. P. Weir.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing Interests
None declared.
Authors' contributions
ARN developed the concepts representing the basis of the manuscript and designed most experiments. NS contributed to the development of the film and tablets and carried out experiments other than infectivity assays. YYL did all the tissue culture work and viral and bacterial infectivity assays.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Neurath, A.R., Strick, N. & Li, YY. Water dispersible microbicidal cellulose acetate phthalate film. BMC Infect Dis 3, 27 (2003). https://doi.org/10.1186/1471-2334-3-27
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2334-3-27