Abstract
Background
Chronic alveolar hypoxia results in sustained arterial constriction, and increase in pulmonary vascular resistance leading to pulmonary artery hypertension (PAHT). The aim of this study was to investigate the effect of propofol and etomidate on pulmonary artery (PA) reactivity in chronically hypoxic (CH) rats, a model of pulmonary arterial hypertension (PAHT), in normoxic animals, and human PA.
Methods
CH rats were maintained 14 days at 380 mmHg pressure in a hypobaric chamber. Human tissue was retrieved from histological lung pieces from patients undergoing resection for carcinoma. Cumulative concentrations of anaesthetics were tested on isolated vascular rings precontracted with phenylephrine (PHE) or 100 mM KCl. Statistical comparisons were done by ANOVA, followed, when needed, by Student t tests with Bonferroni correction as post-hoc tests.
Results
In normoxic rat PA, maximal relaxation (Rmax) induced by etomidate and propofol was 101.3 ± 0.8% and 94.0 ± 2.3%, respectively, in KCl-precontracted rings, and 63.3 ± 9.7% and 46.1 ± 9.1%, respectively, in PHE-precontracted rings (n = 7). In KCl-precontracted human PA, Rmax was 84.7 ± 8.6 % and 66.5 ± 11.8%, for etomidate and propofol, respectively, and 154.2 ± 22.4 % and 51.6 ± 15.1 %, respectively, in PHE-precontracted human PA (n = 7). In CH rat PA, the relaxant effect of both anaesthetics was increased in PHE-precontracted and, for etomidate only, in KCl-precontracted PA. In aorta, CH induced no change in the relaxant effect of anaesthetics.
Conclusion
Propofol and etomidate have relaxant properties in PA from human and normoxic rat. The relaxant effect is specifically accentuated in PA from CH rat, mainly via an effect on the pharmacomechanical coupling. Etomidate appears to be more efficient than propofol at identical concentration, but, taking into account clinical concentrations, etomidate is less potent than propofol, which effect was in the range of clinical doses. Although these findings provide experimental support for the preferential use of etomidate for haemodynamic stability in patients suffering from PAHT, the clinical relevance of the observations requires further investigation.
Similar content being viewed by others
Background
Chronic hypoxia (CH) occurs in people living at high altitude and in children who suffer congenital heart disease with left to right shunt; it is also a main characteristic of chronic obstructive pulmonary disease, a major cause of death that affects a significant proportion of adults. Chronic alveolar hypoxia results in sustained arterial constriction, an increase in pulmonary vascular resistance leading to pulmonary artery hypertension (PAHT). At last, PAHT is responsible for right ventricular failure, which may end in death [1, 2]. Patients with PAHT may undergo anaesthesia, i. e., for cardiac surgery or heart catheterisation. During general anaesthesia of such patients, variations in cardiac and pulmonary flows may lead to dangerous increase or decrease of systemic or pulmonary pressures. Such variations during catheterism would make the procedure useless. It is then important to consider the effects of the anaesthetics on vascular responsiveness.
The effect of etomidate on vascular reactivity has been poorly investigated. Early clinical studies showed that anaesthesia with etomidate induces little or no change in both pulmonary and systemic arterial pressure [3, 4]. Murday et al. [5] had observed an increase in pulmonary vascular resistance and a decrease in systemic vascular resistance in patients undergoing cardiac surgery, whereas Shapiro et al evidenced a decrease in mean arterial pressure [6]. In experimental studies, etomidate has been shown to inhibit relaxant responses in canine pulmonary arteries [7]. Experiments on isolated rat lung indicated that etomidate is a direct pulmonary vasoconstrictor [8]. The effect of etomidate on systemic and pulmonary vasculature remains hence unclear.
Propofol has become a widely used general anaesthetic during the last decade and was studied in many clinical trials. However, its effect on pulmonary vasculature is unclear. In some clinical trial, propofol altered neither pulmonary mean arterial pressure nor pulmonary vascular resistance, though it decreased systemic vascular resistance [9], whereas in other studies it was shown to decrease both pulmonary arterial pressure and pulmonary arterial resistance [10]. Experimental studies on rats isolated lungs showed a direct vasodilatant effect of propofol [8], and a relaxant effect was also evidenced on rat isolated pulmonary arterial rings [11, 12]. By contrast, it has been shown in dogs and canine isolated pulmonary arterial rings that propofol potentiates phenylephrine-induced vasoconstriction [13, 14]. As for etomidate, the effect of propofol on pulmonary artery remains hence highly controversial.
Most of the experimental studies have been performed on normal arteries. However, PAHT is associated with morphological and functional changes of pulmonary artery, mainly hypertrophy and hyperplasia of smooth muscle cells, and altered vascular reactivity and Ca2+ homeostasis [15, 16]. These functional and morphological alterations have been noted both in small intralobar PA and in main PA, indicating that main PA can be used as a relevant model for the study of pulmonary vasomotricity in CH conditions [17–22]. We have hence assessed the effects of propofol and etomidate on main pulmonary artery reactivity of chronically hypoxic (CH) rats, a model of PAHT, versus normoxic rat and human isolated pulmonary arteries. Since chronic hypoxia has differential effects on the systemic versus the pulmonary vasculature, we compared the results obtained in rat pulmonary artery with those obtained in systemic thoracic vasculature, i. e., thoracic aorta, in order to determine if the changes in the effect of anaesthetics observed in pulmonary artery were specific.
Methods
Chronic hypoxia protocol
The animals used in this study were treated and sacrificed in accordance with national guidelines, and the protocol accepted by local animal experimentation committee. Male Wistar rats, 8–10 weeks old, were exposed to a simulated altitude of 5500 m (barometric pressure 380 mmHg) in a well-ventilated, temperature-controlled hypobaric chamber for 14 days, as previously described [23, 24]. Such a protocol is classically used to generate PAHT [18, 19, 25, 26]. In previous studies, our laboratory has characterized this model of hypobaric hypoxia-induced PAHT and shown that this protocol consistently increases mean pulmonary arterial pressure, vessel wall thickness and produces right ventricular hypertrophy evidenced by an increase in the ratio of right ventricle to left ventricle + septum weight (RV/LVS) [15, 23, 27–30]. Normoxic rats were kept under similar conditions but not in the hypobaric chamber.
Tissue preparation
Rat pulmonary arteries and aorta from normoxic and hypoxic animals were obtained as follows: for each experiment, a rat was killed by cervical dislocation. The heart and lungs were removed en-bloc, and the extrapulmonary artery and the thoracic part of the aorta were rapidly dissected out. From each specimen, 3 rings 3–4 mm in length were obtained from the main, left and right extrapulmonary artery, and 3 rings of similar length from the thoracic portion of the aorta.
Human bronchial rings were obtained from lung pieces collected for histological examination following resection for carcinoma. Specimens were selected from 7 patients for whom no sign of pulmonary hypertension appeared after pulmonary radiology and clinical examination. Patients were 60.6 ± 4.1 years old. Their lung function was within the normal range: mean forced expiratory volume in 1 second (FEV1) was 84.4 ± 6.4% of predicted values and mean partial O2 pressure was 83.7 ± 3.3 mm Hg. Quickly after resection, segments of pulmonary arteries (3rd to 5th generation; 3–5 mm in internal diameter) were carefully dissected from a macroscopically tumour-free part of each of the histological pieces and transferred to the laboratory in an ice-cold physiological saline solution. Segments were then cut into rings measuring about 4–5 mm in length for isometric contraction measurements. Use of human tissues was performed according to national guidelines, in compliance with the Helsinki Declaration. Since tissues were obtained incidentally to patient surgery and discarded by the histological pathologist, specific ethical approval of the protocol was not required by French laws.
Isometric tension measurement
Isometric tension was measured in intact, i. e., with endothelium, vessel rings that were mounted between two stainless steel clips in vertical 20 ml organ baths of a computerized isolated organ bath system (IOX, EMKA Technologies, Paris, France) previously described [15, 24]. Baths were filled with Krebs-Henseleit (KH) solution (composition given below) maintained at 37°C and bubbled with a 95% O2-5% CO2 gas mixture. The upper stainless clip was connected to an isometric force transducer (EMKA Technologies). Tissues were set at optimal length (Lo) by equilibration against a passive load of 1.5 g in rat aorta, normoxic human and rat pulmonary arteries, and 2.5 g in CH rat pulmonary arteries, as determined for these types of preparation in control experiments (data not shown).
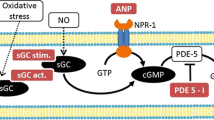
The relaxant effect of cumulative concentrations of etomidate and propofol on precontraction to phenylephrine and KCl was assessed as follows. At the beginning of each experiment, prior to exposure to anaesthetics, a contraction was elicited by either a hyperpotassic extracellular solution containing 100 mM KCl or 10-6 M phenylephrine (PHE). According to the Nernst equation, 100 mM KCl depolarises the membrane potential close to -10 mV, which opens the voltage-operated Ca2+ channels and thus activates the electromechanical coupling. PHE is an α1-adrenergic agonist that binds to G protein-coupled receptor and acts mainly via InsP3 production and Ca2+ release from intracellular stores, the so-called pharmacomechanical coupling.10-6 M PHE induces an inframaximal contractile response, as determined from a cumulative-concentration response curve to PHE in rat aorta and pulmonary artery (n = 4, data not shown). Upon KCl or PHE administration, when the maximal contraction was obtained, propofol or etomidate was added to the vessel rings in cumulative half-log increments from 10-6 to 10-3 M. The ring tension was measured when the response stabilized, i.e., after an equilibration time about 15 min, and expressed as a percentage of the maximal initial contraction of that ring. To avoid any bias due to time-dependent change in tension, the anaesthetic-induced relaxation was normalized to a paired temporal ring, i.e., a ring experimented simultaneously in similar conditions but without exposure to the anaesthetics.
Chemicals and drugs
PHE were purchased from Sigma (Saint Quentin Fallavier, France). Propofol (Diprivan®, Zeneca laboratories, Cergy France) and etomidate (Hypnomidate®, Janssen laboratories, Boulogne Billancourt, France) were obtained from their clinically used presentations. We verified that the vehicle of each of the drugs had no effect per se on contractile responses up to the maximal concentration used in the present experiments, i. e., 1.65%. Normal KH solution contained (in mM): 118.4 NaCl, 4.7 KCl, 2.5 CaCl2.2H2O, 1.2 MgSO4.7H2O, 1.2 KH2PO4, 25.0 NaHCO3, 11.1 D-glucose, pH 7.4. For KCl-induced contraction, KCl was substituted to NaCl for the desired concentrations, in order to keep the osmotic pressure constant.
Analysis of results and statistics
The relaxation induced by each concentration of anaesthetic was expressed as a percentage of the contractile response of the paired temporal control. The concentration-dependent relaxation curves were then fitted by a non-linear Boltzman equation used to determine the concentrations of anaesthetics that reduced the maximal contraction by 50% (IC50) and by 30% (IC30), reported as negative logarithm (pIC50 and pIC30, respectively), according to Lovren and Triggle [31], and as we previously used in airways [24]. Rmax refers to the maximal relaxation obtained at the maximal anaesthetic concentration (10-3 M).
Each experimental condition was repeated on 6 to 9 different specimens. Data are given as mean ± SEM. Overall cumulative concentration-response curves in control, etomidate- and propofol-exposed rings were compared using ANOVA for repeated measurements. Comparison of pIC30, pIC50 and Rmax was done by ANOVA, followed, when needed, by Student t tests with Bonferroni correction as post-hoc tests. Statistical tests were performed using the SPSS® statistical software. Differences were considered significant when P < 0.05.
Results
Effect of etomidate and propofol on normoxic rat pulmonary arterial rings
Both etomidate and propofol significantly relaxed precontracted PA rings (figure 1). Overall comparison of the curves showed no difference in the effect of propofol versus etomidate in KCl- as well as in PHE-precontracted rings. The relaxant effect of both compounds was greater on KCl-precontracted PA rings, since pIC30, pIC50 and Rmax were significantly greater in KCl- than PHE-precontracted tissues (tables 1 and 2).
Relaxant effect of etomidate and propofol on normoxic rat pulmonary arterial rings. Abscissa: log concentration of anaesthetics (M). Ordinate: isometric contraction (% of the paired temporal control unexposed rings). Full circles: rings exposed to etomidate. Open circles: rings exposed to propofol. A: rings precontracted with 100 mM KCl. B: rings precontracted with 10 -6M PHE. Each symbol is mean value from 5 to 8 rats. Vertical bars are SEM. P > 0.05 (overall comparison of etomidate versus propofol).
Effect of etomidate and propofol on human pulmonary artery rings
Overall comparison of the curves showed that propofol and etomidate had a similar concentration-dependent relaxant effect, as shown in fig. 2, despite an apparent greater effect for the highest concentration of etomidate in PHE-precontracted rings. Comparison of human versus normoxic rat PA showed that, for both anaesthetics, Rmax was similar or higher in human PA. However, in KCl-precontracted rings, pIC30 and pIC50 were higher in rat PA (tables 1 and 2).
Relaxant effect of etomidate and propofol on human pulmonary arterial rings. Abscissa: log concentration of anaesthetics (M). Ordinate: isometric contraction (% of the paired temporal control unexposed rings). Full circles: rings exposed to etomidate. Open circles: rings exposed to propofol. A: rings precontracted with 100 mM KCl. B: rings precontracted with 10 -6M PHE. Each symbol is mean value from 7 specimens. Vertical bars are SEM. P > 0.05 (overall comparison of etomidate versus propofol).
Effect of etomidate and propofol on CH rat pulmonary arterial rings
Both etomidate and propofol significantly relaxed precontracted PA rings from chronically hypoxic rats (figure 3). Overall comparison of the curves showed no difference in the effect of propofol versus etomidate in KCl-precontracted rings, whereas etomidate was more potent than propofol in PHE-precontracted PA rings. In contrast with observations on normoxic PA, no significant difference was observed in Rmax and pIC30 between KCl- and PHE-precontracted tissues (tables 1 and 2). Comparison between results obtained in PA from normoxic and CH rats showed that in PHE-precontracted rings, Rmax, pIC30 and pIC50 were higher in CH tissues. In KCl-precontracted rings, though Rmax was greater in CH rings for both anaesthetics, the difference was significant only for etomidate, and no change was observed for pIC30 and pIC50 (tables 1 and 2).
Relaxant effect of etomidate and propofol on pulmonary arterial rings from chronically hypoxic rats. Abscissa: log concentration of anaesthetics (M). Ordinate: isometric contraction (% of the paired temporal control unexposed rings). Full circles: rings exposed to etomidate. Open circles: rings exposed to propofol. A: rings precontracted with 100 KCl. B: rings precontracted with 10-6M PHE. Each symbol is mean value from 5 to 8 rats. Vertical bars are SEM. # P < 0.05 (overall comparison of etomidate versus propofol).
Effect of etomidate and propofol on normoxic and CH rat thoracic aorta
In rings from normoxic rats, both propofol and etomidate had a significant relaxant effect on KCl-and PHE-precontracted aortic rings (figure 4). Overall comparison of the curves indicated that etomidate and propofol had a similar effect on KCl-precontracted aorta, but that etomidate was more potent than propofol in PHE-precontracted tissues. Comparisons of Rmax and pIC30 and pIC50 showed that the relaxant effect of propofol, but not of etomidate, was greater on KCl-precontracted rings (tables 1 and 2). In rings from CH rats, both propofol and etomidate had also a significant relaxant effect on KCl-and PHE-precontracted rings. Overall comparison of CCRC indicated that etomidate and propofol had a similar effect, whatever the contractant agonist. Comparison of Rmax, pIC30 and pIC50 between normoxic and CH aorta showed that the only difference observed was an increase in the maximal relaxation to propofol in PHE-precontracted CH aorta (tables 1 and 2).
Relaxant effect of etomidate and propofol on rat aorta rings. Left panel: aorta rings from normoxic rat. Right panel: aorta rings from CH rat CH Abscissa: log concentration of anaesthetics (M). Ordinate: isometric contraction (% of the paired temporal control unexposed rings). Full circles: rings exposed to etomidate. Open circles: rings exposed to propofol. A: rings precontracted with 100 mM KCl. B: rings precontracted with 10 -6M PHE. Each symbol is mean value from 5 to 8 rats. Vertical bars are SEM. # P < 0.05 (overall comparison of etomidate versus propofol).
Discussion
Our results show that propofol and etomidate display a concentration-dependent relaxant effect on pulmonary vasculature. The effect of propofol on PA observed in this study is in accordance with several experimental data that have shown a relaxant effect of propofol on PA [8, 11, 12] However, some studies have evidenced a contractant effect of propofol on PA [13, 14, 32, 33]. The discrepancy with our study may be due to species differences, since these studies, showing a contractant effect of propofol on PA, were performed in dogs or on canine isolated tissues, whereas we evidenced a relaxant effect of propofol in both rat and human PA. In pulmonary artery, etomidate appeared to have a similar or even greater relaxant effect than propofol. Again, this result is in disagreement with previous studies that have evidenced an antirelaxant effect of etomidate in canine pulmonary artery [34]. In addition to species or tissues differences, it should also be noticed that in these studies the experimental conditions differed from ours and focused on the possible effect of etomidate on relaxant agents, not contractant ones.
Comparison of the Rmax obtained in rat versus human pulmonary arteries indicates that both anaesthetics have similar or even greater maximal relaxant effect in human compared to rat tissues. However, it should be noticed that for etomidate as well as propofol, pIC30 and pIC50 were higher in rat than in human PA precontracted with KCl. This indicates that, though both anaesthetics have a relaxant effect on PA from both species, human PA is less sensitive than rat one to the effect of propofol and etomidate, suggesting small, if any, relaxant effect of etomidate and propofol on normoxic human pulmonary artery at clinical concentrations.
For the two anaesthetics tested, the relaxant effect was greater in CH versus normoxic tissues. Though experiments, for obvious ethical considerations, have not been performed in human tissues from CH hypoxic patients (CH been a usual counterindication for lung surgery), our results suggest that the effect of these anaesthetics on haemodynamics may be greater in patients suffering chronic hypoxia, especially on pulmonary haemodynamics. CH has different effects on systemic and pulmonary vasculature. It has been shown that hypoxia induces systemic vasorelaxation and CH does not induce morphological changes in systemic vasculature [35]. By contrast, hypoxia induces a specific vasoconstriction in pulmonary artery, and CH induces pulmonary hypertension and remodelling [15, 16, 36]. Our study showed that the enhanced relaxant effect of etomidate and propofol in tissues from CH animals is principally observed in pulmonary artery. This indicates that the changes in anaesthetic sensitivity are not due to chronic hypoxia per se, but specifically associated with the CH-induced pulmonary hypertension.
The enhanced effect of the anaesthetics was mainly observed on PHE-precontracted PA. Hence, the increased sensitivity of CH PA is mainly due to an enhanced effect of the anaesthetics on the pharmacomechanical coupling. This suggests that chronic hypoxia modifies the pharmacomechanical coupling of pulmonary artery, in agreement with previous findings on CH-induced calcium signalling in pulmonary arterial smooth muscle cells [15]. Since the pharmacomechanical coupling is activated not only by α-adrenergic stimulation but also by several major physiological vasoactive agonists such as endothelin 1 and angiotensin 2, it is likely that propofol and etomidate may alter the physiological regulation of the pulmonary vasomotricity. Several authors have described an endothelium-dependent effect of propofol and etomidate on pulmonary vascular resistance [32, 34]. Since our experiments were performed in rings with intact endothelium, we cannot exclude that the enhanced relaxant effect of these anaesthetics on pulmonary arteries from CH rats may be endothelium-mediated. However, the endothelium-dependent effect of these anaesthetics have been evidenced on ACh-induced relaxation, whereas the effect of propofol and etomidate on pulmonary arteries stimulated by contractile agonists has been shown to be endothelium-independent [8, 11, 13, 14, 32, 34]. In particular, the effect of propofol, which was shown to be epithelium-dependent when assessed on ACh-induced relaxation [32], appeared to be epithelium-independent when tested on α-adrenergic contraction [11, 14], though with opposite consequence in dogs [14] and rats [11], as mentioned above. Since the enhanced effect of both anaesthetics were mainly observed on phenylephrine-precontracted rings, it is therefore likely that this effect may be endothelium-independent.
Though pulmonary artery and aorta rings used in this study were from chronically hypoxic animals, the experimental conditions for isometric measurements were not hypoxic, rather hyperoxic, since tissues were bubbled with 95% O2 and 5% CO2. Since anesthetized patients are usually ventilated with hyperoxic gas mixture, our experimental conditions remain, nevertheless, clinically relevant.
Blood concentrations of propofol and etomidate, following clinical injection, are about 3–15 μg.mL-1 and 0.5–1,6 μg.mL-1, respectively [37–41]. This corresponds to 10-5-10-4 M for propofol concentration, and about 2–6.10-6 M for etomidate. At these concentrations, below IC30 values, etomidate has no significant relaxant effect in normoxic tissues and, though enhanced, small effect on CH ones. This may explain why clinical studies have generally not concluded to a relaxant effect of etomidate on PA [5, 8], and suggests a small, if any, effect of etomidate on pulmonary haemodynamics in CH patients. By contrast, clinical concentrations of propofol may be in the same range of IC30 values. This may explain why some authors have concluded that propofol infusion at clinical doses decreases pulmonary arterial pressure and pulmonary arterial resistances [10]. Moreover, since the relaxant effect was increased in CH rat pulmonary arteries, the effect of propofol on pulmonary haemodynamics may be higher in CH subjects. Hence, our study provides experimental support for the preferential use of etomidate for the maintenance of haemodynamic stability in patients suffering from PAHT. However, one should be cautious in extrapolating ex vivo data to in vivo conditions, in particular because of the high protein binding of these compounds which decreases their free concentrations and hence their biological effect [42].
Conclusion
In conclusion, our study demonstrates that in normoxic rats etomidate and propofol have a relaxant effect on pulmonary artery, acting mainly on the electromechanical coupling and, to a lesser degree, on the pharmacological coupling. A relaxant effect was also observed in human pulmonary artery, though human PA appears to be less sensitive to the anaesthetics than rat one. The effects of both anaesthetics were greater on PA from an animal model of hypoxia-induced pulmonary hypertension. This enhanced relaxant effect was specific to PA and was mainly seen on the pharmacomechanical coupling. Etomidate appears to be more efficient than propofol at identical concentration. However, comparison that take into account difference between etomidate and propofol concentrations used at clinical doses indicates that etomidate is less potent than propofol, which may have an effect on pulmonary haemodynamics, especially in subjects suffering CH and PAHT. Although these findings provide experimental support for the preferential use of etomidate in patients suffering from PAHT, the clinical relevance of the observations requires further investigation.
Abbreviations
- CCRC:
-
cumulative-concentration response curve
- HC:
-
chronic hypoxia
- IC50 :
-
concentration that reduces the maximal contraction by 50%
- IC30 :
-
concentration that reduces the maximal contraction by 30%
- KH:
-
Krebs-Henseleit
- PA:
-
pulmonary artery
- PHE:
-
phenylephrine
- pIC50 :
-
negative logarithm of IC50
- pIC30 :
-
negative logarithm of IC30
- Rmax :
-
maximal apparent relaxation
References
Klinger JR, Hill NS: Right ventricular dysfunction in chronic obstructive pulmonary disease. Evaluation and management. Chest. 1991, 99: 715-723.
Pierson DJ: Pathophysiology and clinical effects of chronic hypoxia. Respir Care. 2000, 45: 39-51.
Criado A, Maseda J, Navarro E, Escarpa A, Avello F: Induction of anaesthesia with etomidate: haemodynamic study of 36 patients. Br J Anaesth. 1980, 52: 803-806.
Colvin MP, Savege TM, Newland PE, Weaver EJ, Waters AF, Brookes JM, Inniss R: Cardiorespiratory changes following induction of anaesthesia with etomidate in patients with cardiac disease. Br J Anaesth. 1979, 51: 551-556.
Murday HK, Hack G, Hermanns E, Rudolph A: [Hemodynamic effects of an etomidate-flunitrazepam or midazolam- fentanyl combination for induction of anesthesia in patients with heart valve diseases]. Anasth Intensivther Notfallmed. 1985, 20: 175-178.
Shapiro BM, Wendling WW, Ammaturo FJ, Chen D, Pham PS, Furukawa S, Carlsson C: Vascular effects of etomidate administered for electroencephalographic burst suppression in humans. J Neurosurg Anesthesiol. 1998, 10: 231-236.
Sohn JT, Murray PA: Inhibitory effects of etomidate and ketamine on adenosine triphosphate-sensitive potassium channel relaxation in canine pulmonary artery. Anesthesiology. 2003, 98: 104-113. 10.1097/00000542-200301000-00019.
Rich GF, Roos CM, Anderson SM, Daugherty MO, Uncles DR: Direct effects of intravenous anesthetics on pulmonary vascular resistance in the isolated rat lung. Anesth Analg. 1994, 78: 961-966.
Williams GD, Jones TK, Hanson KA, Morray JP: The hemodynamic effects of propofol in children with congenital heart disease. Anesth Analg. 1999, 89: 1411-1416. 10.1097/00000539-199912000-00016.
Hammaren E, Hynynen M: Haemodynamic effects of propofol infusion for sedation after coronary artery surgery. Br J Anaesth. 1995, 75: 47-50.
Park WK, Lynch C, Johns RA: Effects of propofol and thiopental in isolated rat aorta and pulmonary artery. Anesthesiology. 1992, 77: 956-963.
Tanaka H, Yamanoue T, Kuroda M, Kawamoto M, Yuge O: Propofol relaxes extrapulmonary artery but not intrapulmonary artery through nitric oxide pathway. Hiroshima J Med Sci. 2001, 50: 61-64.
Kondo U, Kim SO, Nakayama M, Murray PA: Pulmonary vascular effects of propofol at baseline, during elevated vasomotor tone, and in response to sympathetic alpha- and beta-adrenoreceptor activation. Anesthesiology. 2001, 94: 815-823. 10.1097/00000542-200105000-00020.
Ogawa K, Tanaka S, Murray PA: Propofol potentiates phenylephrine-induced contraction via cyclooxygenase inhibition in pulmonary artery smooth muscle. Anesthesiology. 2001, 94: 833-839. 10.1097/00000542-200105000-00022.
Bonnet S, Belus A, Hyvelin JM, Roux E, Marthan R, Savineau JP: Effect of chronic hypoxia on agonist-induced tone and calcium signaling in rat pulmonary artery. Am J Physiol Lung Cell Mol Physiol. 2001, 281: L193-201.
Durmowicz AG, Stenmark KR: Mechanisms of structural remodeling in chronic pulmonary hypertension. Pediatr Rev. 1999, 20: e91-e102.
Jeffery TK, Wanstall JC: Comparison of pulmonary vascular function and structure in early and established hypoxic pulmonary hypertension in rats. Can J Physiol Pharmacol. 2001, 79: 227-237. 10.1139/cjpp-79-3-227.
Morecroft I, Heeley RP, Prentice HM, Kirk A, MacLean MR: 5-hydroxytryptamine receptors mediating contraction in human small muscular pulmonary arteries: importance of the 5-HT1B receptor. Br J Pharmacol. 1999, 128: 730-734. 10.1038/sj.bjp.0702841.
MacLean MR, Sweeney G, Baird M, McCulloch KM, Houslay M, Morecroft I: 5-Hydroxytryptamine receptors mediating vasoconstriction in pulmonary arteries from control and pulmonary hypertensive rats. Br J Pharmacol. 1996, 119: 917-930.
Rondelet B, Kerbaul F, Van Beneden R, Motte S, Fesler P, Hubloue I, Remmelink M, Brimioulle S, Salmon I, Ketelslegers JM, Naeije R: Signaling molecules in overcirculation-induced pulmonary hypertension in piglets: effects of sildenafil therapy. Circulation. 2004, 110: 2220-2225. 10.1161/01.CIR.0000143836.40431.F5.
Marcos E, Fadel E, Sanchez O, Humbert M, Dartevelle P, Simonneau G, Hamon M, Adnot S, Eddahibi S: Serotonin-induced smooth muscle hyperplasia in various forms of human pulmonary hypertension. Circ Res. 2004, 94: 1263-1270. 10.1161/01.RES.0000126847.27660.69.
Jeffery TK, Wanstall JC: Pulmonary vascular remodelling in hypoxic rats: effects of amlodipine, alone and with perindopril. Eur J Pharmacol. 2001, 416: 123-131. 10.1016/S0014-2999(01)00855-X.
Roux E, Duvert M, Marthan R: Combined effect of chronic hypoxia an in vitro exposure to gas pollutants on airway reactivity. Am J Physiol (Lung Cell Mol Physiol). 2002, 283: L628-35.
Ouedraogo N, Marthan R, Roux E: The effects of propofol and etomidate on airway contractility in chronically hypoxic rats. Anesth Analg. 2003, 96: 1035-1041. 10.1213/01.ANE.0000053236.52491.69.
Karamsetty MR, Klinger JR, Hill NS: Phytoestrogens restore nitric oxide-mediated relaxation in isolated pulmonary arteries from chronically hypoxic rats. J Pharmacol Exp Ther. 2001, 297: 968-974.
MacLean MR, Morecroft I: Increased contractile response to 5-hydroxytryptamine1-receptor stimulation in pulmonary arteries from chronic hypoxic rats: role of pharmacological synergy. Br J Pharmacol. 2001, 134: 614-620. 10.1038/sj.bjp.0704273.
Belouchi NE, Roux E, Savineau JP, Marthan R: Effect of chronic hypoxia on calcium signalling in airway smooth muscle cells. Eur Respir J. 1999, 14: 74-79. 10.1034/j.1399-3003.1999.14a13.x.
Bonnet S, Dubuis E, Vandier C, Martin S, Marthan R, Savineau JP: Reversal of chronic hypoxia-induced alterations in pulmonary artery smooth muscle electromechanical coupling upon air breathing. Cardiovasc Res. 2002, 53: 1019-1028. 10.1016/S0008-6363(01)00548-X.
Bonnet S, Dumas-de-La-Roque E, Begueret H, Marthan R, Fayon M, Dos Santos P, Savineau JP, Baulieu EE: Dehydroepiandrosterone (DHEA) prevents and reverses chronic hypoxic pulmonary hypertension. Proc Natl Acad Sci U S A. 2003, 100: 9488-9493. 10.1073/pnas.1633724100.
Pauvert O, Bonnet S, Rousseau E, Marthan R, Savineau JP: Sildenafil alters calcium signaling and vascular tone in pulmonary arteries from chronically hypoxic rats. Am J Physiol Lung Cell Mol Physiol. 2004, 287: L577-83. 10.1152/ajplung.00449.2003.
Lovren F, Triggle C: Nitric oxide and sodium nitroprusside-induced relaxation of the human umbilical artery. Br J Pharmacol. 2000, 131: 521-529. 10.1038/sj.bjp.0703588.
Kondo U, Kim SO, Murray PA: Propofol selectively attenuates endothelium-dependent pulmonary vasodilation in chronically instrumented dogs. Anesthesiology. 2000, 93: 437-446. 10.1097/00000542-200008000-00023.
Tanaka S, Kanaya N, Homma Y, Damron DS, Murray PA: Propofol increases pulmonary artery smooth muscle myofilament calcium sensitivity: role of protein kinase C. Anesthesiology. 2002, 97: 1557-1566. 10.1097/00000542-200212000-00031.
Ogawa K, Tanaka S, Murray PA: Inhibitory effects of etomidate and ketamine on endothelium-dependent relaxation in canine pulmonary artery. Anesthesiology. 2001, 94: 668-677. 10.1097/00000542-200104000-00022.
Hopkins N, McLoughlin P: The structural basis of pulmonary hypertension in chronic lung disease: remodelling, rarefaction or angiogenesis?. J Anat. 2002, 201: 335-348. 10.1046/j.1469-7580.2002.00096.x.
Welsh DJ, Peacock AJ, MacLean M, Harnett M: Chronic hypoxia induces constitutive p38 mitogen-activated protein kinase activity that correlates with enhanced cellular proliferation in fibroblasts from rat pulmonary but not systemic arteries. Am J Respir Crit Care Med. 2001, 164: 282-289.
Hamada H, Damron DS, Murray PA: Intravenous anesthetics attenuate phenylephrine-induced calcium oscillations in individual pulmonary artery smooth muscle cells. Anesthesiology. 1997, 87: 900-907. 10.1097/00000542-199710000-00025.
Gelissen HP, Epema AH, Henning RH, Krijnen HJ, Hennis PJ, den Hertog A: Inotropic effects of propofol, thiopental, midazolam, etomidate, and ketamine on isolated human atrial muscle. Anesthesiology. 1996, 84: 397-403. 10.1097/00000542-199602000-00019.
Esener Z, Sarihasan B, Guven H, Ustun E: Thiopentone and etomidate concentrations in maternal and umbilical plasma, and in colostrum. Br J Anaesth. 1992, 69: 586-588.
Shafer A, Doze VA, Shafer SL, White PF: Pharmacokinetics and pharmacodynamics of propofol infusions during general anesthesia. Anesthesiology. 1988, 69: 348-356.
Doenicke A, Loffler B, Kugler J, Suttmann H, Grote B: Plasma concentration and E.E.G. after various regimens of etomidate. Br J Anaesth. 1982, 54: 393-400.
Belouchi NE, Roux E, Savineau JP, Marthan R: Interaction of extracellular albumin and intravenous anaesthetics, etomidate and propofol, on calcium signalling in rat airway smooth muscle cells. Fundam Clin Pharmacol. 2000, 14: 395-400.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2253/6/2/prepub
Acknowledgements
The authors thank Dr. Patrick Berger, M.D., PhD, Associate Professor of Physiology, Dr. Hughes Begueret, M.D., Ph. D. Staff Specialist of Histology, and the "Service de Chirurgie Thoracique", C.H.U. de Bordeaux, France, for the supply of human tissues, and Mr. Pierre Téchoueyres for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
NO participated in the conception of the study and its design, the experiments in rat and human tissues, participated in the analysis of the data, carried out the statistical analysis, and helped the draft of the manuscript. BM participated in the experiments in rat tissues and the analysis of data. HC participated in the contractile experiments in rat and human tissues. RM participated in the design of the study and helped the draft of the manuscript. ER participated in the conception of the study and its design, helped in statistical analysis and drafted the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ouédraogo, N., Mounkaïla, B., Crevel, H. et al. Effect of propofol and etomidate on normoxic and chronically hypoxic pulmonary artery. BMC Anesthesiol 6, 2 (2006). https://doi.org/10.1186/1471-2253-6-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2253-6-2