Abstract
A significant number of women with migraine has to face the choice of reliable hormonal contraception during their fertile life. Combined hormonal contraceptives (CHCs) may be used in the majority of women with headache and migraine. However, they carry a small, but significant vascular risk, especially in migraine with aura (MA) and, eventually in migraine without aura (MO) with additional risk factors for stroke (smoking, hypertension, diabetes, hyperlipidemia and thrombophilia, age over 35 years). Guidelines recommend progestogen-only contraception as an alternative safer option because it does not seem to be associated with an increased risk of venous thromboembolism (VTE) and ischemic stroke.
Potentially, the maintenance of stable estrogen level by the administration of progestins in ovulation inhibiting dosages may have a positive influence of nociceptive threshold in women with migraine. Preliminary evidences based on headache diaries in migraineurs suggest that the progestin-only pill containing desogestrel 75 μg has a positive effect on the course of both MA and MO in the majority of women, reducing the number of days with migraine, the number of analgesics and the intensity of associated symptoms. Further prospective trials have to be performed to confirm that progestogen-only contraception may be a better option for the management of both migraine and birth control. Differences between MA and MO should also be taken into account in further studies.
Similar content being viewed by others
Introduction
Migraine is a disabling headache, characterized by moderate to severe head pain, usually accompanied by nausea, photophobia, phonophobia and osmophobia (migraine without aura, MO). In about 30% of patients migraine attacks are preceded by transient focal neurologic symptoms which are called aura (migraine with aura, MA). Migraine has a high socio-economical impact. In fact during migraine attacks most migraineurs reported severe impairment or the need of the bed rest and almost 40% of migraine patients have five or more headache days monthly [1]. The Global Burden of Disease survey 2010 (GBD) recently published showed that migraine is the seventh highest cause of disability in the world [2].
Review
In the last few years significant advance in the field of reversible hormonal methods has been achieved in order to maximize the benefits and to minimize the risks.
We believe it is relevant for clinical practice to briefly review in here potential vascular risks according to the category of migraine, with and without aura, and to the type of hormonal contraceptive option.
Epidemiology of migraine and combined hormonal contraceptive (CHC) use
Migraine affects about 18% of women and 6% of men in USA and Western Europe [3, 4] and its cumulative lifetime prevalence is 43% in women and 18% in men [5]. It is then mostly a female disorder, that it is active in particular during the fertile period of the women’ life with a peak of prevalence in their 20s and 30s [6]. The reproductive life is characterized by the need of reliable and convenient methods of contraception. Among the several forms of contraceptives available, hormonal contraceptives are the most popular reversible method, both in USA and Europe and the “Pill” is the most used [7–9]. Low dose [20 to 30 μg ethynil estradiol (EE2) per day] combined hormonal contraceptives (CHCs) have become the method of choice and the availability of new progestins (third- and fourth-generation) has allowed to achieve non-contraceptive benefits in comparison to older progestins (second – generation) [10]. CHCs are available in several regimens and routes of administration (oral, transdermal vaginal) in the attempt to improve tolerability, adherence and convenience of use [11]. Moreover, two new CHCs containing natural estradiol (E2), instead of EE2, have been introduced to increase safety and future developments are ongoing [12]. Interestingly, many gynecological conditions that are comorbid with migraine can be treated with CHCs. This enhances the likelihood of their use in migraine population [13]. The prescription of CHCs may have different effects on migraine with not univocal results because of many methodological limitations (diverse hormonal combinations, variable research settings, retrospective and/or cross-sectional designs, lack of a clear phenotyping of the headache according to IHS criteria, inadequate duration of observation) [14–16]. Historically, combined oral contraceptive (COCs) is the category best studied in migraineurs with an aggravation of migraine reported in 18-50% of cases, an improvement in 3-35% and no change in 39-65% [17]. A more recent cross-sectional study on a large population found that migraine is significantly associated with COCs assumption. Yet because of the design of the study it is not possible to define a causal relationship between exposure and disease [18]. Analysis on the different effect of the COCs on the two forms of migraine revealed that MA worsen more (56.4%) than MO (25.3%) [19]. Furthermore, women can present MA for the first time during the initiation of COCs [20]. During the last decade, a specific “window” of vulnerability triggered by the 7 days free hormone interval has been identified and the definition of hormonally-associated headaches (exogenous hormone-induced headache and estrogen-withdrawal headache) encompasses several patho-physiological mechanisms which are likely to explain nociceptive threshold in women [21, 22]. Strategies to minimize estrogen withdrawal at the time of expected bleeding or to stabilize circulating estrogen at lower concentration include, respectively, 1) to use transdermal E2 during the free interval of hormonal contraception [22] or to shorten the interval from 7 to 4 and even to 2 days [23, 24]; 2) to administer low dose COCs in extended/flexible regimens [25] or to use extended vaginal contraception [26].
Very recently, Mac Gregor [27] reviewed the effects of currently available contraceptive methods in the context of the risks and benefits for women with migraine and non-migraine headaches and concluded that for the majority of women with headache and migraine, the choice of contraception is unrestricted. Indeed, the contraceptive method is unlikely to have an impact on headache, whereas migraine deserves accurate diagnosis and recognition of the impact of different methods on such condition.
Vascular risks associated with CHCs and migraine
MA, and to a lesser extent also MO, may increase vascular risk, especially the risk for ischemic stroke in younger women [27–30]. Moreover, evidences that need to be corroborated by further studies suggest an association between MA and cardiac events, intracerebral hemorrhage, retinal vasculopathy and mortality [31]. Even though the association between migraine and stroke appears to be independent of other cardiovascular risk factors [32], the presence of some risk factors, such as smoking and/or COCs use or their combination, further increase risk [33]. MA is associated with a twofold increased risk of ischemic stroke but the absolute risk associated with CHC use is very low in healthy young women with no additional risk factors and mostly related to the estrogen dose [34]. In spite of the considerable advances in terms of safety and tolerability of CHCs in migraine sufferers [13], their use is still questioned especially in women with additional risk factors for stroke, including, smoking, hypertension, diabetes, hyperlipidemia and thrombophilia, age over 35 years [35]. New evidences [36–38] have warned clinicians on the use of CHCs and the risk of venous thromboembolism (VTE) which is likely to be dependent on the type of the progestin [RR 1.6–2.4 by using third- and fourth-generation CHCs (namely, desogestrel, gestodene norgestimate and drospirenone, respectively) in comparison with those containing LNG (second-generation)] and the total estrogenicity of CHCs [39, 40]. Even new routes (trandermal patch and vaginal ring) seem to be associated with an increased VTE risk, but data are contradictory [41–43]. Indeed, according to a statement very recently released [44] many factors contribute to VTE risk (e.g. age, duration of use, weight, family history) which makes epidemiological studies vulnerable to bias and confounders. In addition, the decision-making process should take into account non only the small VTE risk (absolute risk depending on the background prevalence rate between 2 to 8 per 10,000 users per year [45]) of the contraceptive method but also other elements such as efficacy, tolerability, additional health benefits, and acceptability which have to be discussed with the individual woman. In any case, it is essential to follow the appropriate guidelines by avoiding the prescription of CHCs to women at elevated risk for VTE. In the context of migraine and CHCs use, it is very important to remember that the World Health Organization Medical Eligibility Criteria for Contraceptive Use stated that MA at any age is an absolute contraindication to the use of COCs (WHO Category 4) [46]. The US/WHO MEC is more restrictive than the UK/WHO MEC as regard to MO, rating CHCs as a category 4 for any migraineur over age 35 [47]. That being so, the personal risk assessment should guide the prescription of CHCs in selected conditions. When there is the sole need of contraception, without the added benefits of a peculiar hormonal compound and/or combination, CHCs with the lower vascular risk or alternative methods for birth control should be considered.
Progestogen-only contraception: a class on its own
The progestin component of hormonal contraceptives accounts for most of their contraceptive effects (inhibition of ovulation, suppression of endometrial activity, thickening of cervical mucus). Progestin-only methods includes pills (the pill most used in Europe contains low doses of desogestrel), injectables [depot Medroxyprogesteroneacetate (DMPA)], implants (the most recent long-acting reversible contraception contains Etonogestrel single-rod implant for at least 3 years), and intrauterine devices (levonorgestrel for at least 5 years) [48]. By providing effective and reversible contraception, progestin-only contraception has many noncontraceptive health benefits including improvement in dysmenorrhea, menorrhagia, premenstrual syndrome, and anemia [49]. Indeed, there is a general reduction of the amount of menstrual bleeding but cycle control may be erratic, a feature that may influence acceptability [50–52]. Progestin-only methods are appropriate for women who cannot or should not take CHCs because they have some contraindications to estrogen use and therefore display a higher risk of VTE [35, 36]. The progestogen-only contraception is a safe alternative to CHCs and the avoidance of the estrogen component has many advantages not only for breastfeeding women but also for women with vascular diseases or risk factors for stroke [46, 47]. The use of progestin-only contraception is not associated with an increased risk of VTE compared with non-users of hormonal contraception [53]. In addition, progestin-only pills, injectables, or implants are not associated with increased risk of ischemic stroke according to a recent metanalysis (OR 0.96; 95% CI: 0.70-1.31) [54]. Since the 1-year prevalence rates for migraine in women are 11% for MO and 5% for MA, respectively [55], there is potentially a high number of women in whom CHCs may be contraindicated according to WHO guidelines and progestogen-only contraception may be safely used [35, 36].
Evidence of progestogen-only contraception in women with migraine
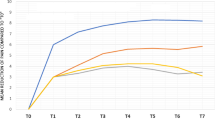
Given the evidence that progestogen-only contraception is a safer option for women with migraine, the main question is whether such contraceptive choice may influence the course of both MA and MO and offer a better management of the disease. Indeed, even though the excess risk of death for a woman taking modern CHCs is 1 in 100,000, which is much lower than the risk of everyday activities such as cycling [56], there is a biological plausibility that in women with migraine should be wiser to use an estrogen-free containing contraception to avoid any potential vascular risk. Two recent very large epidemiologic studies [36, 57] reported the association between CHC and progestogen-only methods and cardiovascular risk, thrombo-embolic risk and stroke. Whereas no increased risk for deep venous thormbosis, myocardial infarction and thrombotic stroke was found for the progestogen-only methods, the risk were two-sixfold elevated in CHC users. The role of progesterone/progestins in the pathophysiology of migraine has been overshadowed by Somerville’s early observations that it was the prevention of estrogen but not of progesterone withdrawal in the late phase of the cycle to be able to prevent the occurrence of migraine attacks [58, 59]. Indeed, at variance with the influence of estrogens upon the cerebral structures implicated in the pathophysiology of migraine [60], cyclic variations in progestin levels were not related to migrainous headaches, but they rather seem to be protective. Progesterone apparently attenuates trigemino-vascular nociception [61] and its receptors are localized in areas of the central nervous system, which are involved in neuronal excitability and neurotransmitter synthesis release and transport [62]. It has been shown that progesterone can antagonize neuronal estrogenic effects by downregulating estrogen receptors [63]. Whereas estrogen peak decrease the threshold for cortical spreading depression (CSD), the neurobiological event underlying MA, estrogen withdrawal increased the susceptibility to CSD in an animal model [64]. Therefore, the maintenance of low estrogen levels and the avoidance of estrogen withdrawal by the administration of progestins in ovulation inhibiting dosages might decrease cortical excitability. Indeed, progestogen-only contraception has a continuous administration, without the hormone-free interval, and does not induce withdrawal stabilizing circulating estrogens, but some fluctuations according to different preparations may still occur [65]. Clinical data are scarce and no comparative studies with progestogen-only contraceptives and placebo or COCs are available in the literature [27]. Diagnoses are often inaccurate, without distinction between headache and migraine, and headache is reported in contraceptive progestin implant users as a potential cause of discontinuation [66]. Similarly, there is an increase in headache, but not migraine, reported over time with both norethisterone enanthate and, especially with depot medroxyprogesterone acetate [67]. Anecdotally, migraine is more likely to improve in women who achieve amenorrhea [68]. In a large, cross-sectional, population-based study in Norway of 13944 women, a significant association between CHC and headaches, but no significant association between progestin-only pills and migraine (OR 1.3, 95% CI: 0.9–1.8) was found but the number of users was small [18]. To date two diary-based studies pilot studies on the effect of desogestrel 75 μg on migraine have been published [69, 70]. Such oral daily pill inhibits ovulation and the dose allows the ovary to synthesize stable amounts of estrogen which are relevant for wellbeing and bone density [71]. The first study included thirty women with MA [69]. The use of desogestrel 75 μg resulted in a significant reduction in MA attacks and in the duration of aura symptoms, already after three months of observation. Interestingly, the beneficial effect of desogestrel 75 μg on visual and other neurological symptoms of aura was significantly present only in those women in whom MA onset was related to previous COCs treatment. These findings suggest that the reduction in estrogen levels may be relevant to the amelioration of MA, but do not exclude a direct effect of the progestin on CSD. The second study on the effect of desogestrel 75 μg included women with MA (n°=6) and with MO (n°=32) and evaluated migraine days, pain score and pain medication [70]. An improvement of each parameter was observed during 3 months use of desogestrel 75 μg in comparison to a three months pretreatment interval. A subanalyses of the effect on 32 women with MO revealed significant improvements in number of migraine days, pain medication and pain intensity. The mean number of migraine attacks at baseline was higher in comparison to that in the study of Nappi et al. [69], indicating that also very severe migraineurs might profit from such a progestin-only contraception. Chronic migraineurs often develop medication overuse headaches with severe limitation of their quality of life. The reduction of pain medication by progestin-only contraception is an interesting approach and it should be studied further. Indeed, there is a broad variation in the intensity of improvement with a reduction in migraine frequency ranging from 20% and 100% [70]. No indicators to identify those women who will profit from desogestrel 75 μg could be ascertained. On the other hand, there were few dropouts of women experiencing more migraine after starting contraception with this progestin in both studies, indicating that progestins can also deteriorate migraine in few cases.
A very recent study investigating the changes of quality of life in migraineurs 3 months after initiation of the progestagen-only pill desogestrel 75 μg demonstrates a highly significant reduction in Midas Score and Midas grades [72]. However, clinical experience with desogestrel 75 μg in migraineurs further shows that during the initial 4 weeks migraine frequency can raise slightly before headaches improve. This information has to be mentioned and discussed during counseling.
In summary, the potential advantages of using progestogen-only contraception in women with migraine are the following:
-
1)
Continuous use
-
2)
Absence of estrogen peak
-
3)
No influence on threshold for cortical spreading depression (CDS)
-
4)
No evidence of increase in cardiovascular, stroke and thrombo-embolic risk
-
5)
No data on progestins inducing migraine
Conclusions
In conclusion, contraceptive counseling in migraine should take into account the risk-benefit profile of the individual woman before prescribing CHCs. In order to reduce potential vascular risks, recommendations should be a main point of guidance for prescribers. Progestogen-only contraception is a safer option in MA and eventually in MO with additional risk factors. Given preliminary evidences of a positive effect of the progestin-only pill desogestrel 75 μg on MA and MO in many, but not all women, further prospective trials have to be performed to confirm that progestogen-only contraception may be a better option for the management of both migraine and birth control. Differences between MA and MO should also be taken into account in further studies.
References
Bigal ME, Lipton RB: The epidemiology, burden, and comorbidities of migraine. Neurol Clin 2009, 27: 321–334. 10.1016/j.ncl.2008.11.011
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, et al.: Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380: 2163–2196. 10.1016/S0140-6736(12)61729-2
Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF, AMPP Advisory Group: Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 2007, 68: 343–349. 10.1212/01.wnl.0000252808.97649.21
Lj S, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, Steiner T, Zwart JA: The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 2007, 27: 193–210. 10.1111/j.1468-2982.2007.01288.x
Stewart WF, Wood C, Reed ML, Roy J, Lipton RB, AMPP Advisory Group: Cumulative lifetime migraine incidence in women and men. Cephalalgia 2008, 28: 1170–1178. 10.1111/j.1468-2982.2008.01666.x
Nappi RE, Berga SL: Migraine and reproductive life. Handb Clin Neurol 2010, 97: 303–322.
Mosher WD, Jones J: Use of contraception in the United States: 1982–2008. Vital Health Stat 2010,23(29):1–44.
Skouby SO: Contraceptive use and behavior in the 21st century: a comprehensive study across five European countries. Eur J Contracept Reprod Health Care 2010, 15: S42-S53. 10.3109/13625187.2010.533002
Johnson S, Pion C, Jennings V: Current methods and attitudes of women towards contraception in Europe and America. Reprod Health 2013, 10: 7. 10.1186/1742-4755-10-7
Maguire K, Westhoff C: The state of hormonal contraception today: established and emerging noncontraceptive health benefits. Am J Obstet Gynecol 2011, 205: S4-S8. 10.1016/j.ajog.2011.06.056
Shulman LP: The state of hormonal contraception today: benefits and risks of hormonal contraceptives: combined estrogen and progestin contraceptives. Am J Obstet Gynecol 2011, 205: S9-S13. 10.1016/j.ajog.2011.06.057
Sitruk-Ware R, Nath A, Mishell DR Jr: Contraception technology: past, present and future. Contraception 2013, 87: 319–330. 10.1016/j.contraception.2012.08.002
Calhoun A: Combined hormonal contraceptives: is it time to reassess their role in migraine? Headache 2012, 52: 648–660. 10.1111/j.1526-4610.2011.02051.x
Loder EW, Buse DC, Golub J: Headache and combination estrogen-progestin oral contraceptives: integrating evidence, guidelines, and clinical practice. Headache 2005, 45: 224–231. 10.1111/j.1526-4610.2005.05049.x
MacGregor EA: Migraine and use of combined hormonal contraceptives: a clinical review. J Fam Plann Reprod Health Care 2007, 33: 159–169. 10.1783/147118907781004750
Steenland MW, Zapata LB, Brahmi D, Marchbanks PA, Curtis KM: Appropriate follow up to detect potential adverse events after initiation of select contraceptive methods: a systematic review. Contraception 2013, 87: 611–624. 10.1016/j.contraception.2012.09.017
Massiou H, MacGregor EA: Evolution and treatment of migraine with oral contraceptives. Cephalalgia 2000, 20: 170–174. 10.1046/j.1468-2982.2000.00038.x
Aegidius K, Zwart JA, Hagen K, Schei B, Stovner LJ: Oral contraceptives and increased headache prevalence: the Head-HUNT Study. Neurology 2006, 66: 349–353. 10.1212/01.wnl.0000196481.57994.09
Granella F, Sances G, Pucci E, Nappi RE, Ghiotto N, Nappi G: Migraine with aura and reproductive life events: a case control study. Cephalalgia 2000, 20: 701–707.
Curtis KM, Chrisman CE, Peterson HB, WHO Programme for Mapping Best Practices in Reproductive Health: Contraception for women in selected circumstances. Obstet Gynecol 2002, 99: 1100–1112. 10.1016/S0029-7844(02)01984-1
Loder EW, Buse DC, Golub JR: Headache as a side effect of combination estrogen-progestin oral contraceptives: a systematic review. Am J Obstet Gynecol 2005, 193: 636–649. 10.1016/j.ajog.2004.12.089
Tassorelli C, Greco R, Allena M, Terreno E, Nappi RE: Transdermal hormonal therapy in perimenstrual migraine: why, when and how? Curr Pain Headache Rep 2012, 16: 467–473. 10.1007/s11916-012-0293-8
De Leo V, Scolaro V, Musacchio MC, Di Sabatino A, Morgante G, Cianci A: Combined oral contraceptives in women with menstrual migraine without aura. Fertil Steril 2011, 96: 917–920. 10.1016/j.fertnstert.2011.07.1089
Nappi RE, Terreno E, Sances G, Martini E, Tonani S, Santamaria V, Tassorelli C, Spinillo A: Effect of a contraceptive pill containing estradiol valerate and dienogest (E2V/DNG) in women with menstrually-related migraine (MRM). Contraception 2013. Epub ahead of print 10.1016/j.contraception.2013.02.001
Sulak P, Willis S, Kuehl T, Coffee A, Clark J: Headaches and oral contraceptives: impact of eliminating the standard 7-day placebo interval. Headache 2007, 47: 27–37.
Calhoun A, Ford S, Pruitt A: The impact of extended-cycle vaginal ring contraception on migraine aura: a retrospective case series. Headache 2012, 52: 1246–1253. 10.1111/j.1526-4610.2012.02211.x
MacGregor EA: Contraception and headache. Headache 2013, 53: 247–276. 10.1111/head.12035
Etminan M, Takkouche B, Isorna FC, Samii A: Risk of ischaemic stroke in people with migraine: systematic review and meta-analysis of observational studies. BMJ 2005, 330: 63–65. 10.1136/bmj.38302.504063.8F
Schurks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T: Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ 2009, 339: b3914. 10.1136/bmj.b3914
Spector JT, Kahn SR, Jones MR, Jayakumar M, Dalal D, Nazarian S: Migraine headache and ischemic stroke risk: an updated meta-analysis. Am J Med 2010, 123: 612–624. 10.1016/j.amjmed.2009.12.021
Sacco S, Ricci S, Carolei A: Migraine and vascular diseases: a review of the evidence and potential implications for management. Cephalalgia 2012, 32: 785–795. 10.1177/0333102412451361
Scher AI, Terwindt GM, Picavet HS, Verschuren WM, Ferrari MD, Launer LJ: Cardiovascular risk factors and migraine: the GEM population-based study. Neurology 2005, 64: 614–620. 10.1212/01.WNL.0000151857.43225.49
Sacco S, Ricci S, Degan D, Carolei A: Migraine in women: the role of hormones and their impact on vascular diseases. J Headache Pain 2012, 13: 177–189. 10.1007/s10194-012-0424-y
Gillum LA, Mamidipudi SK, Johnston SC: Ischemic stroke risk with oral contraceptives: a meta-analysis. JAMA 2000, 284: 72–78. 10.1001/jama.284.1.72
Allais G, Gabellari IC, De Lorenzo C, Mana O, Benedetto C: Oral contraceptives in migraine. Expert Rev Neurother 2009, 9: 381–393. 10.1586/14737175.9.3.381
Lidegaard Ø, Løkkegaard E, Svendsen AL, Agger C: Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ 2009, 339: b2890. 10.1136/bmj.b2890
Lidegaard Ø, Nielsen LH, Skovlund CW, Skjeldestad FE, Løkkegaard E: Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001–9. BMJ 2011, 343: d6423. 10.1136/bmj.d6423
Lidegaard O, Nielsen LH, Skovlund CW, Løkkegaard E: Venous thrombosis in users of non-oral hormonal contraception: follow-up study. Denmark 2001–10 2012, 344: e2990.
Sitruk-Ware R: Pharmacological profile of progestins. Maturitas 2008, 61: 151–157. 10.1016/j.maturitas.2008.11.011
Tchaikovski SN, Rosing J: Mechanisms of estrogen-induced venous thromboembolism. Thromb Res 2010, 126: 5–11. 10.1016/j.thromres.2010.01.045
Dinger JC, Heinemann LAJ, Kuhl-Habich D: The safety of a drospirenone-containing oral contraceptive: final results from the European Active Surveillance Study on Oral Contraceptives based on 142,475 women-years of observation. Contraception 2007, 75: 344–354. 10.1016/j.contraception.2006.12.019
Dinger J, Pineda AA: Risk of VTE in users of an etonogestrel-containing vaginal ring combined oral contraceptives. Abstract presented at the 60th Annual Clinical Meeting of the American College of Obstetricians and Gynecologists (ACOG). San Diego, CA, USA; 2012.
Sidney S, Cheetam TC, Connel FA, Ouellet-Hellstrom R, Graham DJ, Davis D, Sorel M, Quesenberry CP Jr, Cooper WO: Recent combined hormonal contraceptives (CHCs) and the risk of thromboembolism and other cardiovascular events in new users. Contraception 2013, 87: 93–100. 10.1016/j.contraception.2012.09.015
Bitzer J, Amy JJ, Beerthuizen R, Birkhäuser M, Bombas T, Creinin M, Darney PD, Vicente LF, Gemzell-Danielsson K, Imthurn B, Jensen JT, Kaunitz AM, Kubba A, Lech MM, Mansour D, Merki G, Rabe T, Sedlecki K, Serfaty D, Seydoux J, Shulman LP, Sitruk-Ware R, Skouby SO, Szarewski A, Trussell J, Westhoff C: Statement on combined hormonal contraceptives containing third- or fourth-generation progestogens or cyproterone acetate, and the associated risk of thromboembolism. Eur J Contracept Reprod Health Care 2013, 18: 143–147. 10.3109/13625187.2013.792637
Heinemann LAJ, Dinger JC: Range of published estimates of venous thromboembolism incidence in young women. Contraception 2007, 75: 328–336. 10.1016/j.contraception.2006.12.018
World Health Organization: Medical Eligibility for Contraceptive Use (4th edn). 2010.
Faculty of Sexual and Reproductive Healthcare: UK Medical Eligibility Criteria for Contraceptive Use – November 2009. Revised May 2010.
Burke AE: The state of hormonal contraception today: benefits and risks of hormonal contraceptives: progestin-only contraceptives. Am J Obstet Gynecol 2011, 205: S14-S17. 10.1016/j.ajog.2011.04.033
McCann MF, Potter LS: Progestin-only oral contraception: a comprehensive review. Contraception 1994, 50: S1-S195. 10.1016/0010-7824(94)90076-0
Collaborative Study Group on the Desogestrel-Containing Progestogen-Only Pill: A double-blind study comparing the contraceptive efficacy, acceptability and safety of two progestogen-only pills containing desogestrel 75 μg/day and levonorgestrel 30 μ/day. Eur J Contracep Reprod Health Care 1998, 3: 169–178. 10.3109/13625189809167250
Backman T: Benefit-risk assessment of the levonorgestrel intrauterine system in contraception. Drug Saf 2004, 27: 1185–1204. 10.2165/00002018-200427150-00003
Power J, French R, Cowan F: Subdermal implantable contraceptives versus other forms of reversible contraceptives or other implants as effective methods of preventing pregnancy. Cochrane Database Syst Rev 2007, CD001326.
Mantha S, Karp R, Raghavan V, Terrin N, Bauer KA, Zwicker JI: Assessing the risk of venous thromboembolic events in women taking progestin-only contraception: a meta-analysis. BMJ 2012, 345: e4944. 10.1136/bmj.e4944
Chakhtoura Z, Canonico M, Gompel A, Thalabard JC, Scarabin PY, Plu-Bureau G: Progestogen-only contraceptives and the risk of stroke: a metaanalysis. Stroke 2009, 40: 1059–1062. 10.1161/STROKEAHA.108.538405
Kelman L: The aura: a tertiary care study of 952 migraine patients. Cephalalgia 2004, 24: 728–734. 10.1111/j.1468-2982.2004.00748.x
Jensen JT, Trussell J: Communicating risk: does scientific debate compromise safety. Contraception 2012, 86: 327–329. 10.1016/j.contraception.2012.06.010
Lidegaard Ø, Løkkegaard E, Jensen A, Skovlund CW, Keiding N: Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 2012, 366: 2257–2266. 10.1056/NEJMoa1111840
Somerville BW: The role of estradiol withdrawal in the etiology of menstrual migraine. Neurology 1972, 22: 355–365. 10.1212/WNL.22.4.355
Somerville BW: Estrogen-withdrawal migraine. II. Attempted prophylaxis by continuous estradiol administration. Neurology 1972, 25: 245–250.
Greco R, Tassorelli C, Mangione AS, Smeraldi A, Allena M, Sandrini G, Nappi G, Nappi RE: Effect of sex and estrogens on neuronal activation in an animal model of migraine. Headache 2013, 53: 288–296. 10.1111/j.1526-4610.2012.02249.x
Bolay H, Berman NE, Akcali D: Sex-related differences in animal models of migraine headache. Headache 2011, 51: 891–904. 10.1111/j.1526-4610.2011.01903.x
Martin VT, Behbehani M: Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis–part i. Headache 2006, 46: 3–23. 10.1111/j.1526-4610.2006.00309.x
Jayaraman A, Pike CJ: Progesterone attenuates oestrogen neuroprotection via downregulation of oestrogen receptor expression in cultured neurones. J Neuroendocrinol 2009, 21: 77–81. 10.1111/j.1365-2826.2008.01801.x
Eikermann-Haerter K, Kudo C, Moskowitz MA: Cortical spreading depression and estrogen. Headache 2007, 47: S79-S85. 10.1111/j.1526-4610.2007.00818.x
Endrikat J, Gerlinger C, Richard S, Rosenbaum P, Düsterberg B: Ovulation inhibition doses of progestins: a systematic review of the available literature and of marketed preparations worldwide. Contraception 2011, 84: 549–557. 10.1016/j.contraception.2011.04.009
Glasier A: Implantable contraceptives for women: effectiveness, discontinuation rates, return of fertility, and outcome of pregnancies. Contraception 2002, 65: 29–37. 10.1016/S0010-7824(01)00284-0
Organization WH: Multinational comparative clinical evaluation of two long-acting injectable contraceptive steroids: noresthisterone oenanthate and medroxyprogesterone acetate. 2. Bleeding patterns and side effects. Contraception 1978, 17: 395–406. 10.1016/0010-7824(78)90001-X
Somerville B, Carey M: The use of continuous progestogen contraception in the treatment of migraine. Med J Aust 1970, 1: 1043–1045.
Nappi RE, Sances G, Allais G, Terreno E, Benedetto C, Vaccaro V, Polatti F, Facchinetti F: Effects of an estrogen-free, desogestrel-containing oral contraceptive in women with migraine with aura: a prospective diary-based pilot study. Contraception 2011, 83: 223–228. 10.1016/j.contraception.2010.07.024
Merki-Feld GS, Imthurn B, Langner R, Sandor PS, Gantenbein AR: Headache frequency and intensity in female migraineurs using desogestrel-only contraception: a retrospective pilot diary study. Cephalalgia 2013, 33: 340–346. 10.1177/0333102412473373
Rice C, Killick S, Hickling D, Coelingh Bennink H: Ovarian activity and vaginal bleeding patterns with a desogestrel-only preparation at three different doses. Hum Reprod 1996, 11: 737–740. 10.1093/oxfordjournals.humrep.a019245
Merki-Feld GS IB, Seifert B, Merki LL, Agosti R, Gantenbein AR: Desogestrel-only contraception reduces headache frequency and improves quality of life in female migraineurs. Eur J Contracep Reprod Health Care 2013. in press
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Dr. Rossella E. Nappi has had financial relationships (lecturer, member of advisory boards, and/or consultant) with Bayer Pharma, Eli Lilly, Gedeon Richter, HRA Pharma, MSD, Novo Nordisk, Pfizer Inc., Shionogi Limited, Teva/Theramex.
Dr. Gabriele S. Merki-Feld has had financial relationships (lecturer, member of advisory boards) with Bayer Pharma and MSD.
Authors’ contributions
Conception and design: REN, GSM. Acquisition of data: ET, AP. Analysis and interpretation of data: REN, MV, GSM. Drafting the article: REN, MV, GSM. Revising it for intellectual content: REN, MV, GSM. Final approval of the completed article: REN, REN, GSM, ET, AP, MV. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Nappi, R.E., Merki-Feld, G.S., Terreno, E. et al. Hormonal contraception in women with migraine: is progestogen-only contraception a better choice?. J Headache Pain 14, 66 (2013). https://doi.org/10.1186/1129-2377-14-66
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1129-2377-14-66