Abstract
Herein, we attempted to evaluate the therapeutic potential of photobiomodulation (PBM) and curcumin-loaded iron nanoparticles (CUR), alone and in combination, on wound closure rate (WCR), microbial flora by measuring colony-forming units (CFUs), the stereological and biomechanical properties of repairing wounds in the maturation stage of the wound healing course in an ischemic infected delayed healing wound model (IIDHWM) of type I diabetic (TIDM) rats. There were four groups: group 1 was the control, group 2 received CUR, rats in group 3 were exposed to PBM (80 Hz, 890 nm, and 0.2 J/cm2), and rats in group 4 received both PBM and CUR (PBM + CUR). We found CFU was decreased in groups 2, 3, and 4 compared to group 1 (p = 0.000 for all). Groups 2, 3, and 4 showed a considerable escalation in WCR compared to group 1 (p = 0.000 for all). In terms of wound strength parameters, substantial increases in bending stiffness and high-stress load were observed in groups 2, 3, and 4 compared to group 1 (p = 0.000 for all). Stereological examinations revealed decreases in neutrophil and macrophage counts and increases in fibroblast counts in groups 2, 3, and 4compared to group 1 (p = 0.000 for all). Blood vessel counts were more dominant in the PBM and PBM + CUR groups over group 1 (p = 0.000 for all). CFU and wound strength as well as macrophage, neutrophil, and fibroblast counts were found to be improved in the PBM + CUR and PBM groups compared to the CUR group (ranging from p = 0.000 to p < 0.05). Better results were achieved in the PBM + CUR treatment over the PBM therapy. We determined therapy with PBM + CUR, PBM alone, and CUR alone substantially accelerated diabetic wound healing in an IIDHWM of TIDM rats compared to control group. Concomitantly, the PBM + CUR and PBM groups attained significantly enhanced results for WCR, stereological parameters, and wound strength than the CUR group, with the PBM + CUR results being superior to those of the PBM group.
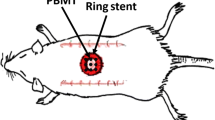
Graphical abstract









Similar content being viewed by others
Data availability statement
Statistical analysis of our work was available as a supplementary file.
References
Baynes, H. W. (2015). Classification, pathophysiology, diagnosis and management of diabetes mellitus. Journal of Diabetes Metabolism, 6(5), 1–9.
Gary Sibbald, R., & Woo, K. Y. (2008). The biology of chronic foot ulcers in persons with diabetes. Diabetes/metabolism research and reviews., 24(S1), S25–S30.
Steel, A., Reece, J., & Daw, A.-M. (2016). Understanding the relationship between depression and diabetic foot ulcers. Journal of Social Health and Diabetes., 4(01), 017–024.
Armstrong, D. G., Boulton, A. J. M., & Bus, S. A. (2017). Diabetic Foot Ulcers and Their Recurrence. New England Journal of Medicine, 376(24), 2367–2375.
Rastogi, A., Goyal, G., Rajesh Kesavan, R., Arun Bal, A., Mangalanadanam, K. H., et al. (2020). Long term outcomes after incident diabetic foot ulcer: multicenter large cohort prospective study (EDI-FOCUS investigators) epidemiology of diabetic foot complications study. Diabetes Research and Clinical Practice, 162, 108–113.
Demirdal, T., & Sen, P. (2018). The significance of neutrophil-lymphocyte ratio, platelet-lymphocyte ratio and lymphocyte-monocyte ratio in predicting peripheral arterial disease, peripheral neuropathy, osteomyelitis and amputation in diabetic foot infection. Diabetes research and clinical practice., 144, 118–125.
Weiss, U. (2008). Inflammation. Nature, 454(7203), 427.
Oliver, E., McGillicuddy, F., Phillips, C., Toomey, S., & Roche, H. M. (2010). The role of inflammation and macrophage accumulation in the development of obesity-induced type 2 diabetes mellitus and the possible therapeutic effects of long-chain n-3 PUFA. Proceedings of the Nutrition Society., 69(2), 232–243.
Nethi, S. K., Das, S., Patra, C. R., & Mukherjee, S. (2019). Recent advances in inorganic nanomaterials for wound-healing applications. Biomaterials science., 7(7), 2652–2674.
Chopra, H., Dey, P. S., Das, D., Bhattacharya, T., Shah, M., Mubin, S., et al. (2021). Curcumin nanoparticles as promising therapeutic agents for drug targets. Molecules, 26(16), 4998.
Karri, V. V. S. R., Kuppusamy, G., Talluri, S. V., Mannemala, S. S., Kollipara, R., Wadhwani, A. D., et al. (2016). Curcumin loaded chitosan nanoparticles impregnated into collagen-alginate scaffolds for diabetic wound healing. International journal of biological macromolecules., 93, 1519–1529.
Anand, P., Kunnumakkara, A. B., Newman, R. A., & Aggarwal, B. B. (2007). Bioavailability of curcumin: problems and promises. Molecular pharmaceutics., 4(6), 807–818.
Justin, C., Samrot, A. V., Sahithya, C. S., Bhavya, K. S., & Saipriya, C. (2018). Preparation, characterization and utilization of coreshell super paramagnetic iron oxide nanoparticles for curcumin delivery. PLoS ONE, 13(7), e0200440.
Naserzadeh, P., Hafez, A. A., Abdorahim, M., Abdollahifar, M. A., Shabani, R., Peirovi, H., et al. (2018). Curcumin loading potentiates the neuroprotective efficacy of Fe3O4 magnetic nanoparticles in cerebellum cells of schizophrenic rats. Biomedicine & Pharmacotherapy., 108, 1244–1252.
Moradi, A., Kheirollahkhani, Y., Fatahi, P., Abdollahifar, M.-A., Amini, A., Naserzadeh, P., et al. (2019). An improvement in acute wound healing in mice by the combined application of photobiomodulation and curcumin-loaded iron particles. Lasers in Medical Science., 34(4), 779–791.
Abhari, S. M. F., Khanbabaei, R., Roodbari, N. H., Parivar, K., & Yaghmaei, P. (2020). Curcumin-loaded super-paramagnetic iron oxide nanoparticle affects on apoptotic factors expression and histological changes in a prepubertal mouse model of polycystic ovary syndrome-induced by dehydroepiandrosterone-A molecular and stereological study. Life sciences., 249, 117515.
Saikia, C., Das, M. K., Ramteke, A., & Maji, T. K. (2016). Effect of crosslinker on drug delivery properties of curcumin loaded starch coated iron oxide nanoparticles. International journal of biological macromolecules., 93, 1121–1132.
Dayya, D., O’Neill, O., Habib, N., Moore, J., Iyer, K., & Huedo-Medina, T. B. (2022). Debridement of diabetic foot ulcers: public health and clinical implications–a systematic review, meta-analysis, and meta-regression. BMJ Surgery, Interventions, & Health Technologies. https://doi.org/10.1136/bmjsit-2021-000081.
Fard, A. S., Esmaelzadeh, M., & Larijani, B. (2007). Assessment and treatment of diabetic foot ulcer. International journal of clinical practice., 61(11), 1931–1938.
Carroll, L., & Humphreys, T. R. (2006). LASER-tissue interactions. Clinics in dermatology, 24(1), 2–7.
Avci, P., Gupta, A., Sadasivam, M., Vecchio, D., Pam, Z., Pam, N., et al. (2013). Low-level laser (light) therapy (LLLT) in skin: stimulating, healing, restoring. Seminars in cutaneous medicine and surgery. UK: NIH Public Access.
Oyebode, O., Houreld, N. N., & Abrahamse, H. (2021). Photobiomodulation in diabetic wound healing: A review of red and near-infrared wavelength applications. Cell Biochemistry and Function., 39(5), 596–612.
Mostafavinia, A., Masteri Farahani, R., Abdollahifar, M.-A., Ghatrehsamani, M., Ghoreishi, S. K., Hajihossainlou, B., et al. (2018). Evaluation of the effects of photobiomodulation on partial osteotomy in streptozotocin-induced diabetes in rats. Photomedicine and Laser Surgery., 36(8), 406–414.
Mostafavinia, A., Farahani, R. M., Abbasian, M., Farahani, M. V., Fridoni, M., Zandpazandi, S., et al. (2015). Effect of pulsed wave low-level laser therapy on tibial complete osteotomy model of fracture healing with an intramedullary fixation. Iranian Red Crescent Medical Journal. https://doi.org/10.5812/ircmj.32076.
Khosravipour, A., Amini, A., Farahani, R. M., Zare, F., Mostafavinia, A., Fallahnezhad, S., et al. (2020). Preconditioning adipose-derived stem cells with photobiomodulation significantly increased bone healing in a critical size femoral defect in rats. Biochemical and biophysical research communications., 531(2), 105–111.
Gazor, R., Asgari, M., Abdollajhifar, M.-A., Kiani, P., Zare, F., Fathabady, F. F., et al. (2021). Simultaneous treatment of photobiomodulation and demineralized bone matrix with adipose-derived stem cells improve bone healing in an osteoporotic bone defect. Journal of Lasers in Medical Sciences, 12(1), E41.
Asgari, M., Abdollahifar, M.-A., Gazor, R., Salmani, T., Khosravipour, A., Mahmoudi, Y., et al. (2022). Photobiomodulation and stem cell on repair of osteoporotic bones. Photobiomodulation, Photomedicine, and Laser Surgery., 40(4), 261–272.
Khosravipour, A., Mostafavinia, A., Amini, A., Gazor, R., Zare, F., Fallahnezhad, S., et al. (2022). Different protocols of combined application of photobiomodulation in vitro and in vivo plus adipose-derived stem cells improve the healing of bones in critical size defects in rat models. Journal of Lasers in Medical Sciences. https://doi.org/10.34172/jlms.2022.10.
Amini, A., Soleimani, H., Abdollhifar, M. A., Moradi, A., Ghoreishi, S. K., Chien, S., et al. (2019). Stereological and gene expression examinations on the combined effects of photobiomodulation and curcumin on wound healing in type one diabetic rats. Journal of cellular biochemistry., 120(10), 17994–18004.
Moradi, A., Kheirollahkhani, Y., Fatahi, P., Abdollahifar, M. A., Amini, A., Naserzadeh, P., et al. (2019). An improvement in acute wound healing in mice by the combined application of photobiomodulation and curcumin-loaded iron particles. Lasers in Medical Science, 34(4), 779–791.
Ebrahimpour-Malekshah, R., Amini, A., Zare, F., Mostafavinia, A., Davoody, S., Deravi, N., et al. (2020). Combined therapy of photobiomodulation and adipose-derived stem cells synergistically improve healing in an ischemic, infected and delayed healing wound model in rats with type 1 diabetes mellitus. BMJ Open Diabetes Research & Care. https://doi.org/10.1136/bmjdrc-2019-001033.
Kamar, S. S., Abdel-Kader, D. H., & Rashed, L. A. (2019). Beneficial effect of curcumin nanoparticles-hydrogel on excisional skin wound healing in type-i diabetic rat: histological and immunohistochemical studies. Annals of Anatomy—Anatomischer Anzeiger, 222, 94–102.
Karri, V. V., Kuppusamy, G., Talluri, S. V., Mannemala, S. S., Kollipara, R., Wadhwani, A. D., et al. (2016). Curcumin loaded chitosan nanoparticles impregnated into collagen-alginate scaffolds for diabetic wound healing. International Journal of Biological Macromolecules, 93(Pt B), 1519–1529.
Liu, J., Chen, Z., Wang, J., Li, R., Li, T., Chang, M., et al. (2018). Encapsulation of curcumin nanoparticles with MMP9-responsive and thermos-sensitive hydrogel improves diabetic wound healing. ACS Applied Materials and Interfaces., 10(19), 16315–16326.
Li, F., Shi, Y., Liang, J., & Zhao, L. (2019). Curcumin-loaded chitosan nanoparticles promote diabetic wound healing via attenuating inflammation in a diabetic rat model. Journal of biomaterials applications., 34(4), 476–486.
Taghavifar, S., Afroughi, F., & Saadati, K. M. (2022). Curcumin nanoparticles improved diabetic wounds infected with methicillin-resistant staphylococcus aureus sensitized with HAMLET. The International Journal of Lower Extremity Wounds., 21(2), 141–153.
Lee, S. Y., Jeon, S., Kwon, Y. W., Kwon, M., Kang, M. S., Seong, K. Y., et al. (2022). Combinatorial wound healing therapy using adhesive nanofibrous membrane equipped with wearable LED patches for photobiomodulation. Science Advances, 8(15), eabn1646.
Zaccaron, R. P., Barbieri, R. T., Mendes, C., Venturini, L. M., Alves, N., Mariano, S. S., et al. (2022). Photobiomodulation associated with lipid nanoparticles and hyaluronic acid accelerate the healing of excisional wounds. Journal of Biomaterials Applications., 15, 8853282221109344.
Lee, S. Y., Seong, I. W., Kim, J. S., Cheon, K. A., Gu, S. H., Kim, H. H., et al. (2011). Enhancement of cutaneous immune response to bacterial infection after low-level light therapy with 1072 nm infrared light: a preliminary study. Journal of Photochemistry and Photobiology B: Biology, 105(3), 175–182.
Karkada, G., Maiya, G. A., Houreld, N. N., Arany, P., Rao, K. G. M., Adiga, S., et al. (2020). Effect of photobiomodulation therapy on inflammatory cytokines in healing dynamics of diabetic wounds: a systematic review of preclinical studies. Archives of physiology and biochemistry. https://doi.org/10.1080/13813455.2020.1861025.
Moradi, A., Zare, F., Mostafavinia, A., Safaju, S., Shahbazi, A., Habibi, M., Abdollahifar, M. A., Hashemi, S. M., Amini, A., Ghoreishi, S. K., Chien, S., Hamblin, M. R., Kouhkheil, R., Bayat, M. (2020). Photobiomodulation plus adipose-derived stem cells improve healing of ischemic infected wounds in type 2 diabetic rats. Scientific Reports, 10(1), 1206. https://doi.org/10.1038/s41598-020-58099-z.
Kim, H., Kim, D. E., Han, G., Lim, N. R., Kim, E. H., Jang, Y., et al. (2022). Harnessing the natural healing power of colostrum: bovine milk-derived extracellular vesicles from colostrum facilitating the transition from inflammation to tissue regeneration for accelerating cutaneous wound healing. Advanced Healthcare Materials., 11(6), 2102027.
Glass, G. E. (2021). Photobiomodulation: a review of the molecular evidence for low level light therapy. Journal of Plastic, Reconstructive & Aesthetic Surgery., 74(5), 1050–1060.
Jere, S. W., Houreld, N. N., & Abrahamse, H. (2018). Photobiomodulation at 660nm stimulates proliferation and migration of diabetic wounded cells via the expression of epidermal growth factor and the JAK/STAT pathway. Journal of Photochemicals and Photobiology B., 179, 74–83.
Karkada, G., Maiya, G. A., Houreld, N. N., Arany, P., Rao Kg, M., Adiga, S., et al. (2020). Effect of photobiomodulation therapy on inflammatory cytokines in healing dynamics of diabetic wounds: a systematic review of preclinical studies. Archives of Physiology and Biochemistry., 23, 1–8.
Dadpay, M., Sharifian, Z., Bayat, M., Bayat, M., & Dabbagh, A. (2012). Effects of pulsed infra-red low level-laser irradiation on open skin wound healing of healthy and streptozotocin-induced diabetic rats by biomechanical evaluation. Journal of Photochemistry and Photobiology B: Biology., 111, 1–8.
Ma, H., Yang, J.-P., Tan, R. K., Lee, H.-W., & Han, S.-K. (2018). Effect of low-level laser therapy on proliferation and collagen synthesis of human fibroblasts in Vitro. Journal of wound management and research., 14(1), 1–6.
George, S., Hamblin, M. R., & Abrahamse, H. (2018). Effect of red light and near infrared laser on the generation of reactive oxygen species in primary dermal fibroblasts. Journal of Photochemistry and Photobiology B: Biology., 188, 60–68.
Skopin, M. D., & Molitor, S. C. (2009). Effects of near-infrared laser exposure in a cellular model of wound healing. Photodermatology, photoimmunology & photomedicine., 25(2), 75–80.
Zhu, Q., Xiao, S., Hua, Z., Yang, D., Hu, M., Zhu, Y.-T., et al. (2021). Near infrared (NIR) light therapy of eye diseases: A review. International Journal of Medical Sciences., 18(1), 109.
Ando, T., Xuan, W., Xu, T., Dai, T., Sharma, S. K., Kharkwal, G. B., et al. (2011). Comparison of therapeutic effects between pulsed and continuous wave 810-nm wavelength laser irradiation for traumatic brain injury in mice. PLoS ONE, 6(10), e26212.
Dai, T., Tegos, G. P., Zhiyentayev, T., Mylonakis, E., & Hamblin, M. R. (2010). Photodynamic therapy for methicillin-resistant Staphylococcus aureus infection in a mouse skin abrasion model. Lasers in Surgery and Medicine: The Official Journal of the American Society for Laser Medicine and Surgery., 42(1), 38–44.
Funding
Our research was economically supported by the Research Department of the medical faculty at SBMU (Grant No.: 30491, (IR.SBMU.MSP.REC.1400. 675,). This article was extracted from the thesis (IR.SBMU.AEC.1401.034) written by Mr. Hamidreza Omidi.
Author information
Authors and Affiliations
Contributions
MB wrote the manuscript. HO, KS, AM, HA, MM, FG, MA, and FR performed the experiments. AA, FF, LG, and SC added their comments. AM completed the statistical methods. All authors approved the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest.
Ethical approval
This investigation was permitted by the Clinical Morals office of SBMU (IR.SBMU.MSP.REC.1400. 675, and IR.SBMU.AEC.1401.034).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Omidi, H., Sohrabi, K., Amini, A. et al. Application of combined photobiomodulation and curcumin-loaded iron oxide nanoparticles considerably enhanced repair in an infected, delayed-repair wound model in diabetic rats compared to either treatment alone. Photochem Photobiol Sci 22, 1791–1807 (2023). https://doi.org/10.1007/s43630-023-00411-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43630-023-00411-7