Abstract
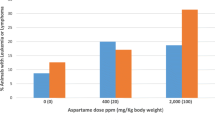
Liver cancer shows noticeable differences in the incidence rate and mortality between genders. To investigate the estrogen effect on tumor progression in liver cancer, we developed a xenograft model using estrogen pellets. SK-Hep1 cells (human male liver carcinoma) were inoculated into male or female nude mice. Subsequently, estrogen pellets were subcutaneously implanted into these xenograft models. Interestingly, the marked adverse effect of estrogen pellets (0.5 mg/21 days) were observed in the male-derived xenograft model, with increased ulcerative dermatitis in male mice than in female mice. Additionally, necrosis was observed in male mice with SK-Hep1-derived tumors. However, the estrogen pellet (0.5 mg/60 days) did not exhibit these adverse effects. Tumor growth in female mice was significantly suppressed by estrogen (0.5 mg/60 days). Tumor growth was also suppressed in male mice implanted with estrogen (0.5 mg/60 days), but the suppression was not significant. We found that estrogen-induced skin damage was more severe in male mice than female mice. The tumor suppression of estrogen was effective in female mice compared to male mice bearing liver cancer. The results suggest that the sex difference affects estrogen activity and thus should be considered in the preclinical assessment.



Similar content being viewed by others
Abbreviations
- ER:
-
Estrogen receptor
- E2:
-
Estrogen
- F:
-
Female
- M:
-
Male
References
Liu WC, Liu QY (2014) Molecular mechanisms of gender disparity in hepatitis B virus-associated hepatocellular carcinoma. World J Gastroenterol 20:6252–6261
Yang ST, Han JQ, Wang YD, Shen C, Zhao CY (2019) Estrogen and its receptors in hepatitis B virus-related hepatocellular carcinoma. Zhonghua gan zang bing za zhi Chin J Hepatol 27:232–235
Altekruse SF, Henley SJ, Cucinelli JE, McGlynn KA (2014) Changing hepatocellular carcinoma incidence and liver cancer mortality rates in the United States. Am J Gastroenterol 109:542–553
Kim BH, Park JW (2018) Epidemiology of liver cancer in South Korea. Clin Mol Hepatol 24:1–9
Li H, Lu JW, Huo X, Li Y, Li Z, Gong Z (2019) Effects of sex hormones on liver tumor progression and regression in Myc/xmrk double oncogene transgenic zebrafish. Gen Comp Endocrinol 277:112–121
Hassan MM, Botrus G, Abdel-Wahab R, Wolff RA, Li D, Tweardy D, Phan AT, Hawk E, Javle M, Lee JS, Torres HA, Rashid A, Lenzi R, Hassabo HM, Abaza Y, Shalaby AS, Lacin S, Morris J, Patt YZ, Amos CI, Khaderi SA, Goss JA, Jalal PK, Kaseb AO (2017) Estrogen replacement reduces risk and increases survival times of women with hepatocellular carcinoma. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 15:1791–1799
Casimiro MC, Wang C, Li Z, Di Sante G, Willmart NE, Addya S, Chen L, Liu Y, Lisanti MP, Pestell RG (2013) Cyclin D1 determines estrogen signaling in the mammary gland in vivo. Mol Endocrinol 27:1415–1428
Nilsson ME, Vandenput L, Tivesten A, Norlen AK, Lagerquist MK, Windahl SH, Borjesson AE, Farman HH, Poutanen M, Benrick A, Maliqueo M, Stener-Victorin E, Ryberg H, Ohlsson C (2015) Measurement of a comprehensive sex steroid profile in rodent serum by high-sensitive gas chromatography-tandem mass spectrometry. Endocrinology 156:2492–2502
Dall G, Vieusseux J, Unsworth A, Anderson R, Britt K (2015) Low dose, low cost estradiol pellets can support MCF-7 tumour growth in nude mice without bladder symptoms. J Cancer 6:1331–1336
Horii Y, Takei H, Koibuchi Y, Horiguchi J, Maemura M, Iino Y, Morishita Y (2006) The regulatory effect of tamoxifen on fibronectin expression in estrogen-dependent MCF-7 breast carcinoma cells. Oncol Rep 15:1191–1195
Suzuki Y, Ii M, Saito T, Terai Y, Tabata Y, Ohmichi M, Asahi M (2018) Establishment of a novel mouse xenograft model of human uterine leiomyoma. Sci Rep 8:8872
Kang JS, Kang MR, Han SB, Yoon WK, Kim JH, Lee TC, Lee CW, Lee KH, Lee K, Park SK, Kim HM (2009) Low dose estrogen supplementation reduces mortality of mice in estrogen-dependent human tumor xenograft model. Biol Pharm Bull 32:150–152
Massarweh S, Osborne CK, Creighton CJ, Qin L, Tsimelzon A, Huang S, Weiss H, Rimawi M, Schiff R (2008) Tamoxifen resistance in breast tumors is driven by growth factor receptor signaling with repression of classic estrogen receptor genomic function. Can Res 68:826–833
Gakhar G, Wight-Carter M, Andrews G, Olson S, Nguyen TA (2009) Hydronephrosis and urine retention in estrogen-implanted athymic nude mice. Vet Pathol 46:505–508
Pearse G, Frith J, Randall KJ, Klinowska T (2009) Urinary retention and cystitis associated with subcutaneous estradiol pellets in female nude mice. Toxicol Pathol 37:227–234
Gerard C, Gallez A, Dubois C, Drion P, Delahaut P, Quertemont E, Noel A, Pequeux C (2017) Accurate control of 17beta-estradiol long-term release increases reliability and reproducibility of preclinical animal studies. J Mammary Gland Biol Neoplasia 22:1–11
Liu P, Xie SH, Hu S, Cheng X, Gao T, Zhang C, Song Z (2017) Age-specific sex difference in the incidence of hepatocellular carcinoma in the United States. Oncotarget 8:68131–68137
Sukocheva OA (2018) Estrogen, estrogen receptors, and hepatocellular carcinoma: Are we there yet? World J Gastroenterol 24:1–4
Kuper H, Mantzoros C, Lagiou P, Tzonou A, Tamimi R, Mucci L, Benetou V, Spanos E, Stuver SO, Trichopoulos D (2001) Estrogens, testosterone and sex hormone binding globulin in relation to liver cancer in men. Oncology 60:355–360
Acknowledgements
This research was supported by the Bio & Medical Technology Development Program of the NRF funded by the Korean Government (2015M3A9B6074045) and the NRF Grant funded by the Korea government, MSIT (2017R1A2B4008254).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Oh, S., Choi, K., Kim, K.M. et al. Sex-dependent effects of estrogen pellets in human liver cancer xenograft models. Toxicol Res. 36, 109–114 (2020). https://doi.org/10.1007/s43188-019-00020-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43188-019-00020-6