Abstract
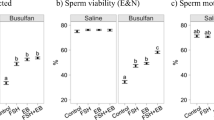
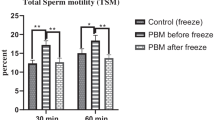
About 50% of infertility is caused by men. This study aimed to investigate the efficiency of photobiomodulation on spermatogenesis in a busulfan-induced infertile mouse as a testicular degeneration treatment. Thirty-two adult NMRI male mice were divided into 4 groups: control, busulfan, PBMT 0.03 J/cm2, and laser 0.2 J/cm2. In the study, azoospermia was induced by busulfan as a testicular degeneration, and then, they were treated using photobiomodulation therapy at 0.03 J/cm2 and 0.2 J/cm2 energy densities. Sperm parameters, stereological analysis, serum testosterone levels, together with SDH activity, MDA production oxidized as a marker for lipid peroxidation, glutathione (GSSG) and glutathione (GSH), mitochondrial membrane permeability (MMP), reactive oxygen species (ROS) production, and ATP production as well as TUNEL assay were assessed. Photobiomodulation therapy with 0.03 J/cm2 energy densities group revealed a significant increase the testosterone hormone level and spermatogenic cells with the reduction of apoptotic cells and marked increase in GSH, ATP, and SDH levels and decrease the levels of MDA and ROS production in the busulfan-induced mice when compared with the control and sham groups. In conclusion, the photobiomodulation therapy (0.03 J/cm2 energy density) may provide benefits on the spermatogenesis following busulfan injection and might be an alternative treatment to the patients with oligospermia and azoospermia in a dose-dependent manner.
Graphical abstract






Similar content being viewed by others
Availability of data and material
Data and material available on request
References
Kumar N, Singh AK. Trends of male factor infertility, an important cause of infertility: A review of literature. J Hum Reprod Sci. 2015;8(4):191–6. https://doi.org/10.4103/0974-1208.170370.
Dohle GR, Halley DJ, Van Hemel JO, et al. Genetic risk factors in infertile men with severe oligozoospermia and azoospermia. Hum Reprod. 2002;17:13–6. https://doi.org/10.1093/humrep/17.1.13.
Sarkar O, Bahrainwala J, Chandrasekaran S, Kothari S, Mathur PP, Agarwal A. Impact of inflammation on male fertility. Front Biosci (Elite Ed). 2011;1(3):89–95. https://doi.org/10.2741/e223.
Wosnitzer M, Goldstein M, Hardy MP. Review of azoospermia. Spermatogenesis. 2014;4(1):e28218.
Esteves SC, Ramasamy R, Colpi GM, Carvalho JF, Schlegel PN. Sperm retrieval rates by micro-TESE versus conventional TESE in men with non-obstructive azoospermia—the assumption of independence in effect sizes might lead to misleading conclusions. Hum Reprod Update. 2020;26:603–5.
Kirby EW, Wiener LE, Rajanahally S, Crowell K, Coward RM. Undergoing varicocele repair before assisted reproduction improves pregnancy rate and live birth rate in azoospermic and oligospermic men with a varicocele: a systematic review and meta-analysis. Fertil Steril. 2016;106(6):1338–43.
Bernie AM, Mata DA, Ramasamy R, Schlegel PN. Comparison of microdissection testicular sperm extraction, conventional testicular sperm extraction, and testicular sperm aspiration for nonobstructive azoospermia: a systematic review and meta-analysis. Fertil Steril. 2015;104(5):1099–103.e3.
Ahn J-C, Kim Y-H, Rhee C-K. The effects of low level laser therapy (LLLT) on the testis in elevating serum testosterone level in rats. 2013.
Moskvin SV, Apolikhin OI. Effectiveness of low level laser therapy for treating male infertility. BioMedicine. 2018;8(2).
Michael R. Hamblin. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys. 2017;4(3):337–61. https://doi.org/10.3934/biophy.2017.3.337.
Gabel CP, Carroll J, Harrison K. Sperm motility is enhanced by low level laser and light emitting diode photobiomodulation with a dose-dependent response and differential effects in fresh and frozen samples. Laser therapy. 2018;27(2):131–6.
Alves MBR, de Arruda RP, Batissaco L, Florez-Rodriguez SA, de Oliveira BMM, Torres MA, et al. Low-level laser therapy to recovery testicular degeneration in rams: effects on seminal characteristics, scrotal temperature, plasma testosterone concentration, and testes histopathology. Lasers Med Sci. 2016;31(4):695–704.
Dadras S, Abdollahifar M-A, Nazarian H, Ghoreishi SK, Fallahnezhad S, Naserzadeh P, et al. Photobiomodulation improved stereological parameters and sperm analysis factors in streptozotocin-induced type 1 diabetes mellitus. J Photochem Photobiol B Biol. 2018;186:81–7.
Ziaeipour S, Ahrabi B, Naserzadeh P, Aliaghaei A, Sajadi E, Abbaszadeh H, et al. Effects of Sertoli Cell Transplantation on Spermatogenesis in Azoospermic Mice. Cell Physiol Biochem. 2019;52(3):421–34.
Ziaeipour S, Ahrabi B, Naserzadeh P, Aliaghaei A, Sajadi E, Abbaszadeh H-A, et al. Effects of Sertoli cell transplantation on spermatogenesis in azoospermic mice. Cell Physiol Biochem. 2019;52:421–34.
Panahi S, Karamian A, Sajadi E, Aliaghaei A, Nazarian H, Abdi S, et al. Sertoli cell–conditioned medium restores spermatogenesis in azoospermic mouse testis. Cell Tissue Res. 2020;379(3):577–87.
Hasani A, Khosravi A, Rahimi K, Afshar A, Fathabadi FF, Raoofi A, et al. Photobiomodulation restores spermatogenesis in the transient scrotal hyperthermia-induced mice. Life Sci. 2020;117767.
Ayoubi M, Naserzadeh P, Hashemi MT, Rostami MR, Tamjid E, Tavakoli MM, et al. Biochemical mechanisms of dose-dependent cytotoxicity and ROS-mediated apoptosis induced by lead sulfide/graphene oxide quantum dots for potential bioimaging applications. Sci Rep. 2017;7(1):1–10.
Gundersen H, Bagger P, Bendtsen T, Evans S, Korbo L, Marcussen N, et al. The new stereological tools: disector, fractionator, nucleator and point sampled intercepts and their use in pathological research and diagnosis. Apmis. 1988;96(7-12):857–81.
Gundersen H, Bendtsen TF, Korbo L, Marcussen N, Møller A, Nielsen K, et al. Some new, simple and efficient stereological methods and their use in pathological research and diagnosis. Apmis. 1988;96(1-6):379–94.
Agarwal A, Saleh RA, Bedaiwy MA. Role of reactive oxygen species in the pathophysiology of human reproduction. Fertil Steril. 2003;79(4):829–43.
Bisht S, Dada R. Oxidative stress: Major executioner in disease pathology, role in sperm DNA damage and preventive strategies. Front Biosci (Schol Ed). 2017;9:420–47.
Zupin L, Pascolo L, Luppi S, Ottaviani G, Crovella S, Ricci G. Photobiomodulation therapy for male infertility. Lasers Med Sci. 2020;35(8):1671–80. https://doi.org/10.1007/s10103-020-03042-x.
Firestone RS, Esfandiari N, Moskovtsev SI, Burstein E, Videna GT, Librach C, et al. The effects of low-level laser light exposure on sperm motion characteristics and DNA damage. J Androl. 2012;33(3):469–73.
Salama N, El-Sawy M. Light-emitting diode exposure enhances sperm motility in men with and without asthenospermia: preliminary results. Archiv Ital Urol Androl. 2015;87(1):14–9.
Bermudez D, Carrasco F. Pérez de Vargas I. Effect of IR laser radiation on germ cell DNA content after one cycle of the seminiferous epithelium. Arch Androl. 1993;31(3):177–81.
Corral-Baqués M, Rigau T, Rivera M, Rodríguez J, Rigau J. Effect of 655-nm diode laser on dog sperm motility. Lasers Med Sci. 2005;20(1):28–34.
Preece D, Chow KW, Gomez-Godinez V, Gustafson K, Esener S, Ravida N, et al. Red light improves spermatozoa motility and does not induce oxidative DNA damage. Sci Rep. 2017;7:46480.
Hasan P, Sa R, Purnomo S, Kainama H. The possible application of low reactive-level laser therapy (LLLT) in the treatment of male infertility: a preliminary report. Laser Therapy. 2004;14(0_Pilot_Issue_2):0_65–6.
Piomboni P, Focarelli R, Stendardi A, Ferramosca A, Zara V. The role of mitochondria in energy production for human sperm motility. Int J Androl. 2012;35(2):109–24.
Ott M, Gogvadze V, Orrenius S, Zhivotovsky B. Mitochondria, oxidative stress and cell death. Apoptosis. 2007;12(5):913–22.
Szundi I, Liao G-L, Einarsdóttir Ó. Near-infrared time-resolved optical absorption studies of the reaction of fully reduced cytochrome c oxidase with dioxygen. Biochemistry. 2001;40(8):2332–9.
Drochioiu G. Laser-Induced ATP Formation: Mechanism and Consequences. Photomed Laser Surg. 2010;28(4):573–4.
Zhang H, Go Y-M, Jones DP. Mitochondrial thioredoxin-2/peroxiredoxin-3 system functions in parallel with mitochondrial GSH system in protection against oxidative stress. Arch Biochem Biophys. 2007;465(1):119–26.
Acknowledgments
This study is derived from the thesis formulated by Fatreh Rezaei, the MSc student at Department of Biology and Anatomical Sciences, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran (Registration No:15128).
Funding
This research was funded by the Laser Application in the Medical Science Research Center,Shahid Beheshti University of the Medical Sciences, Tehran, Iran (Grant number: 15128).
Author information
Authors and Affiliations
Contributions
MA. A designed this study. MA. A and F. R conducted the stereological study and drafted the manuscript. M. B carried out the Laser study. H. N carried out sperm analysis. F. R carried out the animal model and provided the clinical data, and sample. carried out the sperm analysis, molecular test, A. A and HA. A carried out the immunohistochemistry and Molecular test. P. N carried out the cellular analysis. A. A and V. E performed the statistical analysis and helped to write the draft of manuscript. A. A and S.A carried out the immunohistochemistry. S. A helped to designed this study and writing the draft of manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The experimental protocol and all procedures performed in studies involving the use of animals were reviewed and approved by the Ethical Committee at Shahid Beheshti University of
Medical Sciences (IR. SBMU. SM.REC. 1398.186).
Disclosure
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rezaei, F., Bayat, M., Nazarian, H. et al. Photobiomodulation Therapy Improves Spermatogenesis in Busulfan-Induced Infertile Mouse. Reprod. Sci. 28, 2789–2798 (2021). https://doi.org/10.1007/s43032-021-00557-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00557-8