Abstract
The development of immunoassays enables more sophisticated studies of the associations between protein concentrations and pregnancy outcomes, allowing early biomarker identification that can improve neonatal outcomes. The aim of this study was to explore associations between selected mid-trimester amniotic fluid proteins and (1) overall gestational duration and (2) spontaneous preterm delivery. A prospective cohort study, including women undergoing mid-trimester transabdominal genetic amniocentesis, was performed in Gothenburg, Sweden, 2008–2016 (n = 1072). A panel of 27 proteins related to inflammation was analyzed using Meso-Scale multiplex technology. Concentrations were adjusted for gestational age at sampling, experimental factors, year of sampling, and covariates (maternal age at sampling, parity (nulliparous/multiparous), smoking at first prenatal visit, and in vitro fertilization). Cox regression analysis of the entire cohort was performed to explore possible associations between protein concentrations and gestational duration. This was followed by Cox regression analysis censored at 259 days or longer, to investigate whether associations were detectable in women with spontaneous preterm delivery (n = 47). Finally, linear regression models were performed to analyze associations between protein concentrations and gestational duration in women with spontaneous onset of labor at term (n = 784). HMG-1, IGFBP-1, IL-18, MIP-1α, MIP-1β, S100A8, and thrombospondin-1 were significantly associated with gestational duration at term, but not preterm. Increased concentrations of thrombospondin-1, MIP-1β, and S100A8, respectively, were significantly associated with decreased gestational duration after the Holm-Bonferroni correction in women with spontaneous onset of labor at term. This adds to the concept of a pregnancy clock, where our findings suggest that such a clock is also reflected in the amniotic fluid at early mid-trimester, but further research is needed to confirm this.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gestational duration has a significant impact on the short- and long-term health of the neonate [1,2,3]. Data indicate that an inflammatory process precedes the onset of labor in both term and preterm pregnancies [4,5,6] and that endocrine, mechanical, and genetic factors are involved [7,8,9]. However, the mechanisms of pregnancy maintenance and timing of delivery are not yet fully understood [10]. The concept of a pregnancy clock, in which chronological and coordinated signals from the fetus, fetal membranes, placenta, decidua, and myometrium modulate the duration of pregnancy [11,12,13], has recently been expanded with the concepts of a proteomic clock and an immune clock [14, 15]. It has been suggested that recognition of disruptive patterns in these chronological signals could enable early detection of pregnancy complications [15].
Amniotic fluid is a biological surrogate for the dynamic environment surrounding the developing fetus, and its origin and composition changes as pregnancy progresses [16]. Previous studies have identified inflammatory biomarkers that are associated with gestational duration in the amniotic fluid at mid-trimester [17, 18]. However, these studies have mainly focused on spontaneous preterm delivery (PTD, < 37 + 0 gestational weeks) and have also been limited to one or a few proteins. The statistical power to detect associations increases when gestational duration is considered to be a continuous variable instead of a dichotomous (term/preterm) trait [19]. A continuous gestational duration variable is also clinically relevant as there is a gradient of increasing risk of adverse neonatal outcome with decreasing gestational duration [1, 20]. Furthermore, the development of multiplex immunoassays, which allow simultaneous analysis of multiple analytes from small sample volumes, has enabled a more explorative approach to protein patterns in biological compartments in relation to pregnancy outcome [21].
This study aimed at evaluating the concentrations of 27 selected proteins in the amniotic fluid of asymptomatic women at mid-trimester in relation to gestational duration and spontaneous PTD, using multiplex technology. The assay panel selected was designed to explore the inflammatory process that precedes the onset of labor.
Methods
Study Design and Participants
In this prospective cohort study, pregnant women were recruited at Sahlgrenska University Hospital/Östra, Gothenburg, Sweden, between September 2008 and June 2016. The women were enrolled before the clinical introduction of noninvasive prenatal testing (NIPT) in 2017. Inclusion criteria were maternal age ≥ 18 years with a viable singleton pregnancy and undergoing genetic amniocentesis at 14–19 gestational weeks. Clinical indications for genetic amniocentesis were maternal age ≥ 35 years, high risk found in the first-trimester combined screening, anxiety, or family history of a chromosomal abnormality or genetic disease. Multiple pregnancy, positive for HIV or hepatitis B, and known or suspected fetal malformations were ineligibility criteria, as were situations in which study samples could not be collected. Women were excluded if they declined participation, could not give informed consent in Swedish due to language difficulties or if an insufficient amount of fluid was retrieved during amniocentesis.
Demographics and pregnancy outcomes were obtained by review of medical records. Gestational age was based on fetal biometry at ultrasound, routinely performed at gestational weeks 17–20. Spontaneous PTD was defined as delivery < 37 gestational weeks, as a result of either preterm labor or preterm prelabor rupture of membranes. Women with medically indicated (iatrogenic) PTD, where various complications affected the duration of pregnancy, as well as women who had a miscarriage, stillbirth, termination of pregnancy, incomplete data or who were lost to follow-up, were excluded from analysis.
Sample Collection and Processing
Amniocentesis was performed transabdominally with a 22-gauge needle under sonographic guidance. An additional 3 ml of fluid was aspirated for research purposes. Samples were stored at + 4–8 °C immediately after sampling and coded. Samples were centrifuged for 20 min at 12,000 g at 4 °C to separate supernatant from the pellet. Aliquots were stored at − 80 °C until analysis. None of the aliquots used in this study had been thawed or used in previous analyses.
Development of the Assay Panel
The assay panel was designed to explore the inflammatory processes and mechanisms preceding the onset of labor, both at term and at preterm. Selection was influenced by previous studies reporting biomarkers associated with term and preterm parturition [6, 22] as well as proteins previously analyzed in a sub-cohort of this project [23]. The selection of DAMPs in the panel was based on the hypothesis that these endogenous mediators trigger an inflammatory process, defined as sterile intra-amniotic inflammation [24, 25], related to the onset of labor both at term [26] and preterm [27].
The panel consisted of 27 cytokines, chemokines, damage-associated molecular patterns (DAMPs), and other proteins, distributed on two 10-plex analysis for analytes that had previously been developed and tested by the institute performing the analyses (panels 1 and 2) and one 7-plex analysis with analytes that had not previously been tested (panel 3).
Analysis of Samples
Analyte concentrations were analyzed at Statens Serum Institut (SSI), Copenhagen, Denmark, using in-house multiplex sandwich immunoassays based on U-PLEX Meso-Scale technology. Samples from spontaneous PTD cases were evenly distributed on the plates by the researchers, to minimize the risk of confounding by the plate layout. Laboratory staff performing the analyses were blinded to clinical information and outcome.
The analysis started with the different capture antibodies being biotinylated, after which they were bound to different linkers (1–10), mixed to reach a concentration of 10 μg/ml per antibody, added to each of the U-PLEX plate (Meso-Scale, K15235) wells (50 μl/well) in all plates in the respective panels and incubated for 1 h. After washing with washing buffer (PBS, containing 0.05% Tween 20), the plates were stored at 4 °C until use. Detection antibodies were sulfo-tagged using Meso-Scale Discovery Gold Sulfo-Tag NHS-Ester (Meso-Scale, R91AO-2). Monocyte chemotactic protein 1 (C-C motif chemokine 2; MCP-1) antibody was purchased from BD Biosciences, while the remaining antibodies came from R&D Systems. Calibrators, consisting of eight samples with known concentrations, were used to create calibration curves to translate readings into concentrations. High and low controls were used to calculate assay variations. Both calibrators and high and low controls were prepared by recombinant antigens and pipetted onto each plate, together with 25μl of samples. The amniotic fluid samples were measured undiluted in panel 1 and panel 3 and diluted 1:5 in panel 2. The plates were sealed, simultaneously incubated and shaken for 2 h and washed three times. The plates were then simultaneously incubated and shaken for another 2 h after adding the corresponding detection antibodies. The plates were washed and 150 μl 2xRead buffer T (Meso-Scale R92TC) per well was added. They were then immediately read on the QuickPlex reader.
Statistical Analyses
Continuous data were presented using median and interquartile range (IQR), while categorical data were presented as frequency distribution. Concentrations were log-transformed for statistical analysis. Amniotic fluid protein concentrations were adjusted for gestational age at sampling, experimental factors (plates), and year of sampling using linear regression. In the following analysis, these adjusted concentrations were used as predictors, together with covariates selected based on previous studies (maternal age at sampling, parity (nulliparous/multiparous), smoking at first prenatal visit, and in vitro fertilization (IVF)) [28,29,30,31]. For each of the amniotic fluid protein concentrations, separately, a Cox regression analysis of the entire study cohort was used to explore possible associations with gestational duration. Cox regression was then censored at 259 days (37 + 0 gestational weeks) or longer to examine whether associations could be detected in women with spontaneous PTD. Linear regression models, followed by a conservative Holm-Bonferroni correction, were used to evaluate protein concentrations’ associations with gestational duration as a continuous variable in women with spontaneous onset of labor at term, as well as to obtain an effect estimate of days/standard deviation (SD). A p value of < 0.05 using a two-sided alternative hypothesis was considered significant. Statistical analysis was performed in SPSS 25.0 for Windows XP OS (SPSS Inc., USA) and R, version 3.3.1.
Results
Characteristics of the Study Population
Between September 2008 and June 2016, 2962 women underwent mid-trimester genetic amniocentesis at the department. After application of the exclusion and ineligibility criteria described above, the study cohort consisted of 1072 women. The selection of study participants is displayed in Fig. 1. Maternal and neonatal characteristics are presented in Table 1.
Flow chart. This figure shows the selection process for the different cohorts in the respective analytical steps. In step I, the entire cohort was analyzed. Step II consists of women with spontaneous PTD, compared with women with term delivery, and step III consists of women with spontaneous onset of labor at term
Candidate Protein Concentrations
The inter-assay coefficients of variation (CV), intra-assay CV, and limits of detection (LOD) for the analytes measured are presented in Table 2. The protein names and, in some cases, the recommended names (in parentheses) and their short-form abbreviations are assigned by the UniProt Consortium [32]. In cases where the protein concentrations reported from SSI were too low or too high to be fitted on the standard curve, values were set at the LOD or at the highest concentration that could be measured for that specific analyte. Triggering receptor expressed on myeloid cells 1 (TREM-1) was one of the initial proteins in panel 2. However, due to cross-reactions in the preparation phase, this protein was not analyzed. A total of 26 analytes were thus measured, and panel 2 consisted of a 9-plex analysis instead. The median concentrations of the 26 examined proteins are presented in Table 3. The majority of the protein concentrations were not affected by storage time, with the exception of IL-10, TNF-β, CRP, MIP-1α, RANTES, and MMP-8.
Protein Concentrations and Gestational Age at Sampling
Seventeen of the 26 proteins were significantly associated with gestational age at sampling (Table 4). Thrombospondin-1 and HMG-1 underwent the most substantial concentration changes, a 3.4% increase and a 3.2% increase in concentration per day, respectively.
Protein Concentrations and Gestational Duration
Step I: The Entire Study Cohort (n = 1072)
The median gestational duration in this cohort was 39 + 6 (IQR, 38 + 5–40 + 6) weeks. HMG-1, IGFBP-1, IL-18, MIP-1α, MIP-1β, S100A8, and thrombospondin-1 concentrations were significantly associated with gestational duration in the Cox regression analysis (Table 5).
Step II: Women with Spontaneous Preterm Delivery (n = 47)
The incidence of spontaneous PTD in the entire study cohort was 4.4% (47/1072). Women with spontaneous PTD were more often nulliparous, had a higher BMI at the first prenatal visit, and had a higher rate of IVF and previous PTD than women with a term delivery (Table 1).
The median gestational duration among women with spontaneous PTD was 35 + 6 (IQR, 33 + 4–36 + 4) weeks, compared with 39 + 6 (IQR, 38 + 6–40 + 6) weeks in women who underwent term delivery.
The selected proteins were not associated with spontaneous PTD in the censored Cox regression model (Table 6), indicating that the associations found in step I were mainly derived from women with term delivery. Women with spontaneous PTD were therefore excluded from further analysis.
Step III: Women with Spontaneous Onset of Labor at Term (n = 784)
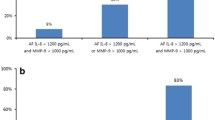
Consequently, the subsequent analyses focused on women with term delivery. Women with induced labor or planned cesarean section at term (n = 241), for whom clinical decisions determined the gestational duration, were excluded from analysis, leaving only women with spontaneous onset of labor at term (n = 784). The median gestational duration in this cohort was 40 + 0 (IQR, 39 + 1–40 + 6) weeks. There were significant associations between thrombospondin-1, MIP-1β, S100A8, IL-18, MIP-1α, IGFBP-1, HMG-1, and TNF-α concentrations and gestational duration in this cohort (Table 5). All but TNF-α remained significant at a false discovery rate (FDR) of 0.1. Thrombospondin-1, MIP-1β, and S100A8 remained significant (pc < 0.05) after a conservative Holm-Bonferroni correction. Scatter plots of the association between the concentrations of thrombospondin-1, MIP-1β, and S100A8 and gestational duration are presented in Fig. 2. For thrombospondin-1, an increase of one standard deviation (SD) in log concentration (corresponding to a 104% increase in concentration) was associated with a 1.1-day decrease in gestational duration. For MIP-1β and S100A8, an increase of one SD in log concentrations (corresponding to a 103% and 57% increase, respectively, in concentration) was associated with a shortened gestational duration by 0.9 day.
Discussion
The key findings were as follows: (i) gestational age at sampling was significantly associated with concentrations of the majority of the selected analytes; (ii) mid-trimester amniotic fluid concentrations of thrombospondin-1, MIP-1β, and S100A8 were significantly associated with gestational duration in women with spontaneous onset of labor at term; and iii) mid-trimester amniotic fluid concentrations of the selected proteins were not associated with spontaneous PTD in this small cohort.
The concentrations of 17 of the 26 candidate proteins were associated with gestational age at sampling despite the limited sampling window of approximately 5 weeks. To our knowledge, this association has not been described to this extent previously, implying that the findings are an essential contribution to the research field and indicating the need to adjust for this variable.
In genetic studies, analyzing gestational duration has proven more successful than dichotomizing this trait, suggesting that a single biological pathway common to all preterm cases is unlikely to be identified [9, 33]. Several of the examined proteins in our study were associated with gestational duration, but these associations appeared to be driven by the term delivery group rather than the spontaneous PTD group. These findings are unique as only a few studies have examined amniotic fluid protein concentrations with gestational duration as a continuous variable [17, 18]. These studies have found an inverse relationship between IL-6 and IL-10 concentrations and gestational duration using enzyme-linked immunosorbent assay (ELISA), a singleplex assay. Their cohorts were small, with a spontaneous PTD rate of 7.2–15.6% and a substantially higher proportion of early PTD. Different assays, cohort sizes, and differences within study populations, such as maternal age, ethnicity, or PTD etiologies, may explain the contradictory results. Further, the risk of PTD in Sweden is generally low [34]. Even in this high-risk cohort, only 4.4% had a spontaneous PTD, limiting the amount of cases to be studied.
Identifying markers specific to spontaneous PTD has proven difficult. Several previous studies, including two by our group [23, 35], have investigated whether mid-trimester amniotic fluid proteins are associated with subsequent spontaneous PTD. The results are conflicting, as some have found associations [36,37,38,39], while others have not [23, 35, 40,41,42]. In this study, none of the selected proteins were associated with spontaneous PTD. However, spontaneous PTD cases of this study mainly occurred late, and infection and inflammation were thus involved to a lesser extent [43]. Our findings support spontaneous PTD as a multifactorial condition with different sub-phenotypes, making early identification of genetic or protein markers more challenging and complex. Furthermore, spontaneous PTD can also originate as a result of acute events which may not be detectable in amniotic fluid as early as at mid-trimester.
Similar issues have been encountered in genetic studies of gestational duration. Several genes associated with this trait have been identified [9, 33, 44], and many of them appear related to inflammatory processes. However, large sample sizes were required to achieve this, and most of the “hits” are still not consistent across cohorts.
Inflammation of non-infectious origin—or sterile inflammation—mediated by DAMPs or alarmins [27], has gained increasing attention. DAMPs are endogenous molecules released in response to cellular injury and death, eliciting an inflammatory response to defend the host through pathways ultimately leading to the release of pro-inflammatory cytokines [45]. This sterile inflammation has previously been described in relation to several pregnancy complications [46], such as spontaneous PTD [27], but also related to the pathway leading to the onset of labor at term [26]. Elevated concentrations of HMG-1, considered the prototypic alarmin [47], have been demonstrated in cases of preterm delivery with intra-amniotic inflammation [48, 49] and in clinical chorioamnionitis at term [50]. We evaluated a few of the classical DAMPs such as HMG-1, HSP70, S100A8, and thrombospondin-1, and three of them (HMG-1, S100A8, and thrombospondin-1) were associated with shorter gestational duration. However, we did not find significant alterations in the concentrations of any of the examined cytokines. We theorize that the increase of DAMPs in early gestation is reflective of trimester-specific, localized events such as the fusion of the fetal membranes and establishment of the amniotic cavity [51] or growth and remodeling of the feto-placental unit, rather than an acute inflammatory process. Based on this, we further hypothesize that there is a relationship between the development of the uterine cavity and gestational duration. It should, however, be emphasized that our results are solely based on protein concentrations from amniotic fluid samples collected between 14 and 19 gestational weeks. These associations may not consist beyond this point.
In women with a spontaneous onset of labor at term, increased concentrations of MIP-1β, S100A8, and thrombospondin-1 were significantly associated with a decrease in gestational duration. MIP-1β has previously been demonstrated in cases of spontaneous PTD at < 34 weeks [52], as well as in women with symptoms of preterm labor who delivered within 7 days [6]. An upregulation of S100A8 is associated with chorioamnionitis/deciduitis [53]. S100-alarmins have also been described as essential immunoregulators in newborns, preventing excessive inflammation [54]. S100A8/A9 have been analyzed in breast milk; concentrations were significantly higher after term delivery, compared with PTD, and after vaginal delivery, compared with cesarean section [55]. Thrombospondin-1 is expressed in the placenta and has previously been reported in cases of small for gestational age (SGA) pregnancies and preeclampsia [56, 57].
Understanding the physiological events preceding parturition in healthy term pregnancies is essential in order to understand pathological pregnancies and, ultimately, possible prevention strategies. Aghaeepour et al. [14, 15] suggest the presence of a proteomic and an immune clock in women delivering at term, where deviations from precisely timed and chronological changes could potentially assist in the early prediction of adverse outcomes. However, they analyzed maternal sera and peripheral blood, repeatedly collected throughout gestation, while this study analyzed the protein composition of amniotic fluid collected at mid-trimester. The association between protein concentrations and gestational duration in this study though evokes the additional concept of a pregnancy clock that may also comprise the amniotic fluid. While the sample size was small, the lack of associations in the preterm group suggests that the immunological response in women with a spontaneous PTD may diverge from that of women delivering at term. However, further research is needed to confirm this.
The strengths of this study were particularly the robust methodology, including meticulous selection criteria, the extensive panel of selected candidate proteins, and the analysis of gestational duration as a continuous rather than a dichotomous (preterm/term) variable. We used two different statistical models and were able to show that the associations are robust to modeling choices. While the Cox regression is natural for modeling the survival outcome, a linear model can be more suited for detecting markers that have time-varying effects—this was previously shown to be likely based on Swedish birth demographics [58].
Furthermore, the cohort is unique due to its size, with a total loss-to-follow-up/missing information rate of only 0.97%. Another strength is that the results have been adjusted for covariates and experimental factors (plates); the latter are frequently neglected. Finally, we used a technology that offers a broader dynamic range and better accuracy, with lower inter- and intra-assay variation [59, 60], than other immunoassay technologies such as LUMINEX. To the best of our knowledge, this is the first study using a Meso-Scale Discovery approach with a broad panel of inflammatory markers in this context.
One limitation is that the study population of women undergoing invasive genetic testing is of advanced age with high risk or a history of chromosomal abnormalities. These circumstances, therefore, might not reflect the general low-risk pregnant population, limiting generalizability. The clinical translation value of our findings is also limited, and the results should rather be seen as interesting biological associations that may serve as a basis for future research. The results have been adjusted for plate effects, but other analytical conditions might have influenced the results. Researchers must be aware of the limitations of new markers and techniques during this rapidly expanding and developing era of biomarker research [60, 61].
Conclusion
Mid-trimester amniotic fluid concentrations of thrombospondin-1, MIP-1β, and S100A8 were significantly associated with gestational duration at term, but not at preterm. This adds to the concept of a pregnancy clock, where our findings suggest that such a clock is also reflected in mid-trimester amniotic fluid. Further research is though needed to explore this. It is important to adjust for gestational age at sampling when performing amniotic fluid biomarker studies.
Data Availability
All relevant data are within the manuscript.
References
Boyle EM, Poulsen G, Field DJ, Kurinczuk JJ, Wolke D, Alfirevic Z, et al. Effects of gestational age at birth on health outcomes at 3 and 5 years of age: population based cohort study. BMJ. 2012;344:e896. https://doi.org/10.1136/bmj.e896.
Moster D, Wilcox AJ, Vollset SE, Markestad T, Lie RT. Cerebral palsy among term and postterm births. JAMA. 2010;304(9):976–82. https://doi.org/10.1001/jama.2010.1271.
Morken NH, Kallen K, Jacobsson B. Outcomes of preterm children according to type of delivery onset: a nationwide population-based study. Paediatr Perinat Epidemiol. 2007;21(5):458–64. https://doi.org/10.1111/j.1365-3016.2007.00823.x.
Christiaens I, Zaragoza DB, Guilbert L, Robertson SA, Mitchell BF, Olson DM. Inflammatory processes in preterm and term parturition. J Reprod Immunol. 2008;79(1):50–7. https://doi.org/10.1016/j.jri.2008.04.002.
Romero R, Espinoza J, Goncalves LF, Kusanovic JP, Friel LA, Nien JK. Inflammation in preterm and term labour and delivery. Semin Fetal Neonatal Med. 2006;11(5):317–26. https://doi.org/10.1016/j.siny.2006.05.001.
Holst RM, Hagberg H, Wennerholm UB, Skogstrand K, Thorsen P, Jacobsson B. Prediction of spontaneous preterm delivery in women with preterm labor: analysis of multiple proteins in amniotic and cervical fluids. Obstet Gynecol. 2009;114(2 Pt 1):268–77. https://doi.org/10.1097/AOG.0b013e3181ae6a08.
Sooranna SR, Lee Y, Kim LU, Mohan AR, Bennett PR, Johnson MR. Mechanical stretch activates type 2 cyclooxygenase via activator protein-1 transcription factor in human myometrial cells. Mol Hum Reprod. 2004;10(2):109–13. https://doi.org/10.1093/molehr/gah021.
Wang B, Parobchak N, Rosen T. RelB/NF-kappaB2 regulates corticotropin-releasing hormone in the human placenta. Mol Endocrinol. 2012;26(8):1356–69. https://doi.org/10.1210/me.2012-1035.
Zhang G, Feenstra B, Bacelis J, Liu X, Muglia LM, Juodakis J, et al. Genetic associations with gestational duration and spontaneous preterm birth. N Engl J Med. 2017;377(12):1156–67. https://doi.org/10.1056/NEJMoa1612665.
Norwitz ER, Robinson JN, Challis JR. The control of labor. N Engl J Med. 1999;341(9):660–6. https://doi.org/10.1056/nejm199908263410906.
McLean M, Bisits A, Davies J, Woods R, Lowry P, Smith R. A placental clock controlling the length of human pregnancy. Nat Med. 1995;1(5):460–3. https://doi.org/10.1038/nm0595-460.
Menon R, Bonney EA, Condon J, Mesiano S, Taylor RN. Novel concepts on pregnancy clocks and alarms: redundancy and synergy in human parturition. Hum Reprod Update. 2016;22(5):535–60. https://doi.org/10.1093/humupd/dmw022.
Norwitz ER, Bonney EA, Snegovskikh VV, Williams MA, Phillippe M, Park JS, et al. Molecular regulation of parturition: the role of the decidual clock. Cold Spring Harbor Perspect Med. 2015;5(11). https://doi.org/10.1101/cshperspect.a023143.
Aghaeepour N, Ganio EA, McIlwain D, Tsai AS, Tingle M, Van Gassen S, et al. An immune clock of human pregnancy. Sci Immunol. 2017;2(15). https://doi.org/10.1126/sciimmunol.aan2946.
Aghaeepour N, Lehallier B, Baca Q, Ganio EA, Wong RJ, Ghaemi MS, et al. A proteomic clock of human pregnancy. Am J Obstet Gynecol. 2018;218(3):347.e1–e14. https://doi.org/10.1016/j.ajog.2017.12.208.
Underwood MA, Gilbert WM, Sherman MP. Amniotic fluid: not just fetal urine anymore. J Perinatol. 2005;25(5):341–8. https://doi.org/10.1038/sj.jp.7211290.
Apuzzio J, Chan Y, Al-Khan A, Illsley N, Kim PL, Vonhaggen S. Second-trimester amniotic fluid interleukin-10 concentration predicts preterm delivery. J Matern Fetal Neonatal Med. 2004;15(5):313–7. https://doi.org/10.1080/14767050410001702186.
Ghidini A, Jenkins CB, Spong CY, Pezzullo JC, Salafia CM, Eglinton GS. Elevated amniotic fluid interleukin-6 levels during the early second trimester are associated with greater risk of subsequent preterm delivery. Am J Reprod Immunol. 1997;37(3):227–31.
Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332(7549):1080. https://doi.org/10.1136/bmj.332.7549.1080.
Platt MJ. Outcomes in preterm infants. Public Health. 2014;128(5):399–403. https://doi.org/10.1016/j.puhe.2014.03.010.
Skogstrand K. Multiplex assays of inflammatory markers, a description of methods and discussion of precautions - our experience through the last ten years. Methods. 2012;56(2):204–12. https://doi.org/10.1016/j.ymeth.2011.09.025.
Keelan JA, Blumenstein M, Helliwell RJ, Sato TA, Marvin KW, Mitchell MD. Cytokines, prostaglandins and parturition--a review. Placenta. 2003;24 Suppl A:S33–46.
Hallingstrom M, Cobo T, Kacerovsky M, Skogstrand K, Hougaard DM, Holst RM, et al. The association between selected mid-trimester amniotic fluid candidate proteins and spontaneous preterm delivery. J Matern Fetal Neonatal Med. 2018;33:1–10. https://doi.org/10.1080/14767058.2018.1497604.
Combs CA, Gravett M, Garite TJ, Hickok DE, Lapidus J, Porreco R, et al. Amniotic fluid infection, inflammation, and colonization in preterm labor with intact membranes. Am J Obstet Gynecol. 2014;210(2):125.e1–e15. https://doi.org/10.1016/j.ajog.2013.11.032.
Romero R, Miranda J, Chaiworapongsa T, Chaemsaithong P, Gotsch F, Dong Z, et al. Sterile intra-amniotic inflammation in asymptomatic patients with a sonographic short cervix: prevalence and clinical significance. J Matern-Fetal Neonatal Med. 2015;28(11):1343–59. https://doi.org/10.3109/14767058.2014.954243.
Kobayashi H. The entry of fetal and amniotic fluid components into the uterine vessel circulation leads to sterile inflammatory processes during parturition. Front Immunol. 2012;3:321. https://doi.org/10.3389/fimmu.2012.00321.
Romero R, Miranda J, Chaiworapongsa T, Korzeniewski SJ, Chaemsaithong P, Gotsch F, et al. Prevalence and clinical significance of sterile intra-amniotic inflammation in patients with preterm labor and intact membranes. Am J Reprod Immunol. 2014;72(5):458–74. https://doi.org/10.1111/aji.12296.
Jackson RA, Gibson KA, Wu YW, Croughan MS. Perinatal outcomes in singletons following in vitro fertilization: a meta-analysis. Obstet Gynecol. 2004;103(3):551–63. https://doi.org/10.1097/01.aog.0000114989.84822.51.
Kyrklund-Blomberg NB, Cnattingius S. Preterm birth and maternal smoking: risks related to gestational age and onset of delivery. Am J Obstet Gynecol. 1998;179(4):1051–5. https://doi.org/10.1016/s0002-9378(98)70214-5.
Kozuki N, Lee AC, Silveira MF, Sania A, Vogel JP, Adair L, et al. The associations of parity and maternal age with small-for-gestational-age, preterm, and neonatal and infant mortality: a meta-analysis. BMC Public Health. 2013;13 Suppl 3:S2. https://doi.org/10.1186/1471-2458-13-s3-s2.
Jacobsson B, Ladfors L, Milsom I. Advanced maternal age and adverse perinatal outcome. Obstet Gynecol. 2004;104(4):727–33. https://doi.org/10.1097/01.AOG.0000140682.63746.be.
UniProt: a worldwide hub of protein knowledge. Nucleic Acids Res. 2019;47(D1):D506–d15. https://doi.org/10.1093/nar/gky1049.
Liu X, Helenius D, Skotte L, Beaumont RN, Wielscher M, Geller F, et al. Variants in the fetal genome near pro-inflammatory cytokine genes on 2q13 associate with gestational duration. Nat Commun. 2019;10(1):3927. https://doi.org/10.1038/s41467-019-11881-8.
Ferrero DM, Larson J, Jacobsson B, Di Renzo GC, Norman JE, Martin JN Jr, et al. Cross-country individual participant analysis of 4.1 million singleton births in 5 countries with very high human development index confirms known associations but provides no biologic explanation for 2/3 of all preterm births. PLoS One. 2016;11(9):e0162506. https://doi.org/10.1371/journal.pone.0162506.
Hallingstrom M, Lenco J, Vajrychova M, Link M, Tambor V, Liman V, et al. Proteomic analysis of early mid-trimester amniotic fluid does not predict spontaneous preterm delivery. PLoS One. 2016;11(5):e0155164. https://doi.org/10.1371/journal.pone.0155164.
Ghezzi F, Franchi M, Raio L, Di Naro E, Bossi G, D'Eril GV, et al. Elevated amniotic fluid C-reactive protein at the time of genetic amniocentesis is a marker for preterm delivery. Am J Obstet Gynecol. 2002;186(2):268–73.
Hsu TY, Lin H, Lan KC, Ou CY, Tsai CC, Cheng BH, et al. High interleukin-16 concentrations in the early second trimester amniotic fluid: an independent predictive marker for preterm birth. J Matern Fetal Neonatal Med. 2013;26(3):285–9. https://doi.org/10.3109/14767058.2012.733750.
Puchner K, Iavazzo C, Gourgiotis D, Boutsikou M, Baka S, Hassiakos D, et al. The implication of second-trimester amniotic fluid TNF-alpha, cytochrome C and cell death nucleosomes in the prediction of preterm labor and/or premature rupture of membranes. Arch Gynecol Obstet. 2012;285(1):37–43. https://doi.org/10.1007/s00404-011-1909-7.
Wenstrom KD, Andrews WW, Hauth JC, Goldenberg RL, DuBard MB, Cliver SP. Elevated second-trimester amniotic fluid interleukin-6 levels predict preterm delivery. Am J Obstet Gynecol. 1998;178(3):546–50.
Bamberg C, Fotopoulou C, Thiem D, Roehr CC, Dudenhausen JW, Kalache KD. Correlation of midtrimester amniotic fluid cytokine concentrations with adverse pregnancy outcome in terms of spontaneous abortion, preterm birth, and preeclampsia. J Matern Fetal Neonatal Med. 2012;25(6):812–7. https://doi.org/10.3109/14767058.2011.587918.
Kesrouani A, Chalhoub E, El Rassy E, Germanos M, Khazzaka A, Rizkallah J, et al. Prediction of preterm delivery by second trimester inflammatory biomarkers in the amniotic fluid. Cytokine. 2016;85:67–70. https://doi.org/10.1016/j.cyto.2016.06.008.
Payne MS, Feng Z, Li S, Doherty DA, Xu B, Li J, et al. Second trimester amniotic fluid cytokine concentrations, Ureaplasma sp colonisation status and sexual activity as predictors of preterm birth in Chinese and Australian women. BMC Pregnancy Childbirth. 2014;14:340. https://doi.org/10.1186/1471-2393-14-340.
Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med. 2000;342(20):1500–7. https://doi.org/10.1056/nejm200005183422007.
Bacelis J, Juodakis J, Sengpiel V, Zhang G, Myhre R, Muglia LJ, et al. Literature-informed analysis of a genome-wide association study of gestational age in Norwegian women and children suggests involvement of inflammatory pathways. PLoS One. 2016;11(8):e0160335. https://doi.org/10.1371/journal.pone.0160335.
Yang, Han Z, Oppenheim JJ. Alarmins and immunity. Immunol Rev. 2017;280(1):41–56. https://doi.org/10.1111/imr.12577.
Nadeau-Vallee M, Obari D, Palacios J, Brien ME, Duval C, Chemtob S, et al. Sterile inflammation and pregnancy complications: a review. Reproduction. 2016;152(6):R277–r92. https://doi.org/10.1530/rep-16-0453.
Bianchi ME. DAMPs, PAMPs and alarmins: all we need to know about danger. J Leukoc Biol. 2007;81(1):1–5. https://doi.org/10.1189/jlb.0306164.
Romero R, Chaiworapongsa T, Alpay Savasan Z, Xu Y, Hussein Y, Dong Z, et al. Damage-associated molecular patterns (DAMPs) in preterm labor with intact membranes and preterm PROM: a study of the alarmin HMGB1. J Matern Fetal Neonatal Med. 2011;24(12):1444–55. https://doi.org/10.3109/14767058.2011.591460.
Baumbusch MA, Buhimschi CS, Oliver EA, Zhao G, Thung S, Rood K, et al. High mobility group-box 1 (HMGB1) levels are increased in amniotic fluid of women with intra-amniotic inflammation-determined preterm birth, and the source may be the damaged fetal membranes. Cytokine. 2016;81:82–7. https://doi.org/10.1016/j.cyto.2016.02.013.
Romero R, Chaiworapongsa T, Savasan ZA, Hussein Y, Dong Z, Kusanovic JP, et al. Clinical chorioamnionitis is characterized by changes in the expression of the alarmin HMGB1 and one of its receptors, sRAGE. J Matern Fetal Neonatal Med. 2012;25(6):558–67. https://doi.org/10.3109/14767058.2011.599083.
Menon R, Richardson LS, Lappas M. Fetal membrane architecture, aging and inflammation in pregnancy and parturition. Placenta. 2019;79:40–5. https://doi.org/10.1016/j.placenta.2018.11.003.
Lee SM, Park KH, Jung EY, Cho SH, Ryu A. Prediction of spontaneous preterm birth in women with cervical insufficiency: comprehensive analysis of multiple proteins in amniotic fluid. J Obstet Gynaecol Res. 2016;42(7):776–83. https://doi.org/10.1111/jog.12976.
Phillips RJ, Fortier MA, Lopez BA. Prostaglandin pathway gene expression in human placenta, amnion and choriodecidua is differentially affected by preterm and term labour and by uterine inflammation. BMC Pregnancy Childbirth. 2014;14:241. https://doi.org/10.1186/1471-2393-14-241.
Ulas T, Pirr S, Fehlhaber B, Bickes MS, Loof TG, Vogl T, et al. S100-alarmin-induced innate immune programming protects newborn infants from sepsis. Nat Immunol. 2017;18(6):622–32. https://doi.org/10.1038/ni.3745.
Pirr S, Richter M, Fehlhaber B, Pagel J, Hartel C, Roth J, et al. High amounts of S100-alarmins confer antimicrobial activity on human breast milk targeting pathogens relevant in neonatal sepsis. Front Immunol. 2017;8:1822. https://doi.org/10.3389/fimmu.2017.01822.
Andraweera PH, Dekker GA, Thompson SD, North RA, McCowan LM, Roberts CT. A functional variant in the thrombospondin-1 gene and the risk of small for gestational age infants. J Thromb Haemost. 2011;9(11):2221–8. https://doi.org/10.1111/j.1538-7836.2011.04494.x.
Ulu I, Cekmez Y, Yildirim Kopuk S, Ozer N, Yogurtcuoglu EE, Angin P, et al. Maternal serum thrombospondin-1 is significantly altered in cases with established preeclampsia. J Matern Fetal Neonatal Med. 2019;32(15):2543–6. https://doi.org/10.1080/14767058.2018.1441279.
Juodakis J, Bacelis J, Zhang G, Muglia LJ, Jacobsson B. Time-variant genetic effects as a cause for preterm birth: insights from a population of maternal cousins in Sweden. G3 (Bethesda). 2017;7(4):1349–56. https://doi.org/10.1534/g3.116.038612.
Thompson DK, Huffman KM, Kraus WE, Kraus VB. Critical appraisal of four IL-6 immunoassays. PLoS One. 2012;7(2):e30659. https://doi.org/10.1371/journal.pone.0030659.
Chowdhury F, Williams A, Johnson P. Validation and comparison of two multiplex technologies, Luminex and Mesoscale discovery, for human cytokine profiling. J Immunol Methods. 2009;340(1):55–64. https://doi.org/10.1016/j.jim.2008.10.002.
Malekzadeh A, de Groot V, Beckerman H, van Oosten BW, Blankenstein MA, Teunissen C. Challenges in multi-plex and mono-plex platforms for the discovery of inflammatory profiles in neurodegenerative diseases. Methods. 2012;56(4):508–13. https://doi.org/10.1016/j.ymeth.2012.03.017.
Acknowledgments
Open access funding provided by University of Gothenburg. The authors would like to acknowledge the Prenatal Clinic at the Department of Obstetrics and Gynecology, Sahlgrenska University Hospital/Östra, Gothenburg, Sweden, for their help with recruitment and sampling and the staff at the Perinatal Laboratory for their help with recruitment and processing of samples.
Funding
The study was supported by grants from Agreement concerning research and education of doctors, Sweden (grant numbers: ALFGBG-11522, ALFGBG-136431, ALFGBG-426411, ALFGBG-507701, ALFGBG-671611, and ALFGBG-717501), the Health and Medical Care Committee of the Regional Executive Board, Region Västra Götaland, Sweden (grant numbers: VGFOUREG-231311, VGFOUREG-308151, and VGFOUREG-368351), and the foundation “Stiftelsen Fru Mary von Sydows, född Wijk, donationsfond,” Sweden. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Felicia Viklund: Data curation, formal analysis, investigation, writing (original draft) Maria Hallingström: Conceptualization, methodology, investigation, writing (original draft), project administration, funding acquisitionMarian Kacerovsky: Conceptualization, methodology, supervision, writing (review and editing) Teresa Cobo: Conceptualization, methodology, supervision, writing (review and editing) Kristin Skogstrand: Investigation, resources, writing (review and editing)David M. Hougaard: Investigation, resources, writing (review and editing)Karin Sävman: Conceptualization, writing (review and editing)Ylva Carlsson: Investigation, resources, writing (review and editing)Panagiotis Tsiartas: Investigation, resources, writing (review and editing)Julius Juodakis: Validation, formal analysis, writing (review and editing)Staffan Nilsson: Formal analysis, writing (review and editing) Bo Jacobsson: Conceptualization, methodology, investigation, resources, writing (review and editing), supervision, funding acquisition
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethical Review Board at the University of Gothenburg, Sweden (January 22, 2003/No. Dnr. Ö 639-03; April 24, 2008/No. T 318–08; August 18, 2011/No. T 694-11).
Consent to Participate
Written informed consent was obtained from all participants.
Consent for Publication
Not applicable.
Code Availability
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Felicia Viklund and Maria Hallingström should be considered joint first authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Viklund, F., Hallingström, M., Kacerovsky, M. et al. Protein Concentrations of Thrombospondin-1, MIP-1β, and S100A8 Suggest the Reflection of a Pregnancy Clock in Mid-Trimester Amniotic Fluid. Reprod. Sci. 27, 2146–2157 (2020). https://doi.org/10.1007/s43032-020-00229-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-020-00229-z