Abstract
The treatment of headache disorders is adapted to their severity. It is the aim of this study to evaluate the probability of treatment decisions being taken and to identify underlying principles influencing them. The study was internet-based and cross-sectional; participants completed the EUROLIGHT questionnaire anonymously. Inclusion criterion was the consent to participate. Participants were excluded if diagnostic questions had not been completed. We estimated probabilities based on relative frequencies and built binary logistic regression models to identify factors influencing decision-making. The survey was completed by 976 individuals; 636 completed the diagnostic questions. The probability of a patient to consult a GP or a neurologist was 0.26 and 0.20, respectively. Patients decided by a probability of 0.93 to take acute treatment. These treatment decisions, which were taken by patients alone increased in probability with increasing ictal burden (P < 0.001, P < 0.001 and P < 0.001). The probability of treating migraine with triptans was 0.74; the probability to take a prophylactic treatment was 0.43. Neurologists were more likely than GPs to prescribe these medications (P = 0.006 and P < 0.001, respectively). We identified several principles underlying treatment decisions. Most patients decide to take acute treatment for headache attacks; they are less likely to treat their headache disorder interictally. Treatment decisions are less likely to be taken if more than one decision-maker is involved; if physicians are involved, severity of the headache disorder does not affect the probability of a treatment decision being taken. Overall, the more severely affected a headache patient, the less likely an adequate treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Headache disorders affect patients’ lives to varying extent. While some suffer only occasional attacks hardly affecting their everyday lives, others find their well-being curtailed [20]. Guidelines consequently advise tailoring treatment regimens to individual needs [3, 5, 16, 17].
Finding an adequate therapy is not straightforward. Of several available remedies, patients and physicians choose by trial and error. When headache attacks increase in frequency, taking a prophylactic treatment may prove beneficial [17]. Non-pharmacological treatment approaches help many [1], but are more difficult to apply and time-consuming than simply taking a pill. Referral to a headache expert may be necessary when the ictal burden rises [18].
However, the effort of treating a headache disorder increases with its severity, as treatment needs to be escalated. Furthermore, treatment will only be administered if patients (and—in the case of prescription drugs—their doctors) decide to do so. Severely affected headache patients need to work their way up to an adequate treatment regimen, and some might never reach an adequate level [10, 26]. Little is known about the number of patients who give up (or are given up) despite remaining treatment options.
It is the aim of this study to estimate in a real-life sample the probabilities of decisions about headache treatment being taken and to identify underlying principles.
Methods
Study Design, Inclusion and Exclusion Criteria
We conducted an internet-based study and invited potential participants through posters, journal articles and web pages to complete the EUROLIGHT questionnaire [2]; data were collected anonymously. Inclusion criterion was the consent to participate. We excluded participants who had not answered all diagnostic questions. Headache phenotypes were assessed as published [19].
Recruitment/enrolment was initiated in March 2019 and halted in March 2020. As data were collected anonymously, no formal ethical approval was necessary according to Swiss legislation.
Outcome Measures
In this study, we aim to estimate the probability of a treatment decision A being taken, provided that the premises B are met, i.e. P(A| B). The probabilities P(A), P(B) as well as P(A ∩ B) are estimated based on the collected data (empirical probability); P(A| B) will be calculated according to Eq. 1. The decisions (A) to be analysed as well as their premises (B) are listed in Table 1.
Next, we built binary logistic regression models (BLR) for decisions 1 to 4.1 and 5.1 (Table 3) to identify covariates that influence the probability of decision A being taken, premises B being met. Sex, occupation (working and studying vs. unemployment, retirement and homemaker) and headache phenotype (migraine vs. TTH), as well as age, the number of headache days during the last 30 days, the number of days on which the participants were unable to work during the last 30 days because of headaches and the scores of the depression and anxiety subscales of the Hospital Anxiety and Depression Scale [27], were included as covariates. In addition, for decisions 4.1 and 5.1, we included the speciality of the treating physician (neurology vs. general medicine) into the model.
Covariates in the final model were chosen using a stepwise backward selection method; a variable was removed if the probability of its score statistic was above 0.05.
Statistical Analysis
Statistical analyses were performed with IBM SPSS statistics, version 25. We estimated probabilities based on relative frequencies (empirical probabilities); probabilities are reported as ranging from 0 to 1, and proportions as percentages. Average values are presented with their standard deviation and are compared with other average values through analyses of variance. Correlations are assessed with Pearson’s correlation coefficient. We refer to missing values as “not reported” (n.r.). Significance level was set at 0.05.
Results
The survey was completed by 976 individuals; 636 participants (54.7%) had responded to all diagnostic questions of the EUROLIGHT questionnaire. Migraine was diagnosed in 376 (59.1%), probable migraine in 98 (15.4%), tension-type headache (TTH) in 143 (22.5%) and probable TTH in 19 (3.0%). At least one headache attack during the last 30 days had occurred in 616 of 634 participants (2 n.r.).
Only datasets of participants with identifiable headache phenotypes were taken for further analysis. In the following, the phenotypes migraine and probable migraine as well as the phenotypes TTH and probable TTH are aggregated. The demographic profile is detailed in Table 2.
Seeking Medical Advice
More than half of the participants had not consulted any doctor for their headache disorder during the last 12 months (384/608, 63.1%, 28 n.r.). Of those who had, 102 (45.5%) had been treated by a GP alone, 66 by a neurologist (29.5%) and 56 by both (25.0%).
The estimated probability of a person with headaches to consult a GP was 0.26 (Table 1). The number of monthly headache days (P < 0.001) and headache phenotype (P = 0.001) significantly influenced this probability according to BLR (Table 3). A higher ictal burden was associated with an increased probability; participants with migraine were more likely to contact a GP (OR = 2.850, 95%-CI 1.509–5.384) than patients with migraine were.
The estimated probability of a person to consult a neurologist for their headache was 0.20 (Table 1). BLR revealed that the monthly number of headache days and the headache phenotype significantly influenced this decision (P < 0.001, P = 0.010, respectively). Migraine was associated with a higher likelihood of consulting a neurologist (OR = 2.586, 95%-CI 1.251–5.343, Table 3).
On average, participants who had not been treated by a doctor had 6 ± 5 headache days per month, those treated by a GP had 11 ± 8 days and participants treated by a neurologist (or both a neurologist and a GP) had 13 ± 9 headache days (2 n.r.). The difference in headache days between patients treated by no physician and any physician was significant (P < 0.001). Those who consulted a GP had significantly less headache days than those who consulted a neurologist (P = 0.048).
Treatment Decisions
Most participants took OTC medication (NSAIDs or paracetamol) to treat their headaches (532/578, 58 n.r.); the estimated probability to take one of these drugs was 0.93 (Table 1). BLR identified three factors that significantly influenced this probability.
Migraine patients took NSAIDs or paracetamol more frequently (OR = 3.256, 95%-CI 1.684–6.295, P < 0.001) than patients with TTH did. In addition, with increasing number of headache days (P < 0.001), the number of days when participants had been unable to work (P < 0.001) increased, and the probability of taking OTC medication increased likewise (Table 3).
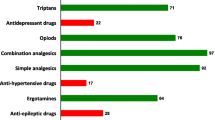
In Switzerland, triptans are available on prescription only. Treatment with these medications was less common than a treatment with OTC medication; 40.6% of all participants reported taking triptans (200/493, 143 n.r.).
Migraineurs with a moderate or high pain intensity during their attacks who had been treated by a GP or a neurologist during the last 12 months had an estimated probability of 0.74 of taking—and thus having received a prescription for—triptans (149 n.r.). The only factor significantly influencing whether a patient took triptans was the speciality of her/his physician (Table 3); patients being treated by a neurologist were more likely to have received a prescription (OR = 2.655, 95%-CI 1.317–5.351, P = 0.006).
The Swiss Headache Association generally recommends prescribing a prophylactic treatment to patients with migraine suffering six or more headache days per month; no precise cut-off value for a prophylactic treatment of TTH is provided [3]. Half of all participants (50.8%, 322/634, 2 n.r.) had at least six headache days per month. Of these, about one third had consulted a doctor during the last 12 months (27.7%, 168/606, 30 n.r.).
The probability of taking a prophylactic treatment was 0.43 in patients suffering from 6 or more headache days per month and treated by a GP or a neurologist (Table 1).
The only covariate significantly influencing whether a patient was treated prophylactically was the specialty of the treating physician (Table 3). Patients treated by a neurologist were significantly more likely to take a prophylactic treatment (OR = 4.415, 95%-CI 1.954–9.976, P < 0.001).
The probabilities of the assessed therapeutic decisions being taken (numbers 3, 4.1, 4.2, 4.3, 5.1, 5.2 and 5.3) correlated highly (r = 0.57) with the number of eligible patients (Table 1).
Discussion
We analysed the probabilities of decisions about headache treatment being taken. The data suggest that whether a decision is probable or improbable depends mainly on several principles underlying decision-making processes.
Decisions about headache treatment can be subdivided into two subgroups depending on the number of decision-makers involved. Patients choose by themselves to take OTC medication and to seek a physician’s advice. In decisions about prescription drugs, a second decision-maker—the prescriber—is involved.
Single decision-makers are likely to decide taking OTC medication—almost everyone relied on a pharmacological treatment (Table 1). BLR revealed that the most important reasons were headache phenotype and ictal burden. Consequently, to reduce impairment seems to be the most important motivation to treat. This unsurprising finding supports the notion of pain conveying imperatives.
Imperativism is a philosophical theory suggesting that the purpose of pain is to influence human behaviour (it “motivates towards action”) [11]. In that aspect, pain resembles thirst and hunger more closely than sensory input. Although migraine attacks might be triggered by external factors [13, 14], removing these triggers is unlikely to interrupt the ongoing attack. Consequently, taking acute treatment may be the only way that quickly leads to pain freedom and thus responds to the imperative.
The probability of a patient deciding to self-treat was higher than the probability of a patient seeking a physician’s advice. We suppose that the latter decision is taken interictally in the absence of pain. This would suggest that consulting a doctor is not a direct consequence of pain influencing human behaviour through imperatives but the result of a cognitive process to find a solution to repeated interruptions of well-being.
The decision to consult a physician depends significantly on the ictal burden (determined by pain phenotype and attack frequency), suggesting that a reduction of impairment might reduce the need for a physician. Although previous research has pointed out that women are more likely to seek a physician’s advice for headache [7], our data do not corroborate that finding. Also, anxiety and depression were not found to influence that decision.
Overall, the above-mentioned findings suggest that the driving force behind decisions that patients take is the desire to end pain and burden. Things change when a second decision-maker comes into play.
Doctors offer additional means to reach patients’ therapeutic goals. Apart from providing information and recommending non-pharmacological interventions, they may prescribe triptans and prophylactic drugs.
Triptans are drugs that were developed to treat migraine. While systematic reviews failed to find a general superiority of triptans over NSAIDs [25], patients generally express greater satisfaction with the former [8]. It has been recommended that migraine attacks be treated with triptans if pain intensity can be expected to become moderate to severe [24]. Among participants meeting these criteria, the empirical probability of taking triptans was 0.74 (Table 1). This supports the conclusion drawn in a previous study that too few migraine patients receive triptans [10].
Furthermore, we estimated the probability of taking a prophylactic drug among patients who had six or more headache days per month. While some authors recommend taking prophylactic drugs with different numbers of headache days [5, 16, 17], we felt that most headache experts would probably agree that patients in this group might benefit from a prophylactic treatment irrespective of their headache phenotype (migraine and TTH).
As prophylactic drugs are taken daily, patients decide taking them in the absence of pain. Again, our data imply that patients are less likely to decide taking a pill in the absence of pain—the probability of taking triptans was 0.74, while that of taking a prophylactic treatment was 0.43 (Table 1). This seconds Katsavara et al. who found that too few patients receive prophylactic drugs [10] but also suggests that patients prefer treating pain when it is present—and not when it is not.
The probability of a patient receiving a prescription drug is well below the probability of a patient taking OTC medication (Table 1). Other potential reasons left aside, this difference may be due to the involvement of a second decision-maker.
Physicians decide with a certain probability to recommend a treatment escalation and to prescribe a new medication; patients on the other side decide whether they are willing to take it. As two positive assessments are necessary for the treatment to be started, one might suspect that the probabilities of these positive assessments are multiplied to calculate the probability of a prescription being made. In this case, if the probabilities were below 1, the product would be even smaller.
Our study design does not allow to measure the extent to which patient and physician influence each other in decision-making. However, if these decisions were taken completely independently, it would be unlikely for of the patient to consent—and perhaps irrational.
It is important to realize that while most patients have already used NSAIDs or paracetamol in the past, they are probably unfamiliar with triptans or prophylactic drugs. The probability of the state “treatment relieves pain” to occur is unknown to them (Table 4). If their physician did not give some idea about what to expect, they would be taking a so-called “decision under ignorance” [15].
Different ways have been proposed to take such a decision [15]. For instance, pessimistic patients might try to prevent the worst outcome (this strategy is called the “maximin principle”). In this case, they would probably refuse taking a new medication as “equal amount of pain and side-effects” is the least favourable outcome (Table 4). More optimistic patients may choose the option with the best possible outcome. However, whether the best option really is “less pain but side-effects” depends on the amount of pain reduction and the side-effects to be expected. If patients guessed that the side-effects were horrible, it would be irrational to take the pills. Consequently, they need advice and information.
We suspect that patients’ uncertainty is an important factor that prevents treatment escalation. Therefore, it is mandatory for doctors to give their patients an idea of what to expect. The importance of the quality indicator “patients are given the information they need to understand their headache and its management,” which has been advanced by Steiner et al. [21], cannot be overemphasized.
The regression models (Table 3) suggested that whether a patient received a prescription drug mainly depended on the specialty of the treating physician. In addition, patients with more depressive symptoms were slightly less likely to receive triptans. (Given that pessimistic attitudes may be part of a depression [9], this finding suggests that these patients might apply the “maximin principle”—see above—to take a decision.)
Surprisingly, the ictal burden had no significant influence on the likelihood of the prescription of a drug. (This finding challenges the idea of patients and their physician sharing a common therapeutic goal.) The reason for this is unknown but we speculate that individual factors—notably on the doctor’s side—are more relevant.
The importance of the physician’s specialty has been found in a previous study [10] as well and is noteworthy. Considering that neurologists escalate treatment more often, the suggestion of referring severely affected patients from primary care to secondary or tertiary headache centres seems reasonable [18]. However, this method also introduces obstacles to treatment escalation because not everybody will be or wants to be referred. If patients could contact healthcare providers on the required level themselves, they might obtain an adequate treatment more easily or more quickly.
Furthermore, we found a high correlation between the number of eligible patients and the probability of the decision to treat being taken (Table 1). This suggests that decisions are less likely to be taken the less frequently they arise. Given that the number of eligible patients decreases with increasing disease severity (Table 1) and assuming that severely affected patients should be treated with triptans and a prophylactic treatment, these findings have an important implication: The more severely affected a patient, the less likely is an adequate treatment. This finding is supported by previous research [10, 26].
This conclusion is of even bigger concern as we analysed only individual decisions and ignored that patients first need to put themselves in a position where treatment decisions can be taken. Before being able to decide taking an OTC drug, patients must have gone to a pharmacy and bought a package. Before deciding about taking a prescription drug, patients must first find a doctor, make an appointment, wait for the appointment, detail their symptoms and then—perhaps—receive information about further treatment options.
As we saw in the analysed decisions (Table 1), no decision is taken with a probability of 1. Hence, some are going to “fall by the wayside” at each step; the more steps required to obtain a treatment, the smaller the proportion of patients receiving it. Apart from allowing patients to contact headache specialists directly if their ictal burden is sufficiently large, facilitating access to advanced treatment approaches should be considered as well. For instance, following the example of some countries [22, 23], triptans could be sold in pharmacies without prescription.
A further issue contributing to the difficulty of receiving an adequate treatment may be the diagnostic classification itself. In the International Classification of Headache Disorders, several migraine phenotypes are distinguished but only two degrees of ictal burden—episodic and chronic migraine—, the latter being diagnosed too infrequently [4, 6]. Introducing into the classification degrees of severity that are easy to discern would offer the opportunity to guide treatment decisions.
We suggest distinguishing degrees of severity based on ictal impairment, as these are the main reasons for patients to seek a physician’s advice—see above. Subsequently, guidelines might provide more binding recommendations for each degree of severity. While patients and physicians may decide to deviate from the recommendations, we believe that this system would help making treatment escalations more probable. This conclusion is supported by Lipton and co-workers. They found that adapting treatment to a patient’s needs provided better clinical outcomes than escalating the treatment if the results are unsatisfactory [12].
For instance, it could be suggested to treat a low-severity migraine with NSAIDs, paracetamol or triptans. For medium severity, a prophylactic agent may be added. For a high severity, an additional treatment such as onabotulinumtoxin A or CGRP antagonists and inpatient care could be recommended.
Limitations
Some limitations need to be addressed. First, the sample is not representative. Although many potential participants were invited and many agreed to fill in the questionnaire, subgroups of the target population might not have taken part. With the study design not allowing assessment of the non-response error, we focused on the relations between subgroups instead of calculating prevalence rates.
Second, the probabilities listed in Table 1 are estimates based on relative frequencies. In a larger sample, different values might have been found. However, most conclusions drawn in this article do not depend on precise values but on relationships between values, which are more robust to changes.
Third, although we aimed to analyse individual decisions, most of them could be subdivided further into interim decisions. More research is needed to investigate these as well as the individual role of all participating decision-makers.
In addition, we only assessed the current headache frequency and did not ask for the headache frequency at the last consultation. However, we assume that in patients who do not receive a prophylactic treatment, the headache frequency remains relatively stable.
The algorithm used to diagnose headache disorders distinguishes only between tension-type headache and migraine [19]. Consequently, less common headache types like cluster headache might have been missed and misclassified.
Finally, we did not correct for multiple testing. This decision was taken deliberately, as the purpose of this study was to create new hypotheses rather than confirm pre-existing ones.
Conclusions
The data collected and analysed in this study suggest that decisions about headache treatment are guided by several factors.
First, the probability of deciding to take an acute treatment increases with the number of headache attacks; consequently, the driving force behind the decision probably is the desire to be pain-free. Second, patients are more willing to treat their pain while in pain; the decision to treat and act prophylactically (while pain-free) is less probable.
Third, decisions about pharmacological treatments are less likely to be taken if more than one decision-maker is involved. Fourth, severity of the headache disorder does not influence decisions about headache treatment if doctors are involved. Fifth, if patients are not provided with enough information about side effects and the efficacy of a medication unknown to them, they might act irrationally if they consented to the treatment.
Finally, the higher the number of steps necessary to obtain a treatment, the smaller the probability of obtaining that treatment. For patients with a higher ictal burden, more steps are necessary to obtain advanced treatment approaches; hence, the more severely affected a headache patient, the less likely is an adequate treatment.
We propose different options to increase the probability of adapting treatment to the degree of severity of the headache disorder.
First, the number of decisions that can be taken by the patient himself/herself could be increased. For instance, triptans might be sold as OTC drugs. Second, the access to specialized headache care could be eased. For instance, patients with a high ictal burden should be encouraged to contact headache experts directly. In addition, the number of headache experts may be increased. Third, doctors should make sure that their patients have sufficient knowledge about efficacy and side effects of a recommended treatment (e.g. with information brochures [21]). Finally, more precise and binding treatment recommendations with less room for interpretation could be formulated. To facilitate that process, it may be helpful to include a higher number of degrees of severity that are easy to diagnose into future versions of the headache classification.
Abbreviations
- BLR:
-
Binary logistic regression
- CI:
-
Confidence interval
- GP:
-
General practitioner
- HADS:
-
Hospital Anxiety and Depression Scale
- n.r.:
-
Not reported
- NSAID:
-
Non-steroidal anti-inflammatory drug
- OTC:
-
Over-the-counter
- TTH:
-
Tension-type headache
References
Andrasik F. What does the evidence show? Efficacy of behavioural treatments for recurrent headaches in adults. Neurol Sci. 2007;28(Suppl 2):S70–7.
Andree C, Vaillant M, Barre J, et al. Development and validation of the EUROLIGHT questionnaire to evaluate the burden of primary headache disorders in Europe. Cephalalgia. 2010;30:1082–100.
Andrée C, Barone-Kaganas I, Biethahn S et al. Therapieempfehlungen für primäre Kopfschmerzen. In:Schweizerische Kopfwehgesellschaft SKG. 2019
Anonymous. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1–211.
Bendtsen L, Birk S, Kasch H, et al. Reference programme: diagnosis and treatment of headache disorders and facial pain. Danish Headache Society, 2nd Edition, 2012. J Headache Pain. 2012;13(Suppl 1):S1–29.
Buse DC, Lipton RB, Reed M, et al. Barriers to chronic migraine care: results of the CaMEO (Chronic Migraine Epidemiology & Outcomes) study (I9-1.004). Neurology. 2014;82:I9–1.004.
Celentano DD, Linet MS, Stewart WF. Gender differences in the experience of headache. Soc Sci Med. 1990;30:1289–95.
Dowson AJ, Tepper SJ, Dahlof C. Patients’ preference for triptans and other medications as a tool for assessing the efficacy of acute treatments for migraine. J Headache Pain. 2005;6:112–20.
Herwig U, Bruhl AB, Kaffenberger T, et al. Neural correlates of ‘pessimistic’ attitude in depression. Psychol Med. 2010;40:789–800.
Katsarava Z, Mania M, Lampl C, Herberhold J, Steiner TJ. Poor medical care for people with migraine in Europe - evidence from the Eurolight study. J Headache Pain. 2018;19:10.
Klein C. An imperative theory of pain. J Philos. 2007;104:517–32.
Lipton RB, Stewart WF, Stone AM, Láinez MJA, Sawyer JPC. Stratified care vs step care strategies for migraine: the Disability in Strategies of Care (DISC) Study: a randomized trial. Jama. 2000;284:2599–605.
Park JW, Chu MK, Kim JM, Park SG, Cho SJ. Analysis of trigger factors in episodic migraineurs using a smartphone headache diary applications. PLoS One. 2016;11:e0149577.
Peroutka SJ. What turns on a migraine? A systematic review of migraine precipitating factors. Curr Pain Headache Rep. 2014;18:454.
Peterson M. An introduction to decision theory: Cambridge University Press; 2017.
Sarchielli P, Granella F, Prudenzano MP, et al. Italian guidelines for primary headaches: 2012 revised version. J Headache Pain. 2012;13(Suppl 2):S31–70.
Silberstein SD. Preventive migraine treatment. Continuum (Minneap Minn). 2015;21:973–89.
Steiner TJ, Antonaci F, Jensen R, Lainez MJ, Lanteri-Minet M, Valade D, et al. Recommendations for headache service organisation and delivery in Europe. J Headache Pain. 2011;12:419–26.
Steiner TJ, Gururaj G, Andree C, et al. Diagnosis, prevalence estimation and burden measurement in population surveys of headache: presenting the HARDSHIP questionnaire. J Headache Pain. 2014;15:3.
Steiner TJ, Stovner LJ, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, et al. The impact of headache in Europe: principal results of the Eurolight project. J Headache Pain. 2014;15:31.
Steiner TJ, Gobel H, Jensen R, et al. Headache service quality: the role of specialized headache centres within structured headache services, and suggested standards and criteria as centres of excellence. J Headache Pain. 2019;20:24.
Tfelt-Hansen P, Steiner TJ. Over-the-counter triptans for migraine : what are the implications? CNS Drugs. 2007;21:877–83.
Von Euler M, Keshani S, Baatz K, et al. Utilization of triptans in Sweden; analyses of over the counter and prescription sales. Pharmacoepidemiol Drug Saf. 2014;23:1288–93.
Worthington I, Pringsheim T, Gawel MJ, et al. Targeted review: medications for acute migraine treatment. Can J Neurol Sci/J Can Sci Neurol. 2015;40:S10–32.
Xu H, Han W, Wang J, Li M. Network meta-analysis of migraine disorder treatment by NSAIDs and triptans. J Headache Pain. 2016;17:113.
Ziegeler C, Brauns G, Jurgens TP, et al. Shortcomings and missed potentials in the management of migraine patients - experiences from a specialized tertiary care center. J Headache Pain. 2019;20:86.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
Funding
Open access funding provided by University of Zurich. The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article:
The study received financial support from the patient association Migraine Action Switzerland, the Swiss Headache Society, as well as Teva Pharmaceutical Ltd., Novartis and Eli Lilly (award/grant numbers are not applicable).
HP was funded by the Werner Dessauer Stiftung. (award/grant number is not applicable).
PSS received financial support from the Research Fund of the RehaClinic Group (award/grant number is not applicable).
The funding sources had no influence on the interpretation of the data, the writing of the manuscript or the decision to submit it for publication.
Author information
Authors and Affiliations
Contributions
HP analysed the data and drafted the manuscript. ARG, PSS and CA critically revised the manuscript for important intellectual content. CA initiated the study and collected the data.
Corresponding author
Ethics declarations
Competing Interests
The authors report the following conflicts of interest with respect to the research, authorship and/or publication of this article.
Dr. Pohl reports other from Teva Pharmaceutical Industries Ltd., and Eli Lilly, grants from Werner Dessauer Stiftung, outside the submitted work. Dr. Gantenbein reports personal fees from Grünenthal, Eli Lilly, Novartis and Teva Pharmaceutical Industries Ltd., outside the submitted work. Dr. Sandor reports personal fees from Novartis, personal fees from Teva Pharmaceutical Industries Ltd., personal fees from Lilly and personal fees from Almirall, outside the submitted work. Dr. Andrée has nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pohl, H., Gantenbein, A.R., Sandor, P.S. et al. A Survey on Probable and Improbable Decisions About Headache Treatment. SN Compr. Clin. Med. 2, 2245–2252 (2020). https://doi.org/10.1007/s42399-020-00556-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-020-00556-x