Abstract
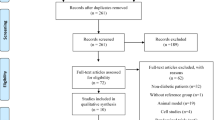
The association between circulating adropin levels and overweight/obesity is currently unclear. The aim of this study was thus to investigate and seek to determine the association between circulating adropin levels and overweight/obesity using the meta-analysis approach of observational studies. A comprehensive literature search was carried out through the PubMed, Web of Science, and SCOPUS databases to identify relevant observational studies that assessed the relationship between circulating adropin levels and overweight/obesity up to September 2020. A random-effects model was used to compute the pooled weighted mean difference (WMD) with 95% confidence intervals (CI). The meta-analysis of five studies (n = 643 participants) showed that circulating adropin levels were significantly lower in the overweight/obese vs. the normal-weight participants (WMD = − 0.96 ng/ml, 95% CI = − 1.72 to − 0.19, P = 0.01; I2 = 88.4%). In subgroup analyses, lower circulating adropin levels in obese participants compared with normal-weight were observed in Asians (WMD = − 1.58 ng/ml, 95% CI = − 1.96 to − 1.21, P < 0.001; I2 = 0.00%), and in patients with metabolic disorders (WMD = − 1.26 ng/ml, 95% CI = − 1.76 to − 0.77, P < 0.001; I2 = 44.6%), respectively. Circulating adropin levels were significantly lower in overweight/obese vs. normal-weight participants, suggesting a possible role of this hormone in the development of obesity. However, the present research indicates that further studies are needed to conclusively confirm whether adropin is a viable marker of obesity.


Similar content being viewed by others
Data availability
Data are available on request from the corresponding author.
References
Jaacks LM, Vandevijvere S, Pan A et al (2019) The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol 7:231–240. https://doi.org/10.1016/s2213-8587(19)30026-9
Aydin S (2014) Three new players in energy regulation: preptin, adropin and irisin. Peptides 56:94–110. https://doi.org/10.1016/j.peptides.2014.03.021
Kumar KG, Trevaskis JL, Lam DD et al (2008) Identification of adropin as a secreted factor linking dietary macronutrient intake with energy homeostasis and lipid metabolism. Cell Metab 8:468–481. https://doi.org/10.1016/j.cmet.2008.10.011
Kumar K, Zhang J, Gao S et al (2012) Adropin deficiency is associated with increased adiposity and insulin resistance. Obesity (Silver Spring, Md) 20:1394–1402. https://doi.org/10.1038/oby.2012.31
Choi H-N, Yim J-E (2018) Plasma adropin as a potential marker predicting obesity and obesity-associated cancer in korean patients with type 2 diabetes mellitus. J Cancer Prev 23:191
Jasaszwili M, Wojciechowicz T, Billert M et al (2019) Effects of adropin on proliferation and differentiation of 3T3-L1 cells and rat primary preadipocytes. Mol Cell Endocrinol 496:110532
O’Dowd BF, Nguyen T, Lynch KR et al (1996) A novel gene codes for a putative G protein-coupled receptor with an abundant expression in brain. FEBS Lett 394:325–329
Stein LM, Yosten GL, Samson WK (2016) Adropin acts in brain to inhibit water drinking: potential interaction with the orphan G protein-coupled receptor, GPR19. Am J Physiol-Regul Integr Comp Phys 310:R476–R480
Thapa D, Stoner MW, Zhang M et al (2018) Adropin regulates pyruvate dehydrogenase in cardiac cells via a novel GPCR-MAPK-PDK4 signaling pathway. Redox Biol 18:25–32. https://doi.org/10.1016/j.redox.2018.06.003
Hoffmeister-Ullerich SA, Süsens U, Schaller HC (2004) The orphan G-protein-coupled receptor GPR19 is expressed predominantly in neuronal cells during mouse embryogenesis. Cell Tissue Res 318:459–463. https://doi.org/10.1007/s00441-004-0948-9
Rao A, Herr DR (2017) G protein-coupled receptor GPR19 regulates E-cadherin expression and invasion of breast cancer cells. Biochim Biophys Acta Mol Cell Res 1864:1318–1327. https://doi.org/10.1016/j.bbamcr.2017.05.001
Nergiz S, Altinkaya SO, Kurt Ömürlü İ et al (2015) Circulating adropin levels in patients with endometrium cancer. Gynecol Endocrinol 31:730–735
Yosaee S, Khodadost M, Esteghamati A et al (2017) Metabolic syndrome patients have lower levels of adropin when compared with healthy overweight/obese and lean subjects. Am J Mens Health 11:426–434. https://doi.org/10.1177/1557988316664074
Zang H, Jiang F, Cheng X et al (2018) Serum adropin levels are decreased in Chinese type 2 diabetic patients and negatively correlated with body mass index. Endocr J 65:685–691
Butler AA, Tam CS, Stanhope KL et al (2012) Low circulating adropin concentrations with obesity and aging correlate with risk factors for metabolic disease and increase after gastric bypass surgery in humans. J Clin Endocrinol Metab 97:3783–3791
Sayın O, Tokgöz Y, Arslan N (2014) Investigation of adropin and leptin levels in pediatric obesity-related nonalcoholic fatty liver disease. J Pediatr Endocrinol Metab 27:479–484
Bousmpoula A, Kouskouni E, Benidis E et al (2018) Adropin levels in women with polycystic ovaries undergoing ovarian stimulation: correlation with lipoprotein lipid profiles. Gynecol Endocrinol 34:153–156
Topuz M, Celik A, Aslantas T et al (2013) Plasma adropin levels predict endothelial dysfunction like flow-mediated dilatation in patients with type 2 diabetes mellitus. J Investig Med 61:1161–1164
Inal ZO, Erdem S, Gederet Y et al (2018) The impact of serum adropin and ischemia modified albumin levels based on BMI in PCOS. Endokrynol Pol 69:135–141. https://doi.org/10.5603/EP.a2018.0002
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34
Wells GA, Shea B, O’Connell D et al (2000) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford
Egger M, Davey-Smith G, Altman D (2008) Systematic reviews in health care: meta-analysis in context. Wiley
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Egger M, Smith GD, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Chen R-M, Yuan X, Ouyang Q et al (2019) Adropin and glucagon-like peptide-2 are associated with glucose metabolism in obese children. World J Pediatr 15:565–571
Guillemot-Legris O, Mutemberezi V, Cani PD et al (2016) Obesity is associated with changes in oxysterol metabolism and levels in mice liver, hypothalamus, adipose tissue and plasma. Sci Rep 6:1–11
Kalaany NY, Gauthier KC, Zavacki AM et al (2005) LXRs regulate the balance between fat storage and oxidation. Cell Metab 1:231–244
Wu L, Fang J, Chen L et al (2014) Low serum adropin is associated with coronary atherosclerosis in type 2 diabetic and non-diabetic patients. Clin Chem Lab Med 52:751–758
Bozic J, Borovac JA, Galic T et al (2018) Adropin and inflammation biomarker levels in male patients with obstructive sleep apnea: a link with glucose metabolism and sleep parameters. J Clin Sleep Med 14:1109–1118. https://doi.org/10.5664/jcsm.7204
Brnić D, Martinovic D, Zivkovic PM et al (2020) Serum adropin levels are reduced in patients with inflammatory bowel diseases. Sci Rep 10:1–9
Trayhurn P, Wood IS (2004) Adipokines: inflammation and the pleiotropic role of white adipose tissue. Br J Nutr 92:347–355
Kuloglu T, Aydin S (2014) Immunohistochemical expressions of adropin and ınducible nitric oxide synthase in renal tissues of rats with streptozotocin-ınduced experimental diabetes. Biotech Histochem 89:104–110
Chen S, Zeng K, Liu Q-c et al (2017) Adropin deficiency worsens HFD-induced metabolic defects. Cell Death Dis 8:e3008
Hu W, Chen L (2016) Association of serum adropin concentrations with diabetic nephropathy. Mediat Inflamm 2016:1–5
Redman LM, Ravussin E (2009) Endocrine alterations in response to calorie restriction in humans. Mol Cell Endocrinol 299:129–136. https://doi.org/10.1016/j.mce.2008.10.014
Lian W, Gu X, Qin Y et al (2011) Elevated plasma levels of adropin in heart failure patients. Intern Med 50:1523–1527
Funding
This work was funded by the Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Author information
Authors and Affiliations
Contributions
SS conceived and designed the study; SS and SY conducted a systematic search, screened articles, and selected eligible articles; SS and RKM extracted the information from eligible studies and performed quality assessments; SS and ShA performed analyses and interpreted the results; SS, RKM, SY, SA, and SA wrote the first draft of the manuscript; CC edited the manuscript; and SA critically revised the manuscript and is the guarantor. All authors have read and approved the final manuscript. All authors had full access to all the data and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Soltani, S., Kolahdouz-Mohammadi, R., Aydin, S. et al. Circulating levels of adropin and overweight/obesity: a systematic review and meta-analysis of observational studies. Hormones 21, 15–22 (2022). https://doi.org/10.1007/s42000-021-00331-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-021-00331-0