Key summary points
To investigate potential factors associated with medication adherence in the older and chronic population through a PRISMA systematic review of qualitative studies on patients’ experience.
AbstractSection FindingsThe main barriers and facilitators of non-adherence were found to be patients’ beliefs about polypharmacy and drug prioritization, patient’s experience and capabilities, prescriber-patient relationship, health literacy, treatment characteristics and complexity, family and social support.
AbstractSection MessageThe present findings, derived from two well-established theoretical frameworks (ABC Taxonomy, Three Factor model) and stemming from the patient’s narratives, may provide healthcare professionals with practical information to enhance medication adherence in clinical practice.
Abstract
Purpose
Medication non-adherence represents a socially relevant challenge, particularly when interlinked to multiple chronic diseases and polypharmacy. Non-adherence rates affect treatment efficacy and increase health care costs. The aim of the study was to identify factors influencing medication adherence in the older adults through a systematic review of qualitative studies on patients’ experience.
Methods
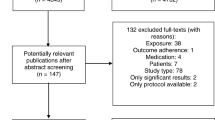
Two electronic databases were searched for qualitative studies on medication adherence in chronic diseases (hypertension, heart disease, COPD, asthma) involving people aged 65 + . The systematic review was performed according to the PRISMA statement guidelines, employing theoretical frameworks of the ABC Taxonomy of patient adherence and Three Factor model of determinants of behaviour.
Results
The initial database search identified 1234 records, of which 39 studies were considered eligible. Most of the studies focused on hypertension and were conducted in English-speaking countries. According to the ABC Taxonomy, Persistence and Implementation were the most often considered phases. Considering the Three Factor model, the most often reported themes were Information and Strategies upon being adherent. Stemming from the review findings and the patients’ narratives, a new integrated model was proposed. It reports the patient’s decisional flowchart describing barriers and facilitators (personal, social and environmental) to adherence.
Conclusion
Medication adherence is a complex and multifaceted process. The implementation of theoretical frameworks along with a patient-centred perspective may provide clinicians with useful suggestions for clinical practice, enhancing the patient’s ability to adhere.


Similar content being viewed by others
References
United Nations, Department of Economic and Social Affairs, Population Division (2017) World population ageing 2017—highlights (ST/ESA/SER.A/397). https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2017_Highlights.pdf. Accessed 29 November 2018.
Yarnall AJ, Sayer AA, Clegg A, Rockwood K, Parker S, Hindle JV (2017) New horizons in multimorbidity in older adults. Age Ageing 46(6):882–888
Onder G, Bonassi S, Abbatecola AM, Folino-Gallo P, Lapi F, Marchionni N, Pani L, Pecorelli S, Sancarlo D, Scuteri A, Trifirò G, Vitale C, Zuccaro SM, Bernabei R, Fini M, Geriatrics Working Group of the Italian Medicines Agency (2014) High prevalence of poor quality drug prescribing in older individuals: a nationwide report from the Italian Medicines Agency (AIFA). J Gerontol A Biol Sci Med Sci 69(4):430–437
Midão L, Giardini A, Menditto E, Kardas P, Costa E (2018) Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch Gerontol Geriatr 78:213–220
Aslani P, Ahmed R, Alves da Costa F (2019) The Role of Adherence in Pharmaceutical Care. In: Alves da Costa F, van Mil J, Alvarez-Risco A (eds) The Pharmacist Guide to Implementing Pharmaceutical Care. Springer, Berlin
Sabaté E (ed) (2003) Adherence to long-term therapies: evidence for action. World Health Organization, Geneva
Pagès-Puigdemont N, Mangues MA, Masip M, Gabriele G, Fernández-Maldonado L, Blancafort S, Tuneu L (2016) Patients’ perspective of medication adherence in chronic conditions: a qualitative study. Adv Ther 33(10):1740–1754
Cutler RL, Fernandez-Llimos F, Frommer M, Benrimoj C, Garcia-Cardenas V (2018) Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open 8(1):e016982
Davies EA, Omahony MS (2015) Adverse drug reactions in special populations—the elderly. Br J Clin Pharmacol 80(4):796–807
Costa E, Giardini A, Monaco A (eds) (2017) Adherence to medical plans for active and healthy ageing. Nova Science Editors, New York
Pasina L, Brucato AL, Falcone C, Cucchi E, Bresciani A, Sottocorno M, Taddei GC, Casati M, Franchi C, Djade CD, Nobili A (2015) Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging 31(4):283–289
Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, Dobbels F, Fargher E, Morrison V, Lewek P, Matyjaszczyk M, Mshelia C, Clyne W, Aronson JK, Urquhart J (2012) ABC project team. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 73(5):691–705
Vrijens B, Kardas P (2017) The ABCs of medication adherence. In: Costa E, Giardini A, Monaco A (eds) Adherence to medical plans for active and healthy ageing. Nova Science Editors, New York, pp 1–11
DiMatteo MR, Haskard-Zolnierek KB, Martin LR (2019) Improving patient adherence: a three-factor model to guide practice. Health Psychol Rev 6(1):74–91
Maffoni M, Giardini A (2017) Qualitative studies on medication adherence: what do they add to knowledge gained by quantitative methods? In: Costa E, Giardini A, Monaco A (eds) Adherence to medical plans for active and healthy ageing. Nova Science Editors, New York, pp 75–102
Giardini A, Maffoni M, Kardas P, Costa E (2018) A cornerstone of healthy aging: do we need to rethink the concept of adherence in the elderly? Patient Prefer Adher 2018(12):1003–1005
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
United Nations Development Programme (2019) Human development indicators and indices: 2018 Statistical Update. 2018; New York. https://hdr.undp.org/en/2018-update. Accessed 7 January 2019.
Ogedegbe G1, Harrison M, Robbins L, Mancuso CA, Allegrante JP (2004) Barriers and facilitators of medication adherence in hypertensive African Americans: a qualitative study. Ethn Dis 14(1):3–12
Svensson S, Kjellgren KI, Ahlner J, Säljö R (2000) Reasons for adherence with antihypertensive medication. Int J Cradiol 76:157–163
Singh JA, Herbey I, Bharat A, Dinnella JE, Pullman-Mooar S, Eisen S, Ivankova N (2017) Gout self-management in African–American veterans: a qualitative exploration of challenges and solutions from patients’ perspectives. Arthrs Care Res 69(11):1724–1732
Tolmie EP, Lindsay GM, Kerr SM, Brown MR, Ford I, Gaw A (2003) Patients’ perspectives on statin therapy for treatment of hypercholesterolaemia: a qualitative study. Eur J Cardiovasc Nurs 2(2):141–149
George M, Freedman TG, Norfleet AL, Feldman HI, Apter AJ (2003) Qualitative research-enhanced understanding of patients’ beliefs: results of focus groups with low-income, urban, African American adults with asthma. J Allergy Clin Immunol 111(5):967–973
Williams B, Shaw A, Durrant R, Crinson I, Pagliari C, De Lusignan S (2005) Patient perspectives on multiple medications versus combined pills: a qualitative study. QJM Mon J Assoc Physicians 98(12):885–893
Sale JEM, Gignac M, Hawker G (2006) How, “bad” does the pain have to be? A qualitative study examining adherence to pain medication in older adults with osteoarthritis. Arthr Rheum 55(2):272–278
Reid M, Clark A, Murdoch DL, Morrison C, Capewell S, Mcmurray J (2006) Patients strategies for managing medication for chronic heart failure B. Int J Cardiol 109:66–73
Elliott RA, Ross-Degnan D, Adams AS, Safran DG, Soumerai SB (2007) Strategies for coping in a complex world: adherence behavior among older adults with chronic illness. J Gen Intern Med 22(6):805–810. https://doi.org/10.1007/s11606-007-0193-5
Gordon K, Smith F, Dhillon S (2007) Effective chronic disease management: Patients’ perspectives on medication-related problems. Patient Educ Couns 65(3):407–415
Chen C, Wu J (2007) A model of medication-taking behavior in elderly individuals with chronic disease. J Cardiovasc Nurs 22(5):359–365
Williams AF, Manias E, Walker R (2008) Adherence to multiple, prescribed medications in diabetic kidney disease: a qualitative study of consumers’ and health professionals’ perspectives. Int J Nurs Stud 45(12):1742–1756
Williams AF, Manias E, Walker R (2009) The role of irrational thought in medicine adherence: People with diabetic kidney disease. J Adv Nurs 65(10):2108–2117
Lubaki JF, Mabuza L, Ndimande JV (2009) Reasons for non-compliance among patients with hypertension at Vanga hospital, Bandundu province, Democratic Republic of Congo: a qualitative study. Afr J Prim Heal Care Fam Med Artic 1(1):107–111
Rifkin DE, Laws MB, Rao M, Balakrishnan VS, Sarnak MJ, Wilson IB (2010) Medication adherence behavior and priorities among older adults with CKD: a semistructured interview study. Am J Kidney Dis 56(3):439–446
Lewis LM, Askie P, Randleman S, Shelton-Dunston B (2010) Medication adherence beliefs of community-dwwlling hypertensive African Americans. J Cardiovasc Nurs 25(3):199–206
Pascucci MA, Leasure AR, Belknap DC, Kodumthara E (2010) Situational Challenges That Impact health adherence in vulnerable populations. J Cult Divers. 17(1):4–12
Tsiantou V (2010) Factors affecting adherence to antihypertensive medication in Greece: results from a qualitative study. Patient Prefer Adher 4:335–343
Mishra SI, Gioia D, Childress S, Barnet B, Ramothea LW (2011) Adherence to medication regimens among low-income patients with multiple comorbidities. Heal Soc Work 36(4):249–258
Henriques MA, Costa MA, Cabrita J (2012) Adherence and medication management by the elderly. J Clin Nurs 21(21–22):3096–3105
Anthony H, Valinsky L, Inbar Z, Gabriel C, Varda S (2012) Perceptions of hypertension treatment among patients with and without diabetes. BMC Fam Pract 13:24
Stamer M, Schmacke N, Richter P (2013) Noncompliance: a never-ending story. understanding the perspective of patients with rheumatoid arthritis. Forum Qual Soc Res 14(3). https://www.qualitative-research.net/index.php/fqs/article/view/1932/3566. Accessed 15 December 2018.
Bryant L, Martini N, Chan J et al (2013) Could the polypill improve adherence? The patient perspective. J Prim Health Care 5(1):28–35
Holt EW, Rung AL, Leon KA, Firestein C, Krousel-Wood M (2014) Medication adherence in older adults: a qualitative study. Educ Gerontol 40(3):198–211
Fix GM, Cohn ES, Solomon JL et al (2014) The role of comorbidities in patients’ hypertension self-management. Chronic Illn 10(2):81–92
Odusola AO, Hendriks M, Schultsz C et al (2014) Perceptions of inhibitors and facilitators for adhering to hypertension treatment among insured patients in rural Nigeria: a qualitative study. BMC Health Serv Res 14(1):1–16
Legido-Quigley H, Lopez PAC, Balabanova D et al (2015) Patients’ knowledge, attitudes, behaviour and health care experiences on the prevention, detection, management and control of hypertension in Colombia: a qualitative study. PLoS ONE 10(4):1–16
Rahmawati R, Bajorek B (2016) Perspectives on antihypertensive medication: a qualitative study in a rural Yogyakarta province in Indonesia. Drugs Ther Perspect 32(2):76–83
Marin NS, dos Santos MF, dos Moro AS (2016) Perception of hypertensive patients about their non-adherence to the use of medication. Rev da Esc Enferm 50:59–64
Pagès-Puigdemont N, Mangues MA, Masip M et al (2016) Patients’ perspective of medication adherence in chronic conditions: a qualitative study. Adv Ther 33(10):1740–1754
Brandstetter S, Hertig S, Loss J, Ehrenstein B, Apfelbacher C (2016) The lesser of two evils—views of persons with rheumatoid arthritis on medication adherence: a qualitative study. Psychol Heal 31(6):675–692
Gibson G (2016) Signposts on the journey; medication adherence and the lived body in men with Parkinson’s disease. Soc Sci Med 152:27–34
Kassavou A, Sutton S (2017) Reasons for non-adherence to cardiometabolic medications, and acceptability of an interactive voice response intervention in patients with hypertension and type 2 diabetes in primary care: a qualitative study. BMJ Open 7(8):e015597
Abel WM, Joyner JS, Cornelius JB, Greer DB (2017) Self-care management strategies used by black women who self-report consistent adherence to antihypertensive medication. Patient Prefer Adher 11:1401–1412
Dalvi V, Mekoth N (2017) Patient non-adherence: an interpretative phenomenological analysis. Int J Health Care Qual Assur 30(3):274–284
Gebrezgi MT, Trepka MJ, Kidane EA (2017) Barriers to and facilitators of hypertension management in Asmara, Eritrea: patients’ perspectives. J Health Popul Nutr 36(1):11
Lewis LM (2011) Medication adherence and spiritual perspectives among African American older women with hypertension. J Pers Soc Psychol 1(1):1188–1197
Benson J, Britten N (2017) What effects do patients feel from their antihypertensive tablets and how do they react to them? Qualitative analysis of interviews with patients. Fam Pract 23(1):80–87
Rahmawati R, Bajorek B (2017) Understanding untreated hypertension from patients’ point of view: a qualitative study in rural Yogyakarta province, Indonesia. Chronic Illn. 0(0):1–13.
Couto JE, Panchal JM, Lal LS, Bunz TJ, Maesner JE, O’Brien T, Khan T (2014) Geographic variation in medication adherence in commercial and Medicare part D populations. J Manag Care Pharm 20(8):834–842
Dalstra JA, Kunst AE, Borrell C, Breeze E, Cambois E, Costa G, Geurts JJ, Lahelma E, Van Oyen H, Rasmussen NK, Regidor E, Spadea T, Mackenbach JP (2005) Socioeconomic differences in the prevalence of common chronic diseases: an overview of eight European countries. Int J Epidemiol 34(2):316–326
Salem H, Hasan DM, Eameash A, El-Mageed HA, Hasan S, Ali R (2018) Worldwide prevalence of hypertension: a pooled meta-analysis of 1670 studies in 71 countries with 29.5 million participants. J Am Coll Cardiol. 71(11):A1819
Arima H, Barzi F, Chalmers J (2011) Mortality patterns in hypertension. J Hypertens 29(Suppl):3–7
Zhou D, Xi B, Zhao M, Wang L, Veeranki SP (2018) Uncontrolled hypertension increases risk of all-cause and cardiovascular disease mortality in US adults: the NHANES III linked mortality study. Sci Rep 8(1):9418
Meyer D, Leventhal H, Gutmann M (1985) Common-sense models of illness: the example of hypertension. Health Psychol 4(2):115–135
Hekler EB, Lambert J, Leventhal E, Leventhal H, Jahn E, Contrada RJ (2008) Commonsense illness beliefs, adherence behaviors, and hypertension control among African Americans. J Behav Med 31(5):391–400
Del Castillo A, Godoy-izquierdo D, Vázquez ML, Godoy JF (2013) Illness beliefs about hypertension among non-patients and healthy relatives of patients. Health 5(4):47–58
McQuaid EL, Landier W (2018) Cultural issues in medication adherence: disparities and directions. J Gen Intern Med 33(2):200–206
Still CH, Ferdinand KC, Ogedegbe G, Wright JT Jr (2015) Recognition and management of hypertension in older persons: focus on African Americans. J Am Geriatr Soc 63(10):2130–2138
Musemwa N, Gadegbeku CA (2017) Hypertension in African Americans. Curr Cardiol Rep 19:129–140
Hammersley M (1992) Deconstructing the qualitative-quantitative divide 1. In: Brannen J (ed) Mixing methods: qualitative and quantitative research. Avebury, Aldershot, pp 39–55
Pierobon A, Covini E, Callus E (2017) Enhancing patient adherence through integrated educational programs based on psychological techniques and practices. In: Costa E, Giardini A, Monaco A (eds) Adherence to medical plans for active and healthy ageing. Nova Science Editors, New York, pp 129–147
Pierobon A, Giardini A, Majani G, Callegari S, Lenta F, La Rovere MT, Febo O (2009) Into the cognitive constructs related to adherence to treatment in CHD outpatients: the importance of accepting the disease limitations. Monaldi Arch Chest Dis 72:130–138
Touré-tillery M, Fishbach A (2014) How to measure motivation: a guide for the experimental social psychologist. Soc Personal Psychol Compass 7:328–341
Reeve J (2016) A grand theory of motivation: why not? Motiv Emot 40(1):31–35
Giardini A, Martin MT, Cahir C, Lehane E, Menditto E, Strano M, Pecorelli S, Monaco A, Marengoni A (2016) Toward appropriate criteria in medication adherence assessment in older persons: position paper. Aging Clin Exp Res 28(3):371–381
Barello S, Savarese M, Graffigna G (2015) The role of caregivers in the elderly healthcare journey: insights for sustaining elderly patient engagement. In: Graffigna G, Barello S, Triberti S (eds) Patient engagement: a consumer-centered model to innovate healthcare. De Gruiter Open, Berlin
Wagle KC, Skopelja EN, Campbell NL (2018) Caregiver-based interventions to optimize medication safety in vulnerable elderly adults: a systematic evidence-based review. J Am Geriatr Soc 66(11):2128–2135
Lemstra M, Nwankwo C, Bird Y, Moraros J (2018) Primary nonadherence to chronic disease medications: a meta-analysis. Patient Prefer Adher 12:721–731
De Geest S, Zullig LL, Dunbar-Jacob J, Helmy R, Hughes DA, Wilson IB, Vrijens B (2018) ESPACOMP medication adherence reporting guideline (EMERGE). Ann Intern Med 169(1):30–35
Funding
The present review was co-funded by the Erasmus + Programme of the European Union – Skills4Adherence- 2017–1-PL01-KA202-038672. Also, this work received financial support from FCT/MCTES (UIDB/04378/2020).
Author information
Authors and Affiliations
Contributions
MM, ST and AG performed the revision of the literature, providing substantial input and drafting and reviewing the manuscript. An overall supervision to the reviewing procedure (both of the literature and of the manuscript) was finalized by PK, MK-M, LM and EC. All authors gave their final approval.
Corresponding author
Ethics declarations
Conflict of interest
PK received speaker’s honoraria from Aflofarm, Fresenius, Polpharma and Sandoz; and got funding from a grant from European Union’s Health Programme (2014–2020) for SIMPATHY project (663082), outside this work, and The European Commission ERASMUS + Project Skills4Adherence (Grant Agreement Number: 2017-1-PL01-KA202-038672). The other authors declare no conflict of interest.
Ethical approval
Ethical approval was not required as the study is based on data retrieved from already published studies.
Informed consent
For a literature review, written consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maffoni, M., Traversoni, S., Costa, E. et al. Medication adherence in the older adults with chronic multimorbidity: a systematic review of qualitative studies on patient’s experience. Eur Geriatr Med 11, 369–381 (2020). https://doi.org/10.1007/s41999-020-00313-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-020-00313-2