Abstract
Background
Parkinson’s disease is still incurable, and several factors are considered when defining pharmacological therapy.
Objective
The aim of this study was to describe the prescription pattern of monoamine oxidase B inhibitors (MAO-BIs) marketed in Italy (selegiline, rasagiline, safinamide) as an add-on to levodopa among new users of MAO-BIs, from the perspective of the Italian National Health Service.
Patients and Methods
Through cross-linkage of administrative healthcare data in the Ricerca e Salute (ReS) database, adults with a supply of one or more MAO-BIs in 2017, and with no other MAO-BI use since 2013, were selected. Levodopa had to be supplied within 30 days before/after the MAO-BI. The incidence, use, sex, age, comorbidities, 2-year prescription patterns (i.e., switches, proportion of treated patients per semester/year, mean daily milligrams/monthly tablets supplied, discontinuation, change to other anti-Parkinson drug) of patients taking MAO-BIs were provided.
Results
In 2017, 1059 new users received an MAO-BI (incidence 22.6 × 100,000 adults) combined with levodopa: 502 subjects (10.7 × 100,000) were treated with selegiline, 161 (3.4 × 100,000) were treated with rasagiline, and 396 (8.4 × 100,000) were treated with safinamide. The cohorts mainly consisted of males with a median age of ≥ 74 years. Treatment incidences increased with age. Switches occurred in 18.0%, 11.0%, and 4.3% of the selegiline, rasagiline, and safinamide cohorts, respectively. Most of the patients switching from selegiline/safinamide changed to rasagiline, while most of the patients switching from rasagiline changed to safinamide. From the first to second years, patient numbers reduced by ≤ 50%, and the daily milligrams/monthly tablets slightly increased. Six-month discontinuation occurred in > 50% of all cohorts, and ≥ 65% of discontinuing patients changed to another anti-Parkinson drug.
Conclusions
This analysis described the heterogeneous use of MAO-BIs as an add-on to levodopa in Italy. Further clinical trials and real-world studies are encouraged to update the few existing guidelines and to align clinical practice strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This retrospective observational analysis of the pharmaco-utilization of monoamine oxidase B inhibitors (MAO-BIs) combined with levodopa in new users of MAO-BIs updates the real-world evidence regarding add-on therapy for Parkinson’s disease in Italy. |
In 2017, selegiline combined with levodopa was the most prescribed formulation, followed by safinamide and rasagiline. Switching to safinamide occurred most frequently in patients treated with rasagiline. Furthermore, the majority of patients switching from selegiline and rasagiline changed to safinamide. Discontinuation was very frequent within the selegiline cohort and 21–35% of discontinuing patients did not change to another anti-Parkinson drug. |
This study demonstrates a very heterogeneous therapeutic approach, which could be improved by more evidence about the combined strategies and the possibility of switching between MAO-BIs, and by training and updating practitioners, especially on the risks of adverse events. |
1 Introduction
Parkinson’s disease (PD) is a neurodegenerative disorder whose progressive loss of dopaminergic neurons in the substantia nigra has been the most agreed upon etiology to date. It is defined by typical motor and non-motor manifestations causing disability and reduced quality of life [1]. Even if its early phase is often characterized by non-motor symptoms [2], the diagnosis is still essentially based on clinical assessment [3]. Currently, PD is incurable because the available therapies have been demonstrated to only mitigate motor/non-motor fluctuations and not to have a disease-modifying action [4]. Clinicians should take into account several factors when they set-up the pharmacological therapy [5]. Interestingly, since PD is an age-dependent disorder, age was the most important determinant of prescription choice until the latest National Institute for Health and Care excellence (NICE) guidelines [6], which considered the impact of motor/non-motor symptoms on life quality as the first criterion when choosing the starting treatment, to allow a more personalized pharmacological scheme [7]. Given the increasing availability of pharmacological agents for PD and the recent evidence on the benefits of the early use of levodopa, despite concerns about dyskinesias induced by its monotherapy at a dosage higher than 400 mg/day, the debate on the most appropriate first-line therapeutic approach (levodopa alone or combined with dopamine-sparing agents) is still ongoing [8]. Nevertheless, the frequent development of motor symptoms after a few years from the beginning of levodopa monotherapy inevitably leads many clinicians to add a drug able to improve motor fluctuations and ideally reduce dyskinesias [9]. These are catechol-O-methyltransferase (COMT) inhibitors, dopamine agonists (DAs), and monoamine oxidase B inhibitors (MAO-BIs). The latter are selegiline and rasagiline, used as monotherapy or as add-on to levodopa, and the most recent, safinamide, which is recommended only in association with levodopa (and other dopamine-sparing agents, if needed). Safinamide, differently from the others, has recently demonstrated its efficacy on non-motor symptoms (e.g. pain, sleep disturbances/daytime sleepiness, depression) [10,11,12]. Moreover, a Welsh population-based study has reported its use as first choice for patients whose non-motor conditions affect their quality of life [8]. According to the official Italian drug consumption report, shortly after the beginning of safinamide reimbursement (February 2016), a change in the prescription pattern of MAO-BIs has been observed [13]. In order to assess this new therapeutic paradigm, few real-world data analyses on prescription patterns of MAO-BIs as add-on therapies to levodopa in patients affected by PD have been carried out [2, 8, 14], especially in Italy [4].
This real-world observational retrospective analysis aimed to describe, from the perspective of the Italian National Health Service (INHS), the prescription pattern of the MAO-BIs marketed in Italy (i.e. selegiline, rasagiline, and safinamide) supplied in association with levodopa among new MAO-BI users between 2017 and 2019.
2 Materials and Methods
2.1 Data Source
This study was performed by analyzing the database of Fondazione Ricerca e Salute (ReS), which has already been used for several observational research studies regarding different clinical fields [15,16,17]. Fondazione ReS is a non-profit foundation working on real-world healthcare data with the aim of creating useful tools for planning and monitoring healthcare policy issues at various levels and for different stakeholders. In collaboration with Cineca (Interuniversity Consortium; https://www.cineca.it/en), which guarantees the quality and safety of data management through international standard certifications, the ReS database routinely collects and integrates healthcare administrative data (demographics, pharmaceuticals, hospitalizations, outpatient specialist services) that come from some Italian Local and Regional Health Authorities under specific agreements and are periodically sent to the Italian Ministry of Health for reimbursement purposes. The pharmaceutical database consists of all drugs reimbursed by the INHS and supplied from both local and hospital pharmacies. Analyses are based on the marketing code, the Anatomical Therapeutic Chemical (ATC) classification, established by the World Health Organization (WHO) to support worldwide drug use monitoring [18], dose (milligrams), number of packs, and dispensing date. The hospitalization database is composed of in-hospital diagnoses and procedures, according to the Italian version of the International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM), 2007 [19], recorded in hospital discharge forms of both ordinary and daily hospitalizations. The outpatient specialist care database comprises examinations, diagnostics, and invasive/non-invasive procedures supplied by the INHS, and is analyzed based on the current national classification system. All these databases also include the costs paid by the INHS for the healthcare services provided. This study originates from the cross-linkage of the aforementioned healthcare administrative databases, based on a unique anonymized identity number per patient. Ethical approval was not sought for the present study because demographics were completely anonymized, according to the current privacy regulations, and the analysis was conducted for institutional purposes, in agreement with local and regional health authorities.
2.2 Cohort Selection
Starting with the ReS database, we selected adults analyzable from 2013 to 2019 and with at least one supply, in 2017, of one MAO-BI, among selegiline (ATC code: N04BD01), rasagiline (N04BD02) and safinamide (N04BD03). The least recent filled prescription date of an MAO-BI was considered the index date. In order to exclusively identify new users of MAO-BIs in 2017, patients with even just one supply of an MAO-BI (N04BD) within the period preceding the index date until 2013 were excluded. Since the fixed combination of MAO-BI and levodopa does not exist, the simultaneous dispensation of the two was ascertained by the filled prescription of levodopa (N04BA02, N04BA03, and N04BA05) within 30 days before or after the MAO-BI dispensation. The three following cohorts were analyzed:
-
patients treated with selegiline and levodopa;
-
patients treated with rasagiline and levodopa;
-
patients treated with safinamide and levodopa.
This analysis was limited to MAO-BIs and did not include new users of the other anti-PD drugs, in order to describe the real-world use of this specific class starting from about 1 year after the beginning of safinamide reimbursement by the INHS in February 2016.
2.3 Epidemiological and Clinical Characterization
On the index date, the characterization and MAO-BI treatment incidence of the cohorts were provided by sex and age. The presence of comorbidities of interest (coronary artery disease [CAD], heart failure, diabetes, dyslipidemia, depression, chronic lung disease, artery hypertension, chronic kidney disease, liver disease) from 2013 were assessed. For the identification criteria of comorbidities, see electronic supplementary Table 1.
2.4 Prescription Patterns of Monoamine Oxidase B Inhibitors (MAO-BIs)
In order to describe the prescription patterns of MAO-BIs, each patient in the cohorts was analyzed within a 2-year follow-up period, at the latest up to 31 December 2019 from the index date.
2.4.1 Length of Levodopa Therapy
Each patient in the three cohorts with at least one supply of levodopa (N04BA02, N04BA03, N04BA05) in the fourth year before the index date was considered to be receiving treatment with levodopa since 2013 at least.
2.4.2 Therapy Switch
The first switch from the index MAO-BI to another MAO-BI during the follow-up period was recorded. The number of patients switching and the average time from the index date to the switch was given.
2.4.3 Treatment Coverage and Consumption of MAO-BIs
This analysis was performed exclusively on patients who did not change their index MAO-BI during the observational period. After having divided both follow-up years into semesters, patients with at least one supply of MAO-BIs in each semester were identified, and the percentage of subjects in the cohort per semester/year defined the ‘coverage’.
Moreover, mean consumption was analyzed in terms of daily milligrams and monthly supplied tablets according to the summaries of product characteristics [20,21,22] for the minimum starting doses, and the common clinical practice (based on case-by-case recommendations) for the maintenance doses. Specifically, drug consumption was analyzed for the different follow-up periods (i.e. semester and year), by MAO-BI, as follows.
-
Selegiline If the mean daily dose was 5 mg during the first year and 10 mg during the second year, and, accordingly, if at least 30 tablets per month were supplied in the first and second years.
-
Rasagiline If the mean daily dose was 1 mg and 30 tablets per month were dispensed, both in the first and second years.
-
Safinamide If the mean daily dose was 50 mg during the first year and, potentially, 100 mg in the second year (the choice of increasing the dose is generally made on a case-by-case); since both doses are marketed in 30-tablet packs, the monthly supply had to be 30 units.
2.4.4 Discontinuation of MAO-BIs
Among patients who did not change their MAO-BI, discontinuation of the index MAO-BIs was defined by the absence of further supplies within at least 90 days after the last free filled prescription. Among discontinuing patients and within 30 days before and after the last dispensation, supplies of other anti-PD drugs, such as levodopa (N04BA02, N04BA03, N04BA05), DAs (N04BC04, ropinirole; N04BC05, pramipexole; N04BC07, apomorphine; N04BC09, rotigotine) and COMT inhibitors (N04BX01, tolcapone; N04BX02, entacapone; N04BX04, opicapone) were searched.
2.5 Statistical Analyses
Generally, when administrative data are analyzed, the number of patients/events is so large that even minimal differences will result in a conventional level of statistical significance (5%), often without a corresponding and convincing level of clinical significance. For this reason, we have avoided the use of detailed p-values and have described nominal differences. Proportions are expressed as percentages. Statistical analyses were performed using Oracle SQL Developer, Italian version 18.1.0.095 (Los Angeles, CA, USA).
3 Results
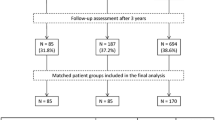
Among more than 5 million adults in the ReS database for 2017, 4,691,582 were analyzable from 2013 (Fig. 1). Among these adults, 4734 patients were treated with an MAO-BI combined with levodopa. Of these, there were 1059 new MAO-BI users (incidence 22.6 × 100,000): 502 subjects (incidence 10.7 × 100,000 adults) were treated with selegiline, 161 (3.4 × 100,000) were treated with rasagiline, and 396 (8.4 × 100,000) were treated with safinamide (Fig. 1). All cohorts mostly comprised males and elderly subjects (Table 1). The treatment incidence increased with age for all groups, reaching a peak at 70–79 years for the rasagiline and safinamide cohort and ≥80 years for the selegiline cohort. About 70% of new MAO-BI users were affected by arterial hypertension and more than 40% suffered from depression, while lower frequencies were found for chronic lung diseases, diabetes, and dyslipidemia (Table 1).
3.1 Prescription Patterns of MAO-BIs
3.1.1 Length of Levodopa Therapy
The search for levodopa treatment in the fourth year before the index date yielded a total of 121 patients in the selegiline cohort (24.1%), 40 patients in the rasagiline cohort (24.8%), and 223 patients in the safinamide cohort (56.3%) who were treated with levodopa for at least 4 years.
3.1.2 Therapy Switch
The switch to another MAO-BI mostly occurred in the rasagiline cohort (18.0%), followed by patients treated with selegiline (11.0%) and those treated with safinamide (4.3%) (Table 2). The majority of subjects switching from selegiline (56.4%) and safinamide (64.7%) changed to rasagiline, while 72.4% of those switching from rasagiline changed to safinamide. On average, the switch occurred after 12 months from the index date.
Of those patients treated with the same MAO-BI during the follow-up period, the coverage and discontinuation of the index MAO-BI were analyzed (Table 2).
3.1.3 Treatment Coverage and Consumption of MAO-BIs
Within the first year, 100% of all cohorts were supplied at least once with the same MAO-BI, while 47.8%, 62.7%, and 69.6% of the selegiline, rasagiline, and safinamide cohorts, respectively, were treated in the second year. By semester, the safinamide-treated cohort showed the highest coverage (percentage of patients with at least one supply). The mean monthly consumption of tablets by year tended to slightly increase, while that of the rasagiline and selegiline cohorts was as likely to be farther from the expected total amount of unit doses (30 tablets/month) than safinamide within the first and second follow-up years. Indeed, the safinamide-treated cohort showed a mean unit dose consumption close to the recommended dose during each semester and both years of follow-up (from 24.6 tablets to 29.0 of 30). In terms of mean daily dose, during the first follow-up year the selegiline and safinamide cohorts were supplied with doses consistent with the related recommended starting doses (5 mg selegiline and 50 mg safinamide). Within the second year, the mean daily consumption did not reach the expected highest dose for selegiline (6.2 vs. 10 mg), the rasagiline cohort moved slightly close to the recommended dose (0.8 vs. 1 mg), and the majority of safinamide-treated patients did not double their dose (61.9 vs. 100 mg).
3.1.4 Discontinuation of MAO-BIs
Overall, 66.7% of selegiline-treated patients (n = 447), 56.8% of rasagiline users (n = 132), and 52.8% of safinamide users (n = 379) discontinued the treatment. On average, discontinuation occurred within 6 months from the index date. A total of 65.1%, 78.7%, and 79.0% of patients discontinuing selegiline, rasagiline, and safinamide, respectively, switched to another anti-PD drug, i.e. levodopa, DAs, or COMT inhibitors. For the remaining subjects, no other supply of dopamine-sparing agents was found.
4 Discussion
To our knowledge, this is the most up-to-date analysis of the prescription patterns of MAO-BIs combined with levodopa from the perspective of the INHS, by means of administrative healthcare databases. The integration between real-world data and results from clinical trials on the PD pharmacological approach has become essential, especially because evidence on daily care settings and on unselected patients is scarce and inconsistent, and a head-to-head assessment of the prescription pattern of the three MAO-BIs has been barely considered. Moreover, descriptions of real-life drug utilization can help clinicians to compare evidence and their therapeutic approach in order to increase their knowledge and improve or confirm their habits, always aiming at the best patient care.
4.1 Cohort Selection
From the 2017 ReS database, new MAO-BI users supplied with levodopa and selegiline (10.7 × 100,000 adults) or safinamide (8.4 × 100,000) or rasagiline (3.4 × 100,000) were identified and analyzed. The ReS database can be considered reliably representative of the Italian population, based on a comparison between our age distributions and those provided by the National Institute of Statistics [23]. Other real-world studies [2, 8, 14] have provided outcomes about the prescription pattern of MAO-BIs among patients with a new diagnosis of PD and/or new users of any anti-PD drug, whereas we analyzed only new users of an MAO-BI that was combined with levodopa, whose continuous use, from a clinical point of view, was also useful to confirm the diagnosis of PD and supported the consistency of our analysis. Therefore, due to the purpose of this study, since we did not consider the overall use of MAO-BIs (i.e. also not associated with levodopa), our treatment incidence rates cannot be compared either with the literature or with the official 2017 consumption prevalence rates provided by the Italian Medicine Agency’s report, which found that safinamide was the most supplied, followed by selegiline and rasagiline [24]. Moreover, this analysis was limited to MAO-BIs and did not include new users of the other anti-PD drugs, in order to describe the real-world use of this specific class starting from approximately 1 year after the beginning of safinamide reimbursement by the INHS in February 2016. From 2017, the positioning of safinamide within the anti-PD therapeutic strategies can be considered better defined for daily clinical practice and its prescription pattern deduced by administrative data can be more reliable and better described. It is however interesting that despite the Italian restrictions to safinamide’s prescription (which follows a mandatory therapeutic plan signed by a specialist), apparently its consumption had already been prevalent since the first year of reimbursement. This could reflect the eagerness of prescribing clinicians to experiment a new promising drug, or, rather, it could have been a consequence of the beginning of the pharmaceutical marketing.
4.2 Epidemiological and Clinical Characterization
The cohorts were mostly composed of males and elderly subjects, in line with worldwide evidence [8, 14, 25]. Specifically, since PD has been ascertained to be age-dependent [3], the increasing treatment incidence with age was expected. Moreover, the selegiline cohort was the oldest, in line with literature [4, 7]. The high prevalence of comorbidities was also foreseen, due to the older age of the cohorts and the high risk for multimorbidity in patients affected by PD [26], such as cardiovascular, musculoskeletal, and mental disorders, which in turn increases the need for support, morbidity, and mortality.
4.3 Prescription Patterns of MAO-BIs
4.3.1 Length of Levodopa Therapy
Selegiline and rasagiline can also be prescribed as monotherapy in the early stages, while safinamide only combined with levodopa in the mid–late stages [1]. To date, the safety and efficacy of MAO-BIs as adjunct to levodopa have been demonstrated in the advanced phases of PD, especially through the improvement of motor fluctuations, but also showing some effect on non-motor fluctuations [1, 26]. Indeed, motor symptoms, particularly dyskinesias, tend to develop after 4–6 years from the beginning of levodopa monotherapy treatment [9]. Therefore, data about levodopa use 4 years before the MAO-BI index date suggest that one-quarter of the selegiline and rasagiline cohorts and more than half of the safinamide group likely started the MAO-BI at an advanced stage, when motor fluctuations were not controlled by levodopa alone or the addition of another dopamine-sparing agent, as recommended by the latest NICE guidelines [6]. Similarly, the proportion of selegiline and rasagiline cohorts without levodopa 4 years before the index date could be considered at a less advanced stage. This assumption could be further supported by evidence of a positive relationship between multiple anti-PD drug use and the duration of the disease [7, 27], namely its progression.
4.3.2 Therapy Switch
The switch between MAO-BIs occurred more frequently in the selegiline cohort and less frequently in the safinamide cohort. The majority of patients from both cohorts who switched changed to rasagiline. Meanwhile, more than 70% of subjects discontinuing rasagiline switched to safinamide. Switching from one MAO-BI to another allows a more personalized, effective, and well-tolerated therapy, since they have different pharmacokinetic, pharmacodynamic, and pharmacological characteristics and adverse effects [1]. In particular, rasagiline has a high bioavailability (about 39%), produces inactive metabolites (e.g., compared with selegiline’s amphetamine-like metabolites), and is generally well tolerated [1]. A pilot study evaluating the switch to rasagiline [28] provided evidence of improved motor behavior, motor complications, mood, and sleep in 30 patients affected by PD, compared with a previous selegiline treatment. Safinamide, the only reversible MAO-BI, has demonstrated higher bioavailability and selectivity but less potency than the others [1]. Moreover, its metabolites are inert, adverse events are moderate, and motor fluctuations are improved in the advanced stage along with non-motor symptoms, thanks to additional activity of glutamate release modulation [10,11,12]. Three real-world studies on the efficacy and safety of switching from an MAO-BI to safinamide have been published [29,30,31]. Two studies observing the overnight switch from rasagiline, which is not recommended by its summary of product characteristics (SPC) [21], did not find any relevant adverse events [30, 31]. In particular, Martí-Andrés and colleagues showed an improvement in motor and non-motor symptoms in 97 patients after switching to safinamide [31]. The third study retrospectively analyzed 91 subjects eligible for safinamide who switched from selegiline and rasagiline treatment, and found improvements in terms of time spent off and on with disabling dyskinesias and a significant reduction in the mean daily dose of levodopa [29]. Nevertheless, the little evidence on the switch from one MAO-BI to another should be integrated with more trials or real-world analyses in order to provide clinicians with concrete data for the most appropriate therapeutic choice, and also in light of the still high concern about the risk of adverse effects in real-world and uncontrolled conditions. The implementation of this evidence would be of particular interest for patients who need to change their selegiline treatment. Indeed, the ability of selegiline to accumulate amphetamine-like metabolites can be prolonged over time and can exacerbate adverse reactions on the nervous system even if the intake of other drugs (e.g. rasagiline) occurs after a short period (a 2-week washout period is recommended before switching to another MAO-Bi [22], as for rasagiline [21]) [1]. Furthermore, this risk could be associated with the cardiovascular risk when levodopa is combined with selegiline [1, 26]. Finally, according to our results, the average switching time calculated at 12 months from the index date could, interestingly, reflect the mean frequency of follow-up checks, which can be considered to be lower than in common clinical practice.
4.3.3 Treatment Coverage and Consumption of MAO-BIs
Within the observational period, the proportion of patients supplied with at least one MAO-BI during the second follow-up year halved for the selegiline cohort and was reduced by about 40% and 30% for the rasagiline and safinamide cohorts, respectively. Based on the consumption analysis, according to the dosing regimens defined in Sect. 2.4.3, on average subjects treated with rasagiline were likely to take a dose very close to the recommended dose (1 mg) in both follow-up years, while the selegiline and safinamide cohorts were found to be supplied with their starting doses/units. Nevertheless, despite the expectation of the dose increase of selegiline in the second year, to our knowledge this was not the same for safinamide. We can assume that the few patients in our cohort who received the 100 mg dose could be in a more advanced stage (also based on the suggestion by Martí-Andrés and colleagues) [31]. We are aware that washout periods (e.g. due to hospitalizations) are common and are not recorded in administrative databases. Therefore, a slight underestimation of coverage was inevitable. Moreover, there is extremely high heterogeneity among Italian regions in following the few existing and updated national (the LIMPE guideline was updated in 2015 [32]) and international guidelines (with particular reference to the NICE guideline updated in 2017 [6]), as an historic cohort study on Italian administrative databases has reported [4]. Moreover, it is worth mentioning that the way the coverage indicator was structured could not be considered a measurement of adherence. However, we would like to briefly discuss a very important issue related to the management of PD patients in real life, which we propose to properly address in a future analysis, in order to implement the still limited data on PD medication adherence. Indeed, it has been demonstrated that a low pharmacological drug adherence among PD patients is common and that it is a widespread phenomenon at all stages [33, 34]. It can be related to patients’ intentional and non-intentional factors [33]. Among the latter, the multimorbidity and the increasing complexity of clinical conditions, together with progression, seem the most influencing factors and are increasingly characterized by motor symptoms and severe motor and non-motor complications. Adherence is multidimensional and multifactorial, thus it is important to analyze the role of clinicians, health systems, other than the patient, the disease, and the therapy themselves [33, 35], if only because, as PD progresses, its economic burden on healthcare systems, society and patients increases [36]. In general, these findings of possible undertreatment with MAO-BIs must be carefully taken into account when assessing patients in terms of adverse events and effectiveness in daily clinical practice.
4.3.4 Discontinuation of MAO-BIs
Discontinuation rates were high (66.7%, 56.8%, and 52.8% for the selegiline, rasagiline, and safinamide cohorts, respectively) and occurred, on average, early (6 months) after the addition of an MAO-BI to levodopa. The elevated median age of the analyzed patients (74 years and older) brings multimorbidity and polypharmacotherapy, which increase the risk of interactions and adverse effects [26]. MAO-BIs are generally well tolerated, but selegiline can cause more disabling adverse events, particularly because of its amphetamine-like metabolites and antidepressant-like effects [1]. Moreover, selegiline has also shown an increased risk of cardiovascular diseases in combination with levodopa, and of gastrointestinal ulcers and bleeding in the elderly [1, 26]. Furthermore, the PD MED study found that 72% of MAO-BI users have withdrawn due to a combination of adverse effects and absence of therapy [37]. Whereas the lowest discontinuation seen for safinamide could be related to the eagerness of prescribing physicians for findings of mild to moderate adverse effects and very good safety profile, although to date assessed by only a few studies, observational or interventional against placebo or the best standard of care [1, 38,39,40,41], which have not found adverse reactions different from those stated in the SPC [20]. Given the fairly recent marketing introduction and the concomitant reimbursement authorization in Italy, up-to-date safety and efficacy evidence is definitely needed, and also against other MAO-BIs. The highest discontinuation rate among new users of selegiline in the current study can be explained by the aforementioned evidence. Nevertheless, it is worth mentioning that the Italian reimbursement criteria are not the same for all MAO-BIs. Indeed, the prescription of rasagiline and safinamide can be limited by a therapeutic drug plan signed by specialist practitioners, according to regional decisions, while selegiline cannot. At the same time, a high proportion of patients without any anti-PD therapies after MAO-BI cessation was observed. It is likely these patients could be considered lost to follow-up because they were treated during hospitalizations longer than 90 days (the in-hospital drug administration is not included in the administrative databases available to ReS), some died in outpatient settings (the ReS database recorded only in-hospital deaths), and some were transferred to residential facilities/nursing homes (not recorded in administrative databases) or moved to a region not included in the ReS database. However, the high rate of discontinuation is an important clinical issue that must be addressed during daily clinical practice.
4.3.5 Strengths and Limitations
Other limitations of this study must be mentioned. A very limited group of patients treated with MAO-BIs was selected. In Italy, these drugs are generally reimbursed by the INHS but some regions have restricted reimbursement criteria, therefore it is possible that the incidence of MAO-BI use was slightly underestimated. It might also be possible that some subjects were not recorded in administrative databases due to the private purchase of MAO-BIs or to administration of the drug during a recovery period in a nursing home or during a hospitalization. Nevertheless, the definition of new users can be considered reliable because we assessed a time span preceding the index prescription long enough to exclude potential planned washout periods. Therefore, prescription patterns were likely to reliably represent the real clinical attitudes of the Italian areas analyzed, which, in line with the Italian Medicines Agency’s 2017 drug consumption report [13], showed that clinicians preferred selegiline and safinamide to rasagiline. Interestingly, between the two older MAO-BIs, the overall preference of selegiline, despite its well-known safety profile, could have been influenced by its longer presence on the market, its easier pattern of prescription, and its lower cost. In any case, validation against clinical data is absolutely necessary, if only to stratify by disease severity, motor/non-motor symptoms, or dose, which are all hard to define through administrative databases. In particular, we did not stratify by either comorbidities or polypharmacotherapy, which are likely to drive the physician’s choice, together with the aforementioned criteria [8]. Moreover, based on the coverage assessment, we defined the cut-offs according to the summaries of product characteristics and the common clinical practice or case-by-case recommendations, but evidence for safinamide, the most recently marketed MAO-BI, is still being produced. In general, the very high country and regional healthcare system variations and the scarce and inconsistent available evidence might have caused significant heterogeneity among therapeutic strategies, which inevitably affects this type of study and limits meaningful comparisons between populations [3, 4, 7]. Finally, the definition of discontinuation was only based on pharmaceutical cut-offs, without considering specialty examinations or hospitalizations planned in the current follow-up timetable. At the same time, the high median age, absence in the ReS database of outpatient mortality, possible transfer to nursing homes or regions not included in the ReS database, and in-hospital drug administration could have led to the overestimation of discontinuation and the proportion of patients not supplied with any anti-PD drug after MAO-BI cessation.
5 Conclusions
To the best of our knowledge, this is the most up-to-date Italian study assessing the 2-year prescription pattern of MAO-BIs as add-on therapy to levodopa in new users of MAO-BIs, from the perspective of the INHS. This analysis provided a reliable picture of the treatment with MAO-BIs, in terms of demographics (i.e. higher use in males and elderly subjects with a high prevalence of cardiometabolic comorbidities and mental disorders) and prescription pattern, in light of the heterogeneous therapeutic strategies existing throughout the Italian areas included in the ReS database. Our findings confirmed high use of safinamide shortly after the beginning of its reimbursement by the INHS. Interestingly, the switch between MAO-BIs occurred with low frequency in the safinamide cohort, while, as expected, it was common in patients treated with selegiline. Moreover, given a slight increase in 2-year consumptions, the possible undertreatment highlighted among all cohorts treated with MAO-BIs must be carefully taken into account by physicians when assessing PD patients in terms of adverse events and effectiveness in daily clinical practice. Finally, high discontinuation rates and proportions of patients without any anti-PD drug after cessation of MAO-BIs combined with levodopa were observed, representing important clinical issues that must be carefully addressed by clinicians. Since, to date, PD does not have a successful disease-modifying therapy and the existing treatments must be evaluated in terms of possible combinations and individual needs, further trials, especially head-to-head trials, and real-world analysis must be encouraged worldwide in order to update and align the still highly heterogeneous therapeutic strategies.
References
Alborghetti M, Nicoletti F. Different generations of type-B monoamine oxidase inhibitors in Parkinson’s disease: from bench to bedside. Curr Neuropharmacol. 2019;17(9):861–73. https://doi.org/10.2174/1570159x16666180830100754.
Kasamo S, Takeuchi M, Ikuno M, et al. Real-world pharmacological treatment patterns of patients with young-onset Parkinson’s disease in Japan: a medical claims database analysis. J Neurol. 2019;266(8):1944–52. https://doi.org/10.1007/s00415-019-09360-7.
Riccò M, Vezzosi L, Balzarini F, et al. Prevalence of Parkinson Disease in Italy: a systematic review and meta-analysis. Acta Biomed. 2020;91(3): e2020088. https://doi.org/10.23750/abm.v91i3.9443.
Degli Esposti L, Piccinni C, Sangiorgi D, et al. Prescribing pattern and resource utilization of monoamine oxidase-B inhibitors in Parkinson treatment: comparison between rasagiline and selegiline. Neurol Sci. 2016;37(2):227–34. https://doi.org/10.1007/s10072-015-2395-7.
Oertel W, Schulz JB. Current and experimental treatments of Parkinson disease: a guide for neuroscientists. J Neurochem. 2016;139(Suppl 1):325–37. https://doi.org/10.1111/jnc.13750.
National Institute for Health and Care Excellence. Parkinson’s disease in adults. NICE guideline. London: National Institute for Health and Care Excellence; 2017.
Orayj K, Lane E. Patterns and determinants of prescribing for Parkinson’s disease: a systematic literature review. Parkinsons Dis. 2019;923:7181. https://doi.org/10.1155/2019/9237181.
Orayj K, Akbari A, Lacey A, et al. Factors affecting the choice of first-line therapy in Parkinson’s disease patients in Wales: A population-based study. Saudi Pharm J. 2021;29(2):206–12. https://doi.org/10.1016/j.jsps.2021.01.004.
Borgohain R, Szasz J, Stanzione P, et al. Two-year, randomized, controlled study of safinamide as add-on to levodopa in mid to late Parkinson’s disease. Mov Disord. 2014;29(10):1273–80. https://doi.org/10.1002/mds.25961.
Liguori C, Stefani A, Ruffini R, et al. Safinamide effect on sleep disturbances and daytime sleepiness in motor fluctuating Parkinson’s disease patients: A validated questionnaires-controlled study. Parkinsonism Relat Disord. 2018;57:80–1. https://doi.org/10.1016/j.parkreldis.2018.06.033.
Geroin C, Di Vico IA, Squintani G, et al. Effects of safinamide on pain in Parkinson’s disease with motor fluctuations: an exploratory study. J Neural Transm. 2020;127(8):1143–52. https://doi.org/10.1007/s00702-020-02218-7.
De Micco R, Satolli S, Siciliano M, et al. Effects of safinamide on non-motor, cognitive, and behavioral symptoms in fluctuating Parkinson’s disease patients: a prospective longitudinal study. Neurol Sci. 2022;43(1):357–64. https://doi.org/10.1007/s10072-021-05324-w.
Agenzia Italiana del Farmaco (2018). L'uso dei Farmaci in Italia. Rapporto Nazionale Anno; 2017.
Neo S, Wong SYA, Ng HL, et al. Evolution of Initial Pharmacologic Treatment of Newly Diagnosed Parkinson’s Disease Patients over a Decade in Singapore. Parkinsons Dis. 2020;2020:6293124. https://doi.org/10.1155/2020/6293124.
Calabria S, Ronconi G, Dondi L, et al. Patterns of prescription, hospitalizations and costs of herpes zoster in patients at risk, from a large Italian claims database. Glob Reg Health Technol Assess. 2020;7(1):66–71. https://doi.org/10.33393/grhta.2020.2026.
Maggioni AP, Dondi L, Andreotti F, et al. Four-year trends in oral anticoagulant use and declining rates of ischemic stroke among 194,030 atrial fibrillation patients drawn from a sample of 12 million people. Am Heart J. 2020;220:12–9. https://doi.org/10.1016/j.ahj.2019.10.017.
Piccinni C, Cevoli S, Ronconi G, et al. Insights into real-world treatment of cluster headache through a large Italian database: prevalence, prescription patterns, and costs. Expert Rev Clin Pharmacol. 2021;14(9):1165–71. https://doi.org/10.1080/17512433.2021.1934448.
World Health Organization. ATC/DDD Index 2020. https://www.whocc.no/atc_ddd_index/. Accessed 16 May 2021.
Ministero del Lavoro, della Salute e delle Politiche Sociali. Classificazione delle malattie, dei traumatismi, degli interventi chirurgici e delle procedure dagnostiche e terapeutiche. Versione italiana della ICD9-CM; 2007.
European Medicines Agency. Xadago. EPAR. Product information (last updated 30 Oct 2019). European Medicines Agency; 2019.
European Medicines Agency. Rasagiline. EPAR. Product information (last updated 22 Oct 2020). European Medicines Agency; 2020.
Agenzia Italiana del Farmaco. Selegiline. Summary of product characteristics (last updated 18 Jan 2020). Agenzia Italiana del Farmaco; 2020.
Istituto Nazionale di Statistica, ISTAT. Resident population by age, sex and marital status. Istituto Nazionale di Statistica; 2017. http://demo.istat.it/popres/index.php?anno=2017&lingua=ita. Accessed 16 May 2021.
Agenzia Italiana del Farmaco. Osservatorio Nazionale sull’impiego dei Medicinali. L’uso dei Farmaci in Italia. Rapporto Nazionale Anno 2017. Roma: Agenzia Italiana del Farmaco; 2018 [The Medicines Utilisation Monitoring Centre. National Report on Medicines use in Italy. Year 2017. Rome: Italian Medicines Agency, 2018].
Krishna R, Ali M. Moustafa AA Effects of combined MAO-B inhibitors and levodopa vs monotherapy in Parkinson’s disease. Front Aging Neurosci. 2014;6:180. https://doi.org/10.3389/fnagi.2014.00180.
Klietz M, Greten S, Wegner F, Höglinger GU. Safety and tolerability of pharmacotherapies for Parkinson’s disease in geriatric patients. Drugs Aging. 2019;36(6):511–30. https://doi.org/10.1007/s40266-019-00654-z.
Suzuki M, Arai M, Hayashi A, Ogino M. Adherence to treatment guideline recommendations for Parkinson’s disease in Japan: A longitudinal analysis of a nationwide medical claims database between 2008 and 2016. PLoS ONE. 2020;15(4): e0230213. https://doi.org/10.1371/journal.pone.0230213.
Müller T, Hoffmann JA, Dimpfel W, Oehlwein C. Switch from selegiline to rasagiline is beneficial in patients with Parkinson’s disease. J Neural Transm (Vienna). 2013;120(5):761–5. https://doi.org/10.1007/s00702-012-0927-3.
Mancini F, Di Fonzo A, Lazzeri G, et al. Real life evaluation of safinamide effectiveness in Parkinson’s disease. Neurol Sci. 2018;39(4):733–9. https://doi.org/10.1007/s10072-018-3272-y.
Stocchi F, Vacca L, Grassini P, et al. Overnight switch from rasagiline to safinamide in Parkinson’s disease patients with motor fluctuations: a tolerability and safety study. Eur J Neurol. 2021;28(1):349–54. https://doi.org/10.1111/ene.14552.
Martí-Andrés G, Jiménez-Bolaños R, Arbelo-González JM, et al. Safinamide in clinical practice: a Spanish multicenter cohort study. Brain Sci. 2019;9(10):272. https://doi.org/10.3390/brainsci9100272.
SNLG-LIMPE-ISS. Linea Guida: "Diagnosi e terapia della malattia di Parkinson" [Guideline: "Diagnosis and therapy of Parkinson's Disease]. Updated to January 2015.
Tosin MHS, Stebbins GT, Goetz CG, et al. Measuring medication adherence in Parkinson’s disease: a systematic review of contributing components in rating scales. Mov Disord Clin Pract. 2020;7(6):607–15. https://doi.org/10.1002/mdc3.13006.
Straka I, Minár M, Škorvánek M, et al. Adherence to pharmacotherapy in patients with Parkinson’s disease taking three and more daily doses of medication. Front Neurol. 2019;10:799. https://doi.org/10.3389/fneur.2019.00799.
Lo Monaco MR, Petracca M, Vetrano DL, et al. Safinamide as an adjunct therapy in older patients with Parkinson’s disease: a retrospective study. Aging Clin Exp Res. 2020;32(7):1369–73. https://doi.org/10.1007/s40520-020-01469-4.
Dodel R, Tinelli M, Deuschl G, et al. The economic benefit of timely, adequate, and adherence to Parkinson’s disease treatment: the Value of Treatment Project 2. Eur J Neurol. 2021;28(2):707–16. https://doi.org/10.1111/ene.14584.
de Bie RMA, Clarke CE, Espay AJ, et al. Initiation of pharmacological therapy in Parkinson’s disease: when, why, and how. Lancet Neurol. 2020;19(5):452–61. https://doi.org/10.1016/s1474-4422(20)30036-3.
Müller T. Safinamide: an add-on treatment for managing Parkinson’s disease. Clin Pharmacol. 2018;10:31–41. https://doi.org/10.2147/cpaa.s137740.
Abbruzzese G, Kulisevsky J, Bergmans B, et al. A European observational study to evaluate the safety and the effectiveness of safinamide in routine clinical practice: the SYNAPSES trial. J Parkinsons Dis. 2021;11(1):187–98. https://doi.org/10.3233/jpd-202224.
Qureshi AR, Rana AQ, Malik SH, et al. Comprehensive examination of therapies for pain in Parkinson’s disease: a systematic review and meta-analysis. Neuroepidemiology. 2018;51(3–4):190–206. https://doi.org/10.1159/000492221.
Giossi R, Carrara F, Mazzari M, et al. Overall efficacy and safety of safinamide in Parkinson’s disease: a systematic review and a meta-analysis. Clin Drug Investig. 2021;41(4):321–39. https://doi.org/10.1007/s40261-021-01011-y.
Acknowledgments
The authors would like to thank Cecilia Baroncini for the professional language proofreading of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was partially supported by an unconditional grant from Zambon Italy. Zambon Italy was not involved in data collection, data analysis and interpretation, writing the report, or in deciding to submit the article for publication.
Conflicts of interest/competing interests
Giulia Ronconi, Silvia Calabria, Carlo Piccinni, Letizia Dondi, Antonella Pedrini, Immacolata Esposito, Alice Addesi, Luisa Sambati, and Nello Martini declare no conflicts of interests/competing interests.
Availability of data and material
The datasets generated and/or analyzed during the current study are not publicly available because they come from anonymized administrative databases in property of the Italian Regional and Local Health Facilities, therefore they were analyzed by Fondazione ReS under specific agreement.
Code availability
Oracle SQL Developer Italian version 18.1.0.095 (Los Angeles, CA, USA) software was used to conduct all the analyses.
Authors’ contributions
All authors contributed to the study conception and design. Material preparation and data collection and analysis were performed by Giulia Ronconi, Letizia Dondi, Silvia Calabria, Carlo Piccinni, Antonella Pedrini and Luisa Sambati. The first draft of the manuscript was written by Silvia Calabria, Luisa Sambati and Carlo Piccinni, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethics approval
Ethical approval was not sought for the present study because it was based on the reuse of anonymous administrative data and conducted for institutional purposes, in agreement with the Italian health facilities (regions and local health units).
Consent to participate
Consent to participate was not sought for the present study.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ronconi, G., Calabria, S., Piccinni, C. et al. Prescription Pattern of Monoamine Oxidase B Inhibitors Combined with Levodopa: A Retrospective Observational Analysis of Italian Healthcare Administrative Databases. Drugs - Real World Outcomes 9, 391–401 (2022). https://doi.org/10.1007/s40801-022-00308-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-022-00308-4