Abstract
Background
Guidelines highlight the importance of an individualized approach to treatment initiation for Parkinson’s disease. Our aim was to investigate initiation of anti-Parkinson medication in Australia from 2013–2018, and to determine factors predicting choice of initial treatment.
Methods
Cohort of new-users (N = 4,887) of anti-Parkinson medication aged ≥ 40 years were identified from a 10% random representative sample of national medication dispensing data from July-2013 to June-2018. Changes in treatment initiation were examined across the whole cohort and stratified by age and sex.
Results
Treatment initiation was most frequent with levodopa followed by non-ergot dopamine agonists (DAs) and anticholinergics. Two thirds initiated with levodopa across the study period. Initiation with non-ergot DAs increased from 22 to 27% (rate ratio, RR 1.23, 95% confidence interval, CI 1.02–1.47) and initiation with anticholinergics decreased from 6.9% to 2.4% (RR 0.34, 95% CI 0.21–0.55) from 2013–2018. Among persons aged ≥ 65 years, one third of women and one fourth of men initiated on levodopa. Among women aged < 65 years, rates of treatment initiation with DAs (37%) and levodopa (37%) were similar in 2013/2014 but initiation with DA exceeded levodopa thereafter. Among men aged < 65 years, treatment initiation with levodopa (44%-49%) remained more frequent than initiation with DAs (29%-32%) throughout the study period.
Conclusions
Treatment initiation with levodopa was most frequent among persons aged ≥ 65 years, consistent with current guidelines. Whilst the value of levodopa sparing strategies is unclear, treatment initiation with DA has become increasingly common relative to levodopa among women but not among men aged < 65 years.
Similar content being viewed by others
Background
Uncertainties exist in relation to the optimal initial treatment for Parkinson’s disease (PD). Clinical guidelines recognize that levodopa provides the greatest benefit for motor symptoms [1,2,3,4,5,6]. However, long-term levodopa treatment is associated with motor fluctuations. Clinicians often prefer levodopa-sparing strategies (e.g. non-ergot dopamine agonists (DAs) or monoamine oxidase B (MAO-B) inhibitors) as initial therapy, especially among younger patients at higher risk of motor fluctuations and dyskinesia. Nevertheless, evidence suggests long-term motor complications and motor function are similar with initiation of levodopa or DAs [7,8,9]. DAs have higher risk of neuropsychiatric adverse events than levodopa [9].
Initial medication selection is individualized according to clinical characteristics (e.g. predominant symptoms, symptom severity, disability), comorbidities, concomitant medications, individual life circumstances and treatment preferences [1,2,3,4,5,6]. The United Kingdom NICE guidelines recommend levodopa in the early stage if motor symptoms impact quality of life; and DAs, levodopa or MAO-B inhibitors if motor symptoms do not affect quality of life [4]. Other guidelines recommend non-ergot DAs or MAO-B inhibitors for younger patients or patients with mild symptoms [1,2,3, 5, 10]. Levodopa is often recommended for older patients, those with more severe symptoms, or at higher risk of cognitive and psychiatric adverse events. Connolly and Lang [10] suggest three decision trees according to predominant symptoms i.e. for ‘tremor-dominant motor symptoms’, ‘predominant bradykinesia and impaired dexterity’, and ‘predominant postural instability and gait impairment’. Differences in guideline recommendations are likely to contribute to within and between country differences in treatment initiation for PD.
The objective of this study was to investigate changes in initiation of anti-Parkinson medication in Australia from 2013–2018, and to determine factors that predict choice of first anti-Parkinson medication.
Methods
Study design and setting
This retrospective cohort study utilized Australian Pharmaceutical Benefit Scheme (PBS) data for a random representative 10% sample of the Australian population [11]. The PBS random sample has been made available to research by Services Australia. The 10% random sample is derived from a ‘one in ten’ random sample of patients eligible to the Australia’s universal health care system Medicare, and dispensed medications via the PBS. The PBS subsidizes prescription medications for Australia’s 25 million citizens, permanent residents and foreign visitors from countries with reciprocal health care agreements. The data contain person-level records of all reimbursed medications dispensed from community pharmacies, private hospitals and public hospital outpatient and discharge dispensing in all states except New South Wales and Australian Capital Territory. Since July 2012, all under co-payment are captured. Data include quantity dispensed, PBS item code, dispensing date, sex, birth year, death year, and concessional status. PBS item codes are mapped to the medication name, strength and Anatomical Therapeutic Chemical (ATC) Classification codes [12].
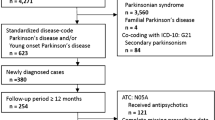
Study sample
We first identified all persons aged ≥ 40 years first dispensed an anti-Parkinson medication (ATC code N04) between 1st July 2013 and 30th June 2018 (shown in Fig. 1). We excluded persons with previous anti-Parkinson medication use to identify incident users. We required initiators to have a second dispensing within 6-month from the first dispensing. We excluded persons with ≥ 1 dispensings of acetylcholinesterase inhibitors (N06DA) or memantine (N06DX01) prior to initiating an anti-Parkinson medication. In addition, we excluded persons with ≥ 1 dispensings of antipsychotics (N05A, excluding lithium), prochlorperazine (N05AB04) or metoclopramide (A03FA01) during the preceding three months. These exclusion criteria were applied because the diagnostic criteria for PD suggest that early dementia or onset of symptoms coinciding with dopamine antagonist treatment suggests diagnosis other than PD [13]. In Australia, two of the 12 available pramipexole products were only subsidized for persons with severe restless legs syndrome and persons initiating these two products were excluded. We also excluded persons who initiated cabergoline or bromocriptine products subsidized for hyperprolactinemia or prevention of the onset of lactation.
Exposure
Persons dispensed a second anti-Parkinson medication within one month of their first anti-Parkinson medication (N04) were considered to have initiated on a combination regimen.
The initial anti-Parkinson medications were categorized into eight mutually exclusive groups:
-
levodopa with peripheral decarboxylase inhibitor (N04BA02);
-
anticholinergics (N04AA01 benzhexol, N04AA02 biperiden, N04AC01 benzatropine);
-
non-ergot DAs (pramipexole N04BC05, apomorphine N04BC07, rotigotine N04BC09);
-
ergot DAs (bromocriptine N04BC01, pergolide N04BC02, cabergoline N04BC06);
-
MAO-B inhibitors (selegiline N04BD01, rasagiline N04BD02);
-
amantadine (N04BB01);
-
levodopa with entacapone (N04BA03 or N04BA02 + N04BX02) or entacapone only (N04BX02); and
-
combination regimens of ≥ 2 different anti-Parkinson drug groups.
Covariates
Concessional status (concessional or general) was defined based on initial anti-Parkinson dispensing. All other covariates were measured at baseline with a 12-month look-back period. Comorbidities were identified using medication dispensings as proxies for medical conditions using the Rx-Risk Index [14]. Comorbidities included cardiovascular disorders, diabetes, gastric acid disorder, reactive airway disease, and osteoporosis/Paget’s. As neuropsychiatric disturbances are a prediagnostic feature of PD [15], we considered antidepressants, benzodiazepines and related drugs, and antipsychotics as predictors. As antipsychotic users during preceding 3 months were excluded, use of antipsychotics was measured from 3 to 12 months prior baseline. Use of propranolol was included as a marker of tremor-dominant symptoms [10]. Use of opioids, nonsteroidal anti-inflammatory agents (NSAIDs), paracetamol and pregabalin were included as markers of pain because different types of pain are common in PD [16] (Supplementary Table 1).
Statistical analyses
Characteristics of the new users were described as frequencies and percentages, or medians and interquartile ranges (IQR). Changes in treatment initiation were studied for the whole study sample and stratified by age group and sex. Poisson regression was used to calculate rate ratios (RRs) with 95% Confidence Intervals (CIs) for the initiation of different anti-Parkinson medications. The July 2013-June 2014 financial year, initiators aged ≥ 65 years, and men were used as reference groups when comparing the incidence rates between years, age groups and sexes, respectively. The associations between predictors and initial anti-Parkinson medication were analyzed with logistic regression and initiation of levodopa was used as the reference category. The odds ratios (ORs) with 95% CIs were adjusted for financial year and all the predictors included into the model. All analyses were conducted using SAS Version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
The study sample comprised 4,887 new users of anti-Parkinson medication (shown in Fig. 1). The median age at initiation was 73 (IQR 63–80) years, 56% were men and 74% were concessional beneficiaries (Table 1). Three quarters were dispensed cardiovascular medications, 59% analgesics, 50% psychotropics, and 45% medications for gastric acid disorders during the preceding year.
Treatment initiation with levodopa was most frequent overall and ranged from 61 to 65% (shown in Supplementary Fig. 1A, Supplementary Table 2). Initiation of non-ergot DAs increased from 22% in 2013/2014 to 27% in 2016/2017 (RR 1.23, 95% CI 1.02–1.47). The majority of initiations with non-ergot DAs comprised of pramipexole initiations (98.7%) and only 1.4% of persons initiated with rotigotine. Initiation with anticholinergics decreased from 6.9% to 2.4% (RR 0.34, 95% CI 0.21–0.55). Initiation with MAO-B inhibitors or combination therapy ranged between 3–4% whereas initiation with amantadine, ergot-derived DAs, or levodopa with catechol-o-methyltransferase inhibitor (LD + COMT), varied below 1% for each group (shown in Supplementary Fig. 1B, Supplementary Table 2).
Levodopa was the most commonly initiated medication among persons aged ≥ 65 years, varying from 70 to 73% (shown in Fig. 2A). Initiation with non-ergot DAs was less frequent among older initiators and was highest (22%) in 2016/2017 compared to 2013/2014 (17%). Among younger persons, initiation with non-ergot DAs (45%) exceeded initiation with levodopa (37%) only in 2015/2016 (shown in Fig. 2A). Otherwise, initiation with levodopa was similar or more frequent than initiation with non-ergot DAs. Persons aged < 65 years compared to those aged ≥ 65 years initiated more frequently with anticholinergics (8.9%-5.7% vs. 6.1%-1.1%) throughout the follow-up. Compared with older people, younger people were also more likely to initiate with MAO-B inhibitors and combination therapy than levodopa (Table 2).
Women were more likely to initiate with non-ergot DAs (RR 1.46, 95% CI 1.31–1.64 adjusted for financial year and age) and amantadine (2.52, 95% CI 1.31–4.85), and less likely to initiate with levodopa (RR 0.88, 95% CI 0.82–0.94) and MAO-B inhibitors (0.62, 95% CI 0.45–0.85) compared to men (shown in Fig. 2B). Among women aged < 65 years, initiation with DAs (37%) was as frequent as initiation with levodopa (37%) in the first financial year but exceeded initiation with levodopa thereafter (shown in Fig. 3A). Among men aged < 65 years, initiation with levodopa (44%-49%) was more frequent than initiation with non-ergot DAs (29%-32%) throughout the follow-up. In both men and women aged ≥ 65 years, initiation with levodopa was most common but still less frequent among women (65%-68%) than among men (73%-76%) (shown in Fig. 3B). In addition to age and sex, concessional status, use of analgesics, antidepressants, antipsychotics and benzodiazepines and related drugs, and specific comorbidities such as cardiovascular disorders, reactive airway diseases, and gastric acid disorder were associated with initiation of different anti-Parkinson medication (Table 2).
Discussion
This is the first national study to report the patterns of treatment initiation for PD in Australia. Overall initiation with levodopa remained stable from 2013 to 2018, whereas initiation with non-ergot DAs increased and anticholinergics decreased. Women were more likely to initiate treatment with non-ergot DAs than men. Non-ergot DAs were preferred over levodopa as initial medication in women aged < 65 years after 2014, whereas levodopa was preferred among men aged < 65 and ≥ 65 years throughout the study period.
Our finding that levodopa was preferred as initial therapy among persons aged ≥ 65 years is consistent with guidelines [1,2,3, 5, 10, 13]. There is no Australian National Health and Medical Research Council guideline for the treatment of PD. However, the widely used Therapeutic Guidelines: Neurology [13] recommend levodopa due to the favourable benefit-to-risk ratio, particularly for persons aged > 70 years or with cognitive impairment. Among persons aged < 65 years, the initial choice varied between levodopa and non-ergot DAs during the five years. Similarly, DAs were preferred as initial medication among persons aged < 60 years in Finland in 2005 and 2012 [17]. Although not directly recommended in the Therapeutic Guidelines [13], initiation with DA in younger persons is consistent with international clinical guidelines [2, 3, 5, 10], with a view to avoiding or delaying levodopa-induced motor complications.
We identified different treatment approaches among men and women despite this not being recommended in guidelines. Levodopa-induced dyskinesias and milder initial symptoms are more likely among women [18, 19], which could explain why DAs were preferred among women. In addition, differences in predominant symptoms, individual life circumstances, preferences, and physician’s attitudes could affect the treatment choice. However, PBS data did not permit analyses of these factors in our study. A recent study from the United States [20] found women had delayed treatment initiation and longer time to treatment switches and add-on than men. Men also use higher levodopa equivalent doses than women but this may reflect dosage adjustment according to patient’s body weight and symptoms [18]. Our findings are similar to an Israeli study [21] that found men aged 75–84 years had higher rate of levodopa initiation than women and younger men aged 50–74 years had higher rates of MAO-B inhibitor use than younger women. Contrary to our findings, older men had higher rates of DA use compared to older women [21]. Further studies are needed to establish the generalizability of our findings to other populations, and to investigate the reasons for and outcomes of preferential initiation with DAs among women.
Treatment initiation with anticholinergics declined in all age groups. This may be because anticholinergics are considered relatively ineffective and associated with anticholinergic adverse events such as confusion, cognitive decline and hallucinations [1, 3, 5] Persons who initiated anticholinergics were more likely to have used propranolol during the preceding year than levodopa initiators, suggesting anticholinergics may have been used for tremor-dominant symptoms. However, apparent initiation with anticholinergics, particularly early in the study period, was unexpected because the Therapeutic Guidelines only recommend anticholinergics as alternatives or adjunct medications after specialist referral if response to levodopa is inadequate [13]. In comparison, treatment was rarely initiated with anticholinergics in Finland in 2012 [17]. Because anticholinergics are mainly used for drug-induced extrapyramidal adverse events [22, 23], we excluded persons who used antipsychotics, prochlorperazine, or metoclopramide in the three months prior to initiation of anti-Parkinson medications. Despite this, initiators of anticholinergics were more likely to have used antipsychotics during the preceding year (13.1%) than initiators of levodopa (1.5%). It is possible, therefore, that our results represent an overestimate of the true rate of treatment initiation with anticholinergics for primary PD because anticholinergic may have been used for the secondary parkinsonism related to antipsychotic use.
Initiation with MAO-B inhibitors was rare throughout the study period. In contrast, initiation with MAO-B inhibitors increased from 18.5% to 33.5% in persons aged < 60 years and from 11.9% to 17.0% in persons aged 60–74 years in Finland from 2005 to 2012 [17]. Several reasons may explain this difference. In Australia, rasagiline was not PBS subsidized for PD for both monotherapy and adjunctive therapy until March 2012 and selegiline is only PBS subsidized for late stage PD as adjunctive therapy [24]. This restriction explains why 91% of MAO-B inhibitor users initiated with rasagiline. The Therapeutic Guidelines state that MAO-B inhibitors have mild effects on symptoms of PD [13]. In comparison, the Finnish Clinical Care Guideline recommends patients aged < 60–65 years and patients with mild symptoms be initiated on either DAs or MAO-B inhibitors [5]. Thus, this difference may reflect the differences in the strength of guideline recommendations and reimbursement practices.
Persons with concessional status were more likely to initiate anticholinergics and less likely to initiate non-ergot DAs and MAO-B inhibitors than levodopa. Anticholinergics were the least expensive anti-Parkinson medications whereas rasagiline was more expensive than most levodopa products. However, the PBS patient co-payment was the same for all medications [25]. Therefore, it is unclear why persons with concessional status were more likely to initiate less expensive medications, unless prescribers were unaware of the cost to the patient. Anecdotally, this might be true for hospital-based prescribers less familiar with Australia’s PBS that predominately reimburses medications dispensed in community and outpatient settings.
Strengths and limitations
A strength of our study is that the 10% random sample is representative for all 25 million Australian residents. We restricted the study period to July 2013 onwards to capture all the under co-payment dispensings. However, the data did not include records of medications not listed on the PBS. General limitations of dispensing data are that it does not include information on diagnoses, type or severity of symptoms. We used anti-Parkinson medication dispensing as a proxy for PD. We cannot be certain that all new users had primary PD rather than other movement disorders. However, we excluded persons who initiated pramipexole products for severe restless legs syndrome, and cabergoline and bromocriptine for hyperprolactinemia. No validation studies have investigated the use of PBS item codes by prescribers. Therefore, it is possible we excluded some persons with primary PD and vice versa. Our results regarding use of anticholinergics and ergot-derived DAs may represent an overestimate.
Conclusions
Levodopa was the most commonly initiated medication among persons aged ≥ 65 years. However, treatment initiation with DA has become increasingly common relative to levodopa among women but not among men aged < 65 years. Differences in the pattern of treatment initiation among men and women deserve further investigation.
Availability of data and materials
The data that support the findings of this study are available from Services Australia. Restrictions apply to the availability of these data, which were used under license for this study.
Abbreviations
- ATC:
-
Anatomical Therapeutic Chemical
- CI:
-
Confidence interval
- DAs:
-
Dopamine agonists
- IQR:
-
Interquartile ranges
- LD + COMT:
-
Levodopa plus catechol-o-methyltransferase inhibitor
- MAO-B:
-
Monoamine oxidase B
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- OR:
-
Odds ratio
- PBS:
-
Pharmaceutical Benefit Scheme
- PD:
-
Parkinson’s disease
- RR:
-
Rate ratio
References
Grimes D, Gordon J, Snelgrove B, Lim-Carter I, Fon E, Martin W, et al. Canadian guidelines on Parkinson’s disease. Can J Neurol Sci. 2012;39:S1–30.
Ferreira JJ, Katzenschlager R, Bloem BR, Bonuccelli U, Burn D, Deuschl G, et al. Summary of the recommendations of the EFNS/MDS-ES review on therapeutic management of Parkinson’s disease. Eur J Neurol. 2013;20:5–15.
Chen S, Chan P, Sun S, Chen H, Zhang B, Le W, et al. The recommendations of Chinese Parkinson’s disease and movement disorder society consensus on therapeutic management of Parkinson’s disease. Transl Neurodegener. 2016;5:12.
NICE (the National Institute for Health and Care Excellence), NICE guideline NG71: Parkinson’s disease in adults: diagnosis and management 2017. https://www.nice.org.uk/guidance/ng71. Accessed 22 Jun 2020.
Working group appointed by the Finnish Medical Society Duodecim and the Finnish Neurological Society. Parkinson’s disease, Current Care Guidelines 2019. Helsinki: The Finnish Medical Society Duodecim [In Finnish]. https://www.kaypahoito.fi/hoi50042. Accessed 22 Jun 2020.
Fox SH, Katzenschlager R, Lim SY, Barton B, de Bie RMA, Seppi K, et al. International Parkinson and Movement Disorder Society Evidence-Based medicine review: Update on treatments for the motor symptoms of Parkinson’s disease. Mov Disord. 2018;33:1248–66.
Hayes MW, Fung VS, Kimber TE, O’Sullivan JD. Updates and advances in the treatment of Parkinson disease. Med J Aust. 2019;211:277–83.
PD Med Collaborative Group, Gray R, Ives N, Rick C, Patel S, Gray A, et al. Long-term effectiveness of dopamine agonists and monoamine oxidase B inhibitors compared with levodopa as initial treatment for Parkinson's disease (PD MED): a large, open-label, pragmatic randomized trial. Lancet. 2014;384:1196–1205.
Zhang J, Tan TC. Revisiting the medical management of Parkinson’s disease: Levodopa versus dopamine agonist. Curr Neuropharmacol. 2016;14:356–63.
Connolly BS, Lang AE. Pharmacological treatment of Parkinson disease: A review. JAMA. 2014;311:1670–83.
Mellish L, Karanges EA, Litchfield MJ, Schaffer AL, Blanch B, Daniels BJ, et al. The Australian Pharmaceutical Benefits Scheme data collection: A practical guide for researchers. BMC Res Notes. 2015;8:634.
WHO Collaborating Centre for Drug Statistics Methodology. The Anatomical Therapeutic Chemical Classification system 2019. https://www.whocc.no/atc_ddd_index/ Accessed 22 Jun 2020.
Neurology Expert Group. Therapeutic Guidelines: Neurology, Version 5, Therapeutic Guidelines Limited. Published November 2017, Amended March 2018, (eTG January 2019 edition).
Pratt NL, Kerr M, Barratt JD, Kemp-Casey A, Kalisch Ellett LM, Ramsay E, et al. The validity of the Rx-Risk Comorbidity Index using medicines mapped to the Anatomical Therapeutic Chemical (ATC) classification system. BMJ Open. 2018;8: e021122.
Schrag A, Horsfall L, Walters K, Noyce A, Petersen I. Prediagnostic presentations of Parkinson’s disease in primary care: A case-control study. Lancet Neurol. 2015;14:57–64.
Ha AD, Jankovic J. Pain in Parkinson’s disease. Mov Disord. 2012;27:485–91.
Keränen T, Virta LJ. Association of guidelines and clinical practice in early Parkinson’s disease. Eur Geriatr Med. 2016;7:131–4.
Picillo M, Nicoletti A, Fetoni V, Garavaglia B, Barone P, Pellecchia MT. The relevance of gender in Parkinson’s disease: A review. J Neurol. 2017;264:1583–607.
Cerri S, Mus L, Blandini F. Parkinson’s disease in women and men: What’s the difference? J Parkinsons Dis. 2019;9:501–15.
Houghton R, Boess F, Verselis L, Ding Y, Freitas R, Constantinovici N, et al. Treatment patterns in patients with incident Parkinson’s disease in the United States. J Parkinsons Dis. 2019;9:749–59.
Peretz C, Chillag-Talmor O, Linn S, Gurevich T, El-Ad B, Silverman B, et al. Parkinson’s disease patients first treated at age 75 years of older: A comparative study. Parkinsonism Relat Disord. 2014;20:69–74.
Gjerden P, Bramness JG, Slordal L. The use and potential abuse of anticholinergic antiparkinson drugs in Norway: A pharmacoepidemiological study. Br J Clin Pharmacol. 2009;67:228–33.
Hollingworth SA, Rush A, Hall WD, Eadie MJ. Utilization of anti-Parkinson drugs in Australia: 1995–2009. Pharmacoepidemiol Drug Saf. 2011;20:450–6.
Pharmaceutical Benefits Advisory Committee (PBAC). Public Summary Document, Rasagiline, tablet, 1 mg (as mesilate), Azilect® 2012. http://www.pbs.gov.au/info/industry/listing/elements/pbac-meetings/psd/2012-03/rasagiline. Accessed 22 Jun 2020.
Australian Government Department of Health. Pharmaceutical Benefits, Fees, patients contributions and safety net thresholds 2020. http://www.pbs.gov.au/info/healthpro/explanatory-notes/front/fee. Accessed 22 Jun 2020.
Acknowledgements
The authors would like to acknowledge Services Australia for data provision.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MK, JSB, SL, RW, AMK, and JI conceptualized and designed the study, JI acquired the data, MK analyzed the data, and MK, JSB, SL, RW, AMK, and JI interpreted the data. MK, JSB, SL, RW, AMK, and JI drafted and revised the article for important intellectual content, and approved the final version of the submitted manuscript.
Corresponding author
Ethics declarations
Ethics and analysis approval and consent to participate
This research was conducted in accordance with the Declaration of Helsinki and the Australian Code for the Responsible Conduct of Research. The authors analysed non-identifiable data provided by Services Australia. No participants were contacted and informed consent was not required. The study was approved by the Monash University Human Research Ethics Committee (approval number 22877). The analysis plan was approved and the manuscript noted by the External Request Evaluation Committee chaired by Services Australia.
Consent for publication
Not applicable
Competing interests
JSB and JI have received funding from Dementia Australia and Yulgilbar Foundation. JSB is funded by a National Health and Medical Research Council Boosting Dementia Leadership Fellowship and has received grant funding from National Health and Medical Research Council (NHMRC), Victorian Government Department of Health and Human Services (DHHS) and Dementia Australia Research Foundation (DARF), GlaxoSmithKline and several aged care provider organizations unrelated to this work. RW is supported by the Yulgilbar Alzheimer’s Research Program. AMK has received grant funding from HS Pitkänen Foundation and Päivikki and Sakari Sohlberg Foundation unrelated to this work. AMK has also received payments for lectures given to medical professionals from TEVA, Allergan, Nutricia, and Finnish Medical Society Duodecim and travel grants for medical congresses from the Finnish Neurological Association, TEVA, Roche, Allergan, and Biogen. JI has received grant funding from the NHMRC, Victorian Government DHHS, National Breast Cancer Foundation and DARF and consultancies from AstraZeneca unrelated to this work. SL and MK have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Figure 1 Proportion of new users who initiated with (A) levodopa, non-ergot dopamine agonists, or anticholinergics; or with (B) other anti-Parkinson drugs for each financial year. (DA=dopamine agonist; MAOBI=Monoamine oxidase B inhibitors; LD+COMT=levodopa + catechol-o-methyltransferase inhibitor)
Additional file 2:
Supplementary Table 1 Definitions of baseline covariates
Additional file 3:
Supplementary Table 2 Proportions and rate ratios of the initiation of different anti-Parkinson medication for each financial year
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Koponen, M., Bell, J.S., Lalic, S. et al. Treatment initiation for parkinson’s disease in Australia 2013–2018: a nation-wide study. BMC Geriatr 22, 483 (2022). https://doi.org/10.1186/s12877-022-03095-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03095-3