Abstract
Objective
The objective of this study was to compare persistence, costs, and healthcare resource utilization in patients with schizophrenia and cardiometabolic comorbidities treated with once-monthly paliperidone palmitate or an oral atypical antipsychotic.
Methods
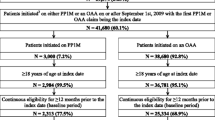
Medicaid data from six states (07/2009–03/2015) were used to identify adults with schizophrenia and cardiometabolic comorbidities initiated on once-monthly paliperidone palmitate or an oral atypical antipsychotic (index date) on 01/2010 or after. Persistence to index medication at 12 months (no gap ≥ 90 days) was compared between patients taking once-monthly paliperidone palmitate and an oral atypical antipsychotic using Chi-squared tests. The 12-month post-index healthcare costs and healthcare resource utilization were compared using multivariate ordinary least squares and Poisson regression, respectively.
Results
Selected patients taking once-monthly paliperidone palmitate (n = 371) were younger (mean age: 45.0 vs. 47.5 years, standardized difference = 24%) than patients taking oral atypical antipsychotics (n = 8296). Persistence at 12 months was higher in patients taking once-monthly paliperidone palmitate (40 vs. 33%, p = 0.006). Adjusted all-cause medical costs were lower in patients taking once-monthly paliperidone palmitate vs. patients taking oral atypical antipsychotics (mean monthly cost differences = US $ − 369, p = 0.004) while all-cause pharmacy costs were higher (mean monthly cost differences = US $279, p < 0.001), resulting in no significant difference in total costs (mean monthly cost differences = US $ − 90, p = 0.357). No significant difference was observed in cardiometabolic comorbidity-related pharmacy or medical costs. Compared with patients taking oral atypical antipsychotics, patients taking once-monthly paliperidone palmitate had more schizophrenia-related outpatient visits (incidence rate ratio = 1.44, p < 0.001) but fewer cardiometabolic comorbidity-related inpatient admissions (incidence rate ratio = 0.73, p < 0.001) with shorter lengths of stay (incidence rate ratio = 0.72, p = 0.020), and fewer cardiometabolic comorbidity-related long-term care admissions (incidence rate ratio = 0.56, p = 0.016).
Conclusions
Medicaid beneficiaries with schizophrenia and cardiometabolic comorbidities who were initiated on once-monthly paliperidone palmitate had similar 12-month total healthcare costs compared with oral atypical antipsychotics. Cardiometabolic comorbidity-related utilization of inpatient and long-term care services was lower in patients taking once-monthly paliperidone palmitate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Persistence at 12 months was higher in patients taking once-monthly paliperidone palmitate (PP1M) than in patients taking an oral atypical antipsychotic. |
Adjusted all-cause medical costs were significantly lower in patients taking PP1M vs. patients taking oral atypical antipsychotics while all-cause pharmacy costs were significantly higher, resulting in no significant difference in total costs. |
Compared with patients taking oral atypical antipsychotics, patients taking PP1M had more schizophrenia-related outpatient visits and similar all-cause and schizophrenia-related inpatient visits; however, patients taking PP1M had fewer cardiometabolic comorbidity-related inpatient admissions with shorter length of stays, and fewer cardiometabolic comorbidity-related long-term care admissions. |
1 Introduction
The annual prevalence of schizophrenia in adults is estimated at between 0.25 and 0.51% in USA [1], with affected individuals having an estimated life expectancy 15–30 years shorter than the general population [2, 3]. This excess mortality is driven by multiple factors, such as the high rates of cardiometabolic comorbidities (CMCs), including diabetes mellitus and cardiovascular disease (CVD) [4, 5].
The presence of CMCs is observed early in individuals diagnosed with schizophrenia. In a population of patients with a first episode of schizophrenia, the prevalence of obesity, dyslipidemia, metabolic syndrome, and hypertension was 48.0, 56.5, 13.2, and 10.0%, respectively [6]. The association between schizophrenia and metabolic syndrome and/or CVD is based on a complex relationship that accounts for genetic, environmental (lifestyle, diet, substance use), and disease-specific factors (treatments and symptoms) [7]. A meta-analysis found schizophrenia was significantly associated with an increased incidence of CVD, stroke, and congestive heart failure, with pooled relative risks ranging from 1.53 to 1.81 [8]. In a study reporting that the prevalence of metabolic syndrome in adults with schizophrenia was 32.5%, the strongest factor influencing the prevalence of metabolic syndrome was the duration of schizophrenia [9].
Schizophrenia is a complex illness that is not only challenging to treat but is also one of the most costly mental illnesses; in 2013, schizophrenia-related direct healthcare costs in USA exceeded US $37.7 billion [10]. Patients with schizophrenia and CMCs may be an important driver of these high costs, as studies have frequently reported increased outpatient or total costs for psychiatric patients with CMCs [11,12,13]. These patients are also more likely to have 30-day readmissions and incur additional costs with each additional CMC [14].
Antipsychotics (APs) are the primary pharmacologic treatment for patients with schizophrenia [15]. Once-monthly paliperidone palmitate (PP1M) is an atypical long-acting injectable AP for patients with schizophrenia that may reduce hospitalizations and lower medical costs compared with oral atypical antipsychotics (OAAs) [16,17,18]. Adherence to APs is critical for patients with schizophrenia to prevent relapse and rehospitalization [19,20,21]. It has been reported that patients with schizophrenia who were adherent to APs were more likely to be adherent to antihypertensive, antihyperlipidemic, and antidiabetic therapies [22]. However, the relationship between APs and CMCs is complex, with studies finding that APs can have a negative impact on some modifiable metabolic disease risk factors such as weight gain [23, 24].
Although prior studies have demonstrated that PP1M is associated with improved adherence and reduced medical costs compared with OAAs [18, 25,26,27,28], there are few real-world studies comparing PP1M with OAAs among patients with CMCs. The current study aims to compare persistence, as well as all-cause, CMC-related, and schizophrenia-related healthcare costs and healthcare resource utilization (HRU) in patients with schizophrenia with CMCs treated with PP1M or an OAA.
2 Methods
2.1 Data Source
The study was conducted using de-identified medical and prescription drug claims from Medicaid databases. The databases included claims of Medicaid beneficiaries from six US states (Iowa, Kansas, Mississippi, Missouri, New Jersey, Wisconsin) from July 2009 to March 2015. Detailed information on patient characteristics, physician visits, hospitalizations, long-term care services, prescription drugs, and other services reimbursed by Medicaid was available. Information was also available for Medicaid payments, out-of-pocket costs, and Medicare copayment and deductibles. Available cost data reflected the Medicaid payers’ perspective, while prescription drug claims were prior to any discounts or rebates. All data were de-identified and in compliance with the Health Insurance Portability and Accountability Act.
2.2 Study Design and Patient Selection
A retrospective cohort study design was used to compare patients with schizophrenia and CMCs, defined as patients with diabetes and/or CVD (including hyperlipidemia, hypertension, and other CVD-related conditions; see Table A of the Electronic Supplementary Material for a full list of the codes), who were initiated on either PP1M or an OAA. Outcomes were evaluated during the fixed 12-month observation period including and following the index date (date of AP initiation), while baseline demographics and clinical characteristics were evaluated during the 6-month period prior to the index date.
To be included in the study, patients were required to meet the following criteria: (1) at least two pharmacy and/or medical claims for PP1M or the same OAA (i.e., two claims for one of the following agents: aripiprazole, asenapine, iloperidone, lurasidone, olanzapine, paliperidone, quetiapine, risperidone, or ziprasidone) within 90 days in the year 2010 or after (the first of the two claims was defined as the index date), (2) no claim for the index agent (PP1M or OAA) in the 6-month period before the index date (baseline period), (3) at least two claims with a diagnosis for schizophrenia during the study period, with at least one claim occurring during the baseline period, (4) at least two claims with a diagnoses for diabetes or at least two claims with a diagnosis of CVD during the study period, with at least one of the claims occurring during the baseline period, (5) at least 6 months of continuous enrollment before the index date, and at least 12 months of follow-up after the index date (observation period), (6) 18–64 years of age as of the index date, and (7) no claim for long-acting injectable therapies during the baseline period (i.e., haloperidol, fluphenazine, aripiprazole, olanzapine, paliperidone, or risperidone long-acting injectable). Treatment groups were defined by the treatment initiated on the index date (i.e., PP1M or specific OAA) and data were analyzed using an intent-to-treat approach.
2.3 Study Outcomes
Outcome measures included persistence, healthcare costs, and HRU measured over the 12-month observation period for each patient and compared between PP1M and OAA treatment groups. Persistence to the index AP at 12 months was defined as not having any gap greater than 30, 60, or 90 days between days with available medication during the 12 months following treatment initiation.
All-cause, schizophrenia-related, and CMC-related costs and HRU measures were reported. Total healthcare costs were calculated and grouped into pharmacy and medical costs. Both medical costs and HRU were stratified into the following categories: outpatient visits, emergency room visits, inpatient visits, skilled nursing and long-term care admissions, mental health institute admissions, 1-day mental health institute outpatient visits, home care services, and other services. Schizophrenia and CMC-related medical costs and HRU were identified as the subset of claims with International Classification of Diseases, 9th revision, Clinical Modification diagnostic codes for schizophrenia, or for diabetes or CVD among patients with each respective comorbidity. Schizophrenia-related pharmacy costs were defined as the costs for AP pharmacy medication claims, while CMC-related pharmacy costs were defined as the costs for diabetes-related and CVD-related medication claims, among patients with each respective comorbidity.
2.4 Statistical Analysis
Descriptive statistics for baseline characteristics included means, medians, standard deviations for continuous variables, and frequencies and proportions for categorical variables. Statistical comparisons between cohorts used standardized differences (Stdiffs), where a Stdiff ≥ 10% was considered clinically meaningful [29, 30]. Persistence to the index medication (i.e., PP1M or index OAA) at 12 months post-index date was compared using Chi-squared tests.
Multivariate adjustment (using age, sex, race, state, region, year of index date, presence of dual insurance eligibility, Quan–Charlson Comorbidity Index, comorbidities (CVD, diabetes), baseline use of atypical APs, presence of AP polypharmacy, total pharmacy costs, total medical costs, the number of mental health institute visits, the number of 1-day mental health institute visits, and the number of comorbidity-related inpatient visits) was conducted for cost and HRU outcome measures. Adjusted medical and pharmacy costs were compared using multivariate ordinary least-squares regressions and mean monthly cost differences (MMCDs), while adjusted HRU outcomes were compared using multivariate Poisson regressions and incidence rate ratios (IRRs). Confidence intervals and p values for both cost and HRU outcomes were obtained from a non-parametric bootstrap procedure (n = 499 replications). All cost outcomes were inflated to 2015 US dollars using the medical care component of the US Consumer Price Index.
3 Results
3.1 Demographic and Clinical Characteristics
A total of 8667 patients with schizophrenia and CMCs met all inclusion criteria, consisting of 371 patients receiving PP1M and 8296 patients receiving OAAs. Among patients receiving OAAs, the most common index agent was risperidone (22.3%), followed by quetiapine (22.0%), aripiprazole (16.5%), olanzapine (14.6%), ziprasidone (9.3%), paliperidone (6.5%), lurasidone (3.7%), asenapine (3.1%), and iloperidone (2.1%). Patients taking PP1M were significantly younger (mean age: 45.0 vs. 47.5 years, Stdiff = 24%), had a lower Quan–Charlson comorbidity index (mean: 1.0 vs. 1.4, Stdiff = 27%), and had lower all-cause baseline healthcare costs (mean: US $2617 vs. US $3160, Stdiff = 11.4%) than patients taking OAA. The percentage of patients with diabetes and CVD medication use was similar across patients taking PP1M (diabetes: 39.9%; CVD: 88.7%) and patients taking OAAs [diabetes: 41.7% (Stdiff = 3.6%); CVD: 88.9% (Stdiff = 0.7%); Table 1].
3.2 Persistence
Figure 1 describes the treatment patterns observed across the PP1M and OAA cohorts during the 12-month observation period. A higher proportion of patients taking PP1M were persistent to the index treatment at 12 month post-index date compared with patients taking OAAs when definitions of no gap ≥ 60 days (34 vs. 27%, p = 0.001) or no gap ≥ 90 days (40 vs. 33%, p = 0.006) were used (Fig. 1). However, there was no significant difference in persistence to the index treatment at 12 months post-index date in patients taking PP1M and OAAs when no gap ≥ 30 days (21 vs. 18%, p = 0.154) was used (Fig. 1).
Index antipsychotic (AP) treatment persistence in patients with schizophrenia with cardiometabolic comorbidities, evaluated during the 12-month follow-up. OAA oral atypical antipsychotic, PP1M once-monthly paliperidone palmitate. * indicates the p value was < 0.05 (vs. OAA). a Persistence was defined as not having any gap greater than 30, 60, or 90 days between AP refills during the 12 months following treatment initiation
3.3 Healthcare Costs
Adjusted all-cause medical costs were significantly lower in patients taking PP1M vs. patients taking OAAs [MMCD = US $ − 369 (95% confidence interval (CI) − 545, − 174), p = 0.004], and all-cause pharmacy costs were significantly higher [MMCD = US $279 (95% CI 213, 347), p < 0.001], resulting in no significant difference in total costs [MMCD = US $ − 90 (95% CI − 272, 114), p = 0.357; Fig. 2]. All-cause medical cost-savings for patients taking PP1M vs. patients taking OAAs were driven by lower costs for inpatient visits [MMCD = US $ − 167 (95% CI − 286, − 12), p = 0.028), skilled nursing and long-term care admissions [MMCD = US $ − 86 (95% CI − 140, − 19), p = 0.008], and home care visits [MMCD = US $ − 145 (95% CI − 221, − 54), p < 0.001; Table 2].
Adjusted mean monthly cost differences in patients with schizophrenia with cardiometabolic comorbidities (CMCs) during the 12-month follow-up. CI confidence interval, MMCD mean monthly cost difference, PP1M once-monthly paliperidone palmitate. a Outcomes were assessed using multivariable linear regression models adjusted for: age, sex, race, state, region, year of index date, presence of dual insurance eligibility, Charlson Comorbidity Index, comorbidities (cardiovascular disease, diabetes), baseline use of atypical antipsychotics, presence of antipsychotic polypharmacy, total pharmacy costs, total medical costs, the number of mental health institute visits, the number of 1-day mental health institute visits, and the number of comorbidity-related inpatient visits. b Ninety-five percent CI and p-values were generated using a non-parametric bootstrap procedure (n = 499 samples). c Schizophrenia- and CMC-related medical costs were identified using International Classification of Diseases, 9th revision diagnosis codes that corresponded with the selected comorbidities. Schizophrenia- and CMC-related pharmacy costs correspond to costs related to pharmacy claims for antipsychotics (schizophrenia related) or cardiovascular disease and diabetes medications (CMC related; among patients with each respective comorbidity). * indicates the p value was < 0.05 (vs. oral atypical antipsychotics)
Adjusted schizophrenia- and CMC-related medical costs were similar between the PP1M and OAA cohorts (Fig. 2). Of note, schizophrenia-related skilled nursing and long-term care costs were lower for patients taking PP1M compared with patients taking OAAs [MMCD = US $ − 36 (95% CI − 65, − 3); p = 0.032], while schizophrenia-related outpatient and 1-day mental health costs were higher for patients taking PP1M [e.g., outpatient: MMCD = US $20 (95% CI 3, 37); p = 0.016; Table 2].
3.4 Healthcare Resource Utilization
Figure 3 illustrates the adjusted HRU comparison between the PP1M and OAA cohorts during the 12-month follow-up period. Once-monthly paliperidone palmitate had significantly lower rates of all-cause skilled nursing and long-term care admissions [IRR = 0.57 (95% CI 0.35, 0.85); p = 0.004] and home care services [IRR = 0.71 (95% CI 0.51, 0.95); p = 0.032], while 1-day mental health institute visit rates were higher [IRR = 1.19 (95% CI 1.07, 1.30); p < 0.001; Fig. 3] compared with patients taking OAAs. Compared with patients taking OAAs, patients taking PP1M had more schizophrenia-related outpatient visits [IRR = 1.44 (95% CI 1.23, 1.67); p < 0.001] and similar rates of all-cause [IRR = 0.89 (95% CI 0.72, 1.08); p = 0.156] and schizophrenia-related [IRR = 1.07 (95% CI 0.83, 1.34); p = 0.658] inpatient visits (Fig. 3). For CMC-related HRU, PP1M patients had fewer CMC-related inpatient admissions [IRR = 0.73 (95% CI 0.58, 0.89); p < 0.001] with shorter cumulative length of stays [IRR = 0.72 (95% CI 0.52, 0.96); p = 0.020], and fewer CMC-related skilled nursing and long-term care admissions [IRR = 0.56 (95% CI 0.29, 0.92); p = 0.016] vs. patients taking OAAs (Fig. 3).
Adjusted healthcare resource utilization in patients with schizophrenia with cardiometabolic comorbidities (CMCs) during the 12-month follow-up. CI confidence interval, IRR incidence rate ratio, PP1M once-monthly paliperidone palmitate. a Outcomes were assessed using multivariable Poisson regression models adjusted for: age, sex, race, state, region, year of index date, presence of dual insurance eligibility, Charlson Comorbidity Index, comorbidities (cardiovascular disease, diabetes), baseline use of atypical antipsychotics, presence of antipsychotic polypharmacy, total pharmacy costs, total medical costs, the number of mental health institute visits, the number of 1-day mental health institute visits, and the number of comorbidity-related inpatient visits. b Ninety-five percent CI and p values were generated using a non-parametric bootstrap procedure (n = 499 samples). * indicates the p value was < 0.05
4 Discussion
This retrospective study assessed the baseline characteristics, treatment patterns, costs, and HRU of patients with schizophrenia and CMCs initiated on PP1M or OAAs. After following the patients over 1 year, we observed that a higher proportion of the PP1M cohort was persistent to their index treatment compared with the OAA cohort. Furthermore, there was no significant difference in total healthcare costs between both cohorts.
This study followed patients with schizophrenia and CMCs, where CMC was defined as having diabetes or CVD. While the definition for a CMC varies in the literature, this study defined a CMC based on a previous publication by Hansen et al., who defined a CMC as having a diagnosis of hypertension, hyperlipidemia, or diabetes [22]. This study slightly expanded on the Hansen et al. definition to include additional CVD conditions, to encompass both patients with risk factors of CVD and patients with specific cardiovascular conditions (e.g., coronary artery disease, congestive heart failure, cardiac arrest). Obesity was excluded from this definition owing to the difficulty in accurately identifying obesity through claims records, as diagnostic codes for obesity are often underreported. Nevertheless, it should be noted that given the conditions that were included in the CMC definition, a high proportion of the study population would be expected to have obesity.
In patients with schizophrenia and CMCs, the 12-month total all-cause cost (pharmacy and medical) was similar between patients initiated on PP1M and OAAs. This was despite the higher pharmacy costs for patients taking PP1M, which were offset by the significant all-cause medical cost savings. Given that these pharmacy costs do not reflect rebates on branded pharmaceutical products in Medicaid or additional manufacturer discounts, pharmacy costs (and therefore total costs) may be overestimated, particularly for patients initiated on PP1M [31].
In the PP1M cohort, all-cause medical cost savings were significantly lower, specifically for services provided in inpatient/long-term care settings as well as in the home (i.e., home care visits), while costs were significantly higher for appropriate short-term schizophrenia-related services (1-day mental health institute outpatient visits). Similar trends were observed in the HRU results; with the exception that similar rates of all-cause but lower rates of CMC-related inpatient visits were found in patients taking PP1M, relative to OAAs. These results seem to indicate that long-term or unplanned inpatient visits occurred less in the PP1M population compared with the OAA population, while planned outpatient visits occurred more in the PP1M population. The cost profile further highlights that PP1M use may lead to a higher utilization of outpatient services and fewer costly inpatient services. This opportunity for a shift in costs to more appropriate and less expensive ambulatory settings may be an important driver in reducing the high economic and humanistic burden of patients with schizophrenia [10]. This is particularly relevant in a population with CMCs, as it has been reported that total healthcare costs increase by 8.3% (25.9% pharmacy and 6.8% medical) for each additional CMC [14]. We observed no difference in terms of CMC-related costs, which suggests that the use of PP1M vs. OAAs did not affect the administration of CMC-related health services. However, this may be related to the poor quality of care and access to medical services among patients with serious mental illness [32,33,34], which is unrelated to medication adherence and instead reflective of the isolation of behavioral health services from other forms of healthcare delivery.
This study has several limitations. The CMC population consists of a mix of patients with several conditions and represents a heterogeneous group, indicating that these results may not be consistent with other populations who may have a different distribution of these disorders. In addition, persistence to OAAs might be overestimated. In fact, as opposed to PP1M, which is administered in a clinical setting, patient claims for OAAs do not mean the medication was subsequently taken. Precise reasons for treatment discontinuation or switching are also not available in claims data, but warrant future investigation in this population to better understand the treatment patterns observed. Additionally, the Medicaid data came from six states, and the patient population may not be representative of other Medicaid states or the general US population. The claims databases used may contain inaccuracies or omissions in diagnoses and other variables, although this is not expected to be differential between cohorts. Moreover, there may be specific initiatives within some states to increase the integration of behavioral health and physical health services, and the effects of such initiatives may not be identifiable through claims and could bias the study results towards the null. Furthermore, as with all retrospective administrative claims data, the study results may be subject to residual confounding because of unmeasured confounders. Nevertheless, with appropriate use of methods to control confounding, health insurance claims data remain a valuable source of information because they contain a large sample of patients’ characteristics and outcomes in a real-world setting.
5 Conclusions
Among Medicaid beneficiaries with schizophrenia and CMCs, those who initiated PP1M were more likely to be persistent to their index AP medication after 12 months when compared with patients initiated on an OAA. Patients taking PP1M also had lower all-cause medical costs, which fully offset the higher pharmacy costs compared with OAAs, resulting in no significant difference in total healthcare costs over 12 months. These cost differences can be attributable to the lower rates of CMC-related inpatient visits and long-term care services in patients initiated on PP1M compared with patients initiated on OAAs. This study suggests a real-world economic benefit of PP1M among the highly prevalent subpopulation of patients with schizophrenia who have coexisting CMCs. Future studies are warranted to build on the limited literature describing the relationship between PP1M and OAAs in patients with schizophrenia and CMCs.
References
Simeone JC, Ward AJ, Rotella P, Collins J, Windisch R. An evaluation of variation in published estimates of schizophrenia prevalence from 1990–2013: a systematic literature review. BMC Psychiatry. 2015;15(1):193.
Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3(2):A42.
Bushe CJ, Taylor M, Haukka J. Mortality in schizophrenia: a measurable clinical endpoint. J Psychopharmacol. 2010;24(4 Suppl.):17–25. https://doi.org/10.1177/1359786810382468.
Lambert TJ, Velakoulis D, Pantelis C. Medical comorbidity in schizophrenia. Med J Aust. 2003;178(Suppl):S67–70.
Bressington D, Mui J, Tse ML, Gray R, Cheung EF, Chien WT. Cardiometabolic health, prescribed antipsychotics and health-related quality of life in people with schizophrenia-spectrum disorders: a cross-sectional study. BMC Psychiatry. 2016;16(1):411. https://doi.org/10.1186/s12888-016-1121-1.
Correll CU, Robinson DG, Schooler NR, Brunette MF, Mueser KT, Rosenheck RA, et al. Cardiometabolic risk in patients with first-episode schizophrenia spectrum disorders: baseline results from the RAISE-ETP study. JAMA Psychiatry. 2014;71(12):1350–63. https://doi.org/10.1001/jamapsychiatry.2014.1314.
De Hert M, Vancampfort D, Correll CU, Mercken V, Peuskens J, Sweers K, et al. Guidelines for screening and monitoring of cardiometabolic risk in schizophrenia: systematic evaluation. Br J Psychiatry. 2011;199(2):99–105. https://doi.org/10.1192/bjp.bp.110.084665.
Fan Z, Wu Y, Shen J, Ji T, Zhan R. Schizophrenia and the risk of cardiovascular diseases: a meta-analysis of thirteen cohort studies. J Psychiatr Res. 2013;47(11):1549–56. https://doi.org/10.1016/j.jpsychires.2013.07.011.
Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, De Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders: a systematic review and meta-analysis. Schizophr Bull. 2013;39(2):306–18. https://doi.org/10.1093/schbul/sbr148.
Cloutier M, Aigbogun MS, Guerin A, Nitulescu R, Ramanakumar AV, Kamat SA, et al. The economic burden of schizophrenia in the United States in 2013. J Clin Psychiatry. 2016;77(6):764–71. https://doi.org/10.4088/JCP.15m10278.
Chwastiak LA, Rosenheck RA, McEvoy JP, Stroup TS, Swartz MS, Davis SM, et al. The impact of obesity on health care costs among persons with schizophrenia. Gen Hosp Psychiatry. 2009;31(1):1–7. https://doi.org/10.1016/j.genhosppsych.2008.09.012.
Guo JJ, Keck PE, Li H, Patel NC. Treatment costs related to bipolar disorder and comorbid conditions among medicaid patients with bipolar disorder. Psychiatr Serv. 2007;58(8):1073–8. https://doi.org/10.1176/ps.2007.58.8.1073.
Jerrell JM, McIntyre RS, Tripathi A. Incidence and costs of cardiometabolic conditions in patients with schizophrenia treated with antipsychotic medications. Clin Schizophr Relat Psychoses. 2010;4(3):161–8. https://doi.org/10.3371/CSRP.4.3.2.
Correll CU, Ng-Mak DS, Stafkey-Mailey D, Farrelly E, Rajagopalan K, Loebel A. Cardiometabolic comorbidities, readmission, and costs in schizophrenia and bipolar disorder: a real-world analysis. Ann Gen Psychiatry. 2017;16:9. https://doi.org/10.1186/s12991-017-0133-7.
Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–23. https://doi.org/10.1056/NEJMoa051688.
Pesa JA, Muser E, Montejano LB, Smith DM, Meyers OI. Costs and resource utilization among Medicaid patients with schizophrenia treated with paliperidone palmitate or oral atypical antipsychotics. Drugs Real World Outcomes. 2015;2(4):377–85. https://doi.org/10.1007/s40801-015-0043-4.
Druais S, Doutriaux A, Cognet M, Godet A, Lancon C, Levy P, et al. Cost effectiveness of paliperidone long-acting injectable versus other antipsychotics for the maintenance treatment of schizophrenia in France. Pharmacoeconomics. 2016;34(4):363–91. https://doi.org/10.1007/s40273-015-0348-x.
Baser O, Xie L, Pesa J, Durkin M. Healthcare utilization and costs of Veterans Health Administration patients with schizophrenia treated with paliperidone palmitate long-acting injection or oral atypical antipsychotics. J Med Econ. 2015;18(5):357–65. https://doi.org/10.3111/13696998.2014.1001514.
Jiang Y, Ni W. Estimating the impact of adherence to and persistence with atypical antipsychotic therapy on health care costs and risk of hospitalization. Pharmacotherapy. 2015;35(9):813–22.
Lally J, MacCabe JH. Antipsychotic medication in schizophrenia: a review. Br Med Bull. 2015;114(1):169–79. https://doi.org/10.1093/bmb/ldv017.
Masand PS, Roca M, Turner MS, Kane JM. Partial adherence to antipsychotic medication impacts the course of illness in patients with schizophrenia: a review. Prim Care Companion J Clin Psychiatry. 2009;11(4):147–54. https://doi.org/10.4088/PCC.08r00612.
Hansen RA, Maciejewski M, Yu-Isenberg K, Farley JF. Adherence to antipsychotics and cardiometabolic medication: association with health care utilization and costs. Psychiatr Serv. 2012;63(9):920–8. https://doi.org/10.1176/appi.ps.201100328.
De Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52–77.
De Hert M, Dekker JM, Wood D, Kahl KG, Holt RI, Moller HJ. Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC). Eur Psychiatry. 2009;24(6):412–24. https://doi.org/10.1016/j.eurpsy.2009.01.005.
Lafeuille MH, Dean J, Carter V, Duh MS, Fastenau J, Dirani R, et al. Systematic review of long-acting injectables versus oral atypical antipsychotics on hospitalization in schizophrenia. Curr Med Res Opin. 2014;30(8):1643–55. https://doi.org/10.1185/03007995.2014.915211.
Xiao Y, Muser E, Lafeuille MH, Pesa J, Fastenau J, Duh MS, et al. Impact of paliperidone palmitate versus oral atypical antipsychotics on healthcare outcomes in schizophrenia patients. J Comp Eff Res. 2015;4(6):579–92. https://doi.org/10.2217/CER.15.34.
Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754–68. https://doi.org/10.18553/jmcp.2015.21.9.754.
Xiao Y, Muser E, Fu DJ, Lafeuille MH, Pilon D, Emond B, et al. Comparison of Medicaid spending in schizoaffective patients treated with once monthly paliperidone palmitate or oral atypical antipsychotics. Curr Med Res Opin. 2016;32(4):759–69. https://doi.org/10.1185/03007995.2016.1140634.
Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simulat Comput. 2009;38(6):1228–34. https://doi.org/10.1080/03610910902859574.
Cohen J. Statistical power analysis for the behavorial sciences. 2nd ed. New York (NY): Routledge; 2013.
Centers for Medicare and Medicaid Services. Medicaid drug rebate program. http://www.medicaid.gov/medicaid/prescription-drugs/medicaid-drug-rebate-program/index.html. Accessed 4 Jan 2017.
Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry. 2009;194(6):491–9. https://doi.org/10.1192/bjp.bp.107.045732.
Nasrallah HA, Meyer JM, Goff DC, McEvoy JP, Davis SM, Stroup TS, et al. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophr Res. 2006;86(1–3):15–22. https://doi.org/10.1016/j.schres.2006.06.026.
Roberts L, Roalfe A, Wilson S, Lester H. Physical health care of patients with schizophrenia in primary care: a comparative study. Fam Pract. 2007;24(1):34–40. https://doi.org/10.1093/fampra/cml054.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the current study. Analyses were carried out by M-HL, ST, RK, and PL. All authors were involved in interpreting the findings and drafting the manuscript, and all approve the final version.
Corresponding author
Ethics declarations
Funding
This study was funded by Janssen Scientific Affairs, LLC.
Conflict of interest
Marie-Hélène Lafeuille, Sean Tiggelaar, Rhiannon Kamstra, and Patrick Lefebvre are employees of Analysis Group, Inc., a consulting company that has received research grants from Janssen Scientific Affairs, LLC, to conduct this study. Kruti Joshi, Neeta Tandon, Yong Yue, and Edward Kim are employees of Janssen Scientific Affairs, LLC.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Lafeuille, MH., Tandon, N., Tiggelaar, S. et al. Economic Impact in Medicaid Beneficiaries with Schizophrenia and Cardiometabolic Comorbidities Treated with Once-Monthly Paliperidone Palmitate vs. Oral Atypical Antipsychotics. Drugs - Real World Outcomes 5, 81–90 (2018). https://doi.org/10.1007/s40801-018-0130-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-018-0130-4