Abstract
Introduction
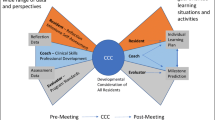
The Core Entrustable Professional Activities for Entering Residency (Core EPAs) are clinical activities all interns should be able to perform on the first day of residency with indirect supervision. The acting (sub) internship (AI) rotation provides medical students the opportunity to be assessed on advanced Core EPAs.
Materials and Methods
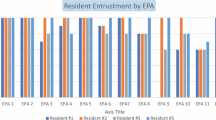
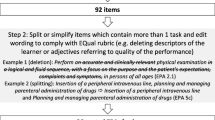
All fourth-year AI students were taught Core EPA skills and performed these clinical skills under direct supervision. Formative feedback and direct observation data were provided via required workplace-based assessments (WBAs). Supervising physicians rated learner performance using the Ottawa Clinic Assessment Tool (OCAT). WBA and pre-post student self-assessment data were analyzed to assess student performance and gauge curriculum efficacy.
Results
In the 2017–2018 academic year, 167 students completed two AI rotations at our institution. By their last WBA, 91.2% of students achieved a target OCAT supervisory scale rating for both patient handoffs and calling consults. Paired sample t tests of the student pre-post surveys showed statistically significant improvement in self-efficacy on key clinical functions of the EPAs.
Discussion
This study demonstrates that the AI rotation can be structured to include a Core EPA curriculum that can assess student performance utilizing WBAs of directly observed clinical skills.
Conclusions
Our clinical outcomes data demonstrates that the majority of fourth-year medical students are capable of performing advanced Core EPAs at a level acceptable for intern year by the conclusion of their AI rotations. WBA data collected can also aid in ad hoc and longitudinal summative Core EPA entrustment decisions.


Similar content being viewed by others
References
Angus S, Vu TR, Halvorsen AJ, Aiyer M, McKown K, Chmielewski AF, et al. What skills should new internal medicine interns have in July? A national survey of internal medicine residency program directors. AcadMed. 2014;89:432–5.
Young JQ, Ranji SR, Wachter RM, Lee CM, Niehaus B, Auerbach AD. “July effect”: impact of the academic year-end changeover on patient outcomes: a systematic review. AnnInternMed. 2011;155:309–15.
Englander R, Flynn T, Call S, Carraccio C, Cleary L, Fulton TB, et al. Toward defining the foundation of the MD degree: Core Entrustable Professional Activities for Entering Residency. AcadMed. 2016;91:1352–8.
Wackett A, Daroowalla F, Lu W-H, Chandran L. Reforming the 4th-year curriculum as a springboard to graduate medical training: one school’s experiences and lessons learned. Teaching and Learning in Medicine. 2016;28:192–201.
Fazio SB, Ledford CH, Aronowitz PB, Chheda SG, Choe JH, Call SA, et al. Competency-based medical education in the internal medicine clerkship: a report from the Alliance for Academic Internal Medicine Undergraduate Medical Education Task Force. Acad Med. 2018;93:421–7.
Lindeman BM, Sacks BC, Lipsett PA. Graduating students’ and surgery program directors’ views of the Association of American Medical Colleges Core Entrustable Professional Activities for Entering Residency: where are the gaps? JSurgEduc. 2015;72:e184–92.
Meyer EG, Kelly WF, Hemmer PA, Pangaro LN. The RIME model provides a context for entrustable professional activities across undergraduate medical education. Acad Med. 2018;93:954.
Benson NM, Stickle TR, Raszka WV Jr. Going “fourth” from medical school: fourth-year medical students’ perspectives on the fourth year of medical school. AcadMed. 2015;90:1386–93.
Aiyer MK, Vu TR, Ledford C, Fischer M, Durning SJ. The subinternship curriculum in internal medicine: a national survey of clerkship directors. TeachLearnMed. 2008;20:151–6.
Lindeman BM, Lipsett PA, Alseidi A, Lidor AO. Medical student subinternships in surgery: characterization and needs assessment. AmJSurg. 2013;205:175–81.
Elnicki DM, Gallagher S, Willett L, Kane G, Muntz M, Henry D, et al. Course offerings in the fourth year of medical school: how U.S. medical schools are preparing students for internship. AcadMed. 2015;90:1324–30.
Brown DR, Warren JB, Hyderi A, Drusin RE, Moeller J, Rosenfeld M, et al. Finding a path to entrustment in undergraduate medical education: a progress report from the AAMC Core Entrustable Professional Activities for Entering Residency Entrustment Concept Group. AcadMed. 2017;92:774–9.
Hauer KE, Holmboe ES, Kogan JR. Twelve tips for implementing tools for direct observation of medical trainees’ clinical skills during patient encounters. Medical Teacher. 2011;33:27–33.
Ryan MS, Santen S. Generalizability of the Ottawa Surgical Competency Operating Room Evaluation (O-SCORE) scale to assess medical student performance of the Core EPAs in the workplace. Acad Med. 2020;(accepted).
Garber AM, Ryan MS, Santen SA, Goldberg SR. Redefining the acting internship in the era of entrustment: one institution’s approach to reforming the acting internship. MedSciEduc [Internet]. 2019 [cited 2019 Mar 20]; Available from: https://doi.org/10.1007/s40670-019-00692-7.
Starmer A, Landrigan C, Srivastava R, Wilson K, Allen A, Mahant S, et al. I-PASS handoff curriculum: faculty observation tools. MedEdPORTAL [Internet]. 2013 [cited 2019 Mar 20]; Available from: https://www.mededportal.org/publication/9570/
Podolsky A, Stern DT, Peccoralo L. The courteous consult: a CONSULT card and training to improve resident consults. J Grad Med Educ. 2015;7:113–7.
Rekman J, Hamstra SJ, Dudek N, Wood T, Seabrook C, Gofton W. A new instrument for assessing resident competence in surgical clinic: the Ottawa Clinic Assessment Tool. J Surg Educ. 2016;73:575–82.
Klassen RM, Klassen JRL. Self-efficacy beliefs of medical students: a critical review. Perspect Med Educ. 2018;7:76–82.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. Journal of Biomedical Informatics. 2019;95:103208.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Funding
VCU receives funding from the Accelerating Change in Medical Education Grant from the American Medical Association. This funding was not related to this study. In addition, REDCap database access at VCU is provided through C. Kenneth and Dianne Wright Center for Clinical and Translational Research grant support (UL1TR002649).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
This study was approved by the VCU Institutional Review Board.
Informed Consent
Not applicable
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Adam M. Garber, Associate Professor of Internal Medicine at the Virginia Commonwealth University School of Medicine.
Moshe Feldman is Associate Professor and Assistant Director for Research and Evaluation, Center of Human Simulation and Patient Safety, Virginia Commonwealth University School of Medicine, Richmond, Virginia.
Michael Ryan, Associate Professor of Pediatrics and Assistant Dean for Clinical Medical Education at the Virginia Commonwealth University School of Medicine.
Sally A. Santen, Professor of Emergency Medicine and Senior Associate Dean for Evaluation, Assessment and Scholarship at the Virginia Commonwealth University School of Medicine.
Alan Dow, Associate Professor of Surgery at the Virginia Commonwealth University Health System.
Stephanie R. Goldberg is Associate Professor of Surgery at the Virginia Commonwealth University School of Medicine, Richmond, Virginia
Supplementary Information
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Garber, A.M., Feldman, M., Ryan, M. et al. Core EPAs in the Acting Internship: Early Outcomes from an Interdepartmental Experience. Med.Sci.Educ. 31, 527–533 (2021). https://doi.org/10.1007/s40670-021-01208-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-021-01208-y