Abstract
Background
Studies show that implicit bias among healthcare providers contributes to health disparities. Despite this knowledge, most medical school curricula lack formal methods for assessing and reducing implicit bias among medical students.
Purpose
The purpose of this study was to create a longitudinal, multidisciplinary training program for first-year medical students to reduce implicit bias toward skin tone, to increase awareness of personal bias, and to measure changes in bias after a targeted intervention.
Methods
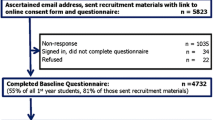
First-year medical students participated in a three-part implicit bias training program that included visits to an art museum, a lecture on medical anthropology, and an interactive sociological discussion about bias in medical research. A control group did not participate in the training. All participants took the Harvard Implicit Association Test for Skin Tone and completed a questionnaire assessing awareness of implicit bias before and after the study activities were administered.
Results
All participants indicated a bias toward light skin tone. In addition, a stronger bias score in the pre-test correlated with a stronger belief that the scores were inaccurate. Neither the experimental group nor the control group demonstrated a significant change in implicit bias, but the experimental group trended toward a decrease in bias. Power analysis suggested that significant results may have been obtained with a larger sample size. All participants indicated an awareness that implicit biases affect the provision of healthcare. When prompted to reflect on these biases, the experimental group provided richer, more detailed personal accounts of implicit bias in the healthcare environment after participating in the study.
Conclusions
First-year medical students who participated in this study were aware that implicit bias affects the provision of healthcare and therefore plays a role in perpetuating health disparities. However, they were less able to recognize bias in themselves. Providing opportunities for medical students to recognize and confront their own implicit biases is an important goal. This study suggests that a longitudinal, multidisciplinary curricular approach to building awareness and reducing implicit bias can produce promising results in medical students. We anticipate that further development and refinement of curricular activities may lead to significant results.
Similar content being viewed by others
Notes
Power analysis conducted at power of 0.8 and alpha level of 0.05.
References
Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, et al. Implicit Bias among Physicians and its Prediction of Thrombolysis Decisions for Black and White Patients. In: Society of General Internal Medicine; 2007. https://doi.org/10.1007/s11606-007-0258-5.
Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;2013:1504–10. https://doi.org/10.1007/s11606-013-2441-1.
Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med. 2018;199:219–29. https://doi.org/10.1016/j.socscimed.2017.05.009.
Hirsh AT, Hollingshead NA, Ashburn-Nardo L, Kroenke K. The interaction of patient race, provider bias, and clinical ambiguity on pain management decisions. J Pain. 2015;16:558–68. https://doi.org/10.1016/j.jpain.2015.03.003.
Hagiwara N, Slatcher RB, Eggly S, Penner LA. Physician racial bias and word use during racially discordant medical interactions. Health Commun. 2017;32:401–8. https://doi.org/10.1080/10410236.2016.1138389.
Van Ryn M, Fu SS. Paved with good intentions: do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health. 2003;93:248–55.
Johnson TJ, Hickey RW, Switzer GE, Miller E, Winger DG, Nguyen M, et al. The impact of cognitive stressors in the emergency department on physician implicit racial bias. Acad Emerg Med. 2016;23:297–305. https://doi.org/10.1111/acem.12901.
Functions and structure of a medical school: standards for accreditation of medical education programs leading to the M.D. degree. 2018. http://lcme.org/publications/. Accessed April 16, 2018.
Baker TK, Smith GS, Jacobs NN, Houmanfar R, Tolles R, Kuhls D, et al. A deeper look at implicit weight bias in medical students. Adv Health Sci Educ Theory Pract. 2017;22:889–900. https://doi.org/10.1007/s10459-016-9718-1.
Cutler JL, Harding KJ, Hutner LA, Cortland C, Graham MJ. Reducing medical students’ stigmatization of people with chronic mental illness: a field intervention at the “living museum” state hospital art studio. Acad Psychiatry. 2012;36:191–6. https://doi.org/10.1176/appi.ap.10050081.
Roberts HJ, Noble JM. Education research: changing medical student perceptions of dementia: an arts-centered experience. Neurology. 2015;85:739–41. https://doi.org/10.1212/WNL.0000000000001867.
Gast A, Rothermund K. When old and frail is not the same: dissociating category and stimulus effects in four implicit attitude measurement methods. Q J Exp Psychol. 2010;63:479–98. https://doi.org/10.1080/17470210903049963.
Kidd M, Nixon L, Rosenal T, Jackson R, Pereles L, Mitchell I, et al. Using visual art and collaborative reflection to explore medical attitudes toward vulnerable persons. Can Med Educ J. 2016;7:e22–30.
Gonzalez CM, Kim MY, Marantz PR. Implicit bias and its relation to health disparities: a teaching program and survey of medical students. Teach Learn Med. 2014;26:64–71. https://doi.org/10.1080/10401334.2013.857341.
White-Means S, Zhiyong Dong, Hufstader M, Brown LT. Cultural competency, race, and skin tone bias among pharmacy, nursing, and medical students: implications for addressing health disparities. Med Care Res Rev. 2009; https://doi.org/10.1177/1077558709333995
Burke SE, Dovidio JF, Perry SP, Burgess DJ, Hardeman RR, Phelan SM, et al. Informal training experiences and explicit bias against African Americans among medical students. Soc Psychol Q. 2017;80:65–84. https://doi.org/10.1177/0190272516668166.
Van Ryn M, Hardeman R, Phelan SM, Burgess DJ, Dovidio JF, Herrin J, et al. Medical school experiences associated with change in implicit racial bias among 3547 students: a medical student changes study report. J Gen Intern Med. 2015;30:1748–56. https://doi.org/10.1007/s11606-015-3447-7.
Leslie KF, Sawning S, Shaw MA, Martin LJ, Simpson RC, Stephens JE, et al. Changes in medical student implicit attitudes following a health equity curricular intervention. Med Teach. 2018;40:372–8. https://doi.org/10.1080/0142159X.2017.1403014.
Greenwald T, Banaji M, Nosek B, Teachman B, Nock M. Project Implicit. 2011. https://implicit.harvard.edu/implicit. .
Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97:17–41. https://doi.org/10.1037/a0015575.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
TEDx Talks. From Park Bench to Lab Bench: What kind of future are we designing? In: Ruha Benjamin Media. 2015. https://www.youtube.com/watch?v=_8RrX4hjCr0. .
Karanfilian BV, Saks NS. Measuring the effects of an observation training program for first-year medical students. Med Sci Educ. 2018;28:649–53. https://doi.org/10.1007/s40670-018-0607-5.
Acknowledgments
The authors would like to thank Ruha Benjamin, PhD; Liesel Copeland, PhD; Alfredo Franco MS; Peter Guarnaccia, PhD; Donna Gustafson, PhD; Robert Lebeau, EdD; Hanin Rashid, PhD; Victoria Wagner, MLS; and the Rutgers University Zimmerli Art Museum for making this project possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ruben, M., Saks, N.S. Addressing Implicit Bias in First-Year Medical Students: a Longitudinal, Multidisciplinary Training Program. Med.Sci.Educ. 30, 1419–1426 (2020). https://doi.org/10.1007/s40670-020-01047-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-020-01047-3