Abstract
Purpose
Atopic eczema (AE, atopic dermatitis), one of the most common chronic skin diseases worldwide, can dramatically influence the lives of affected patients as well as the lives of their families. Despite the availability of several questionnaires for assessing the impairment of quality of life, so far the emotional consequences of AE have received limited attention. The purpose therefore was to develop an instrument to assess the emotional consequences of AE in affected adults.
Methods
The Atopic Eczema Score of Emotional Consequences (AESEC) was developed based on a review of available instruments and by consulting individuals with AE about the emotional consequences of AE through social media. Validation was performed in a test-sample, followed by a large cross-sectional study in patients with AE across nine European countries. AESEC results were compared with the Patient Oriented Eczema Measure (POEM), the Dermatology Life Quality Index (DLQI) and the Hospital Anxiety and Depression Scale (HADS).
Results
A 28-item questionnaire on emotional consequences of having AE was developed. Applied to 1189 participants, AESEC showed high reliability and correlated well with DLQI, HADS and POEM. More than half (57%) of the respondents were emotionally burdened. Large to very large emotional consequences were reported by 43.8% of those with currently moderate AE, 62.2% with severe AE and 66.7% with very severe AE-symptoms.
Conclusion
AESEC is a questionnaire for assessing the emotional consequences of living with AE. It may prove useful in evaluating the burden of disease, beyond skin symptoms and time-specific quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Affecting about 1–5% of adults and 10–20% of children in Europe, Atopic eczema (AE, atopic dermatitis) is one of the most common chronic skin diseases worldwide [1,2,3]. With its chronic and relapsing nature over years and decades, sometimes even life-long, the disease can dramatically influence the lives of affected patients as well as the lives of their families [4,5,6]. Working life is negatively influenced, reflecting in increased sick leave, job choices, job changes and job losses, or even disability pensions for patients severely affected [7]. Moreover, AE can have a significant impact on patients’ quality of life and their mental health [8, 9]. In this context several studies have reported that patients can experience a substantial reduction in quality of life and can suffer from depression and other mental health disorders as measured with different screening and scoring tools [10]. In recent years, Finlay’s Dermatology Life Quality Index (DLQI) has become one of the most commonly used tools to assess quality of life in AE affected patients [11], much more than the Skindex-29 [12]. An instrument specifically designed for AE, but rarely used, is the Quality of Life Index for Atopic Dermatitis (QoLIAD) [13]. Other more generic instruments that have been used include the Short Form (SF)-36 Health Survey [14] and the SF-12 Health Survey [15].
What all of these instruments fail to capture are the emotional consequences for people living with AE and in fact, these consequences have received limited attention so far. However, there is growing evidence that these aspects of life impairment might be substantial in AE. Several recent studies have found that AE is associated with anxiety, depressive mood and depression, stress, and even suicidal ideation [16,17,18,19,20,21]. A study conducted in Germany with 181 patients with AE found a prevalence of 21.3% for suicidal ideation of affected patients with 3.9% scoring above the cut-off indicating acute suicidality [22].
Addressing the emotional aspects in affected patients requires increased emphasis from dermatologists and other healthcare specialists treating AE. However, tools to measure and assess the impact of AE on the personal emotions are still lacking. Although tools like DQLI and Skindex-29 capture emotions, these are not AE-specific and contain only a small number of items on emotional impact. QoLIAD contains 25 AE-specific items, yet not all items are on emotional consequences. The QoLIAD items are also all negatively worded, which may create negative bias, and they can only be answered with ‘yes’ or ‘no’, leaving no room for nuance. Therefore a new questionnaire was developed in order to fill this gap, carried out by the European umbrella patient organisation for AE.
Materials and methods
Development of the questionnaire items
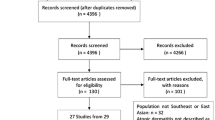
The aim of the questionnaire was to capture and measure the emotional consequences of having AE with a patient-centric view, and it therefore should reflect the situation of people living with AE. Firstly, an extensive list of items was compiled which was based on previous experience with Quality of Life studies. Secondly, through a social media group specifically for people with AE, the over 250 group members were asked for input on a specific question: ‘What personal aspects of living with atopic eczema do you think are important to know for those who do not have eczema?’ Both were combined, de-duplicated and worded as brief statements. These statements should be (re)worded in items such as: ‘I …’ or ‘My …’, should not be time specific—for example ‘Over the last week …’—and should alternate between negative and positive. As for the latter: when all statements are worded as negatives it potentially presupposes that these negatives could be applicable. And when the questionnaire is self-completed there is a possibility that participants tend to answer in the same answer-column creating negative bias. An example of an instrument that uses such alternating strategy is the much used and valued Hospital Anxiety and Depression Scale (HADS) [23]. As to force an answer and rule out the option of choosing ‘neutral’ or ‘don’t know’, the following 4‑point Likert scale was chosen: applies fully, somewhat applies, rather not, or does not apply at all. For negative statements, scoring would be from 3 (applies fully) to 0 (does not apply at all), whilst the positive statements score in reverse; as is the case with HADS. Translations from the devised questionnaire in English (Great Britain) into target languages were done by certified translators experienced in health care questionnaires and were checked by patients with AE from these countries on comprehension and correct use of terminology. A concept of the questionnaire was tested online in the five largest EU countries (target n = 100). Based on the test results, the reliability, consistency and inter-item correlations were calculated and an exploratory factor analysis was carried out. Subsequently, redundant items were deleted, resulting in the final questionnaire to be used in a larger validation study. An overview can be found in Fig. 1.
Validation and real-life study
The development and use of the emotional consequences’ questionnaire was part of a recent and larger project to assess the real-life burden of disease of people living with AE in Europe [24], principally because no other tools for this specific purpose were available. This questionnaire on emotional consequences was therefore embedded in a larger questionnaire, which included other validated instruments to assess the burden of disease, which made it possible to compare the outcomes with those other instruments. For assessing current AE severity, the Patient Oriented Eczema Measure (POEM) [25] was chosen, based on the recommendation by the Harmonising Outcomes Measures for Eczema initiative (HOME) [26]. POEM is a 7-item questionnaire measuring eczema symptoms over the past week, the scores can be categorized into (almost) clear, mild, moderate, severe and very severe, and it correlates well with physicians’ assessed severity [27]. Measurement of the effect of AE on quality of life was undertaken using the DLQI, which categorizes the impact of dermatological diseases into no effect at all on patient’s life, small effect, moderate effect, very large effect and extremely large effect [11]. To assess depressive symptoms, the 7‑items relevant to depression from the Hospital Anxiety and Depression Scale (HADS-D7) were used, in which the score can be rated as: “normal”, “borderline” or “abnormal” (indicating clinical ‘caseness’) [23].
In each country permission was requested from the local Ethics Committees and given before starting the study. Participants were recruited through physicians to ensure adherence to the inclusion criteria: 18 years or older, AE diagnosis made by a physician, current use of systemic immunomodulatory therapy or phototherapy, or candidate for systemic immunomodulatory therapy or phototherapy. Therefore these participants had moderate-to-severe AE that could not be adequately controlled by topical therapy alone, e.g. emollients and moisturisers, (very) potent topical corticosteroids and/or topical calcineurin inhibitors. The actual severity of the AE of the participant could vary, depending on the effectiveness of the therapy at the time of participation. The study was carried out in nine European countries (target n; total 1200): Czech Republic (50), Denmark (50), France (180), Germany (180), Italy (180), Netherlands (150), Spain (180), Sweden (50) and United Kingdom (180). The method of Computer Assisted Telephone Interview (CATI) was chosen to ensure a national coverage with the greatest possible evaluation quality. Fieldwork started October 2017 and was completed beginning of March 2018. During the telephone interview participants were asked—besides the questions on demographic details and the aforementioned instruments—for their response to the questions on emotional consequences. These were phrased by the interviewers as “I will now read out a number of aspects that you may feel apply or do not apply to your life with Atopic Eczema. Please tell me for each individual aspect, the degree to which it applies to your situation”.
Statistical and psychometric analyses
Development of the questionnaire, its testing and subsequent analyses involved rigorous and proven statistical analyses to ensure reliability and consistency. Analyses on the reliability and consistency of the concept questionnaire were done using Cronbach’s alpha (α) and Spearman’s rho (ρ). Furthermore an exploratory factor analysis (orthogonal/varimax) was carried out, as was an approval analysis and a sensitivity analysis with regard to AE severity. The reliability of the final questionnaire based on the real-life results from the EU study was reported on the total set with Cronbach’s α and Spearman’s ρ for inter-item correlations. Reliability was further tested with a split-half analysis. A principal component analysis (three-factor analysis, orthogonal/varimax) was carried out, including factor correlations. Correlations with HADS-D7, DLQI and POEM were calculated and reported with Spearman’s ρ. All statistical analyses were performed using SPSS software version 14.0 (IBM Corp., New York, NY, USA).
Results
Development of the questionnaire
Participation of adults living with AE through social media yielded 119 very personal and verbatim answers. These were de-duplicated and reworded into brief statements starting, if possible, with ‘I …’or ‘My …’, leaving 74 items. After careful and detailed assessment of these statements with regard to overlap, ambiguity, or cultural or language specificity, and combined with the findings from the literature review, 37 items were selected by the author team. If necessary and when linguistically possible, some statements were reworded from negative into positive, resulting in a fair balance between the two. During the whole process, a native English speaker experienced in developing questionnaires was involved.
Between 18 and 22 August 2017, 103 people with AE (53.4% female/46.6% male, mean age 42 years [SD 14.3], age range 20–87) in France, Germany, Italy, Spain and the United Kingdom (20% in each country) answered the 37-item concept questionnaire online to enable its testing. Self-assessed disease severity was reported as 10.7% (almost) clear, 29.1% mild, 49.5% moderate and 10.7% severe. The internal consistency and reliability of the questionnaire was excellent (α = 0.938; based on moderate to severe AE: n = 62), even when divided into parts. The sets of negative and positive items were each appraised on the approval rate and the differences between those with mild versus moderate/severe AE. Exploratory factor analysis (orthogonal/varimax) found four possible factors (cheerful/carefree, suffering/worried, overstrained, ashamed/insecure) and reliability and sensitivity analyses were carried out within each group. Furthermore, redundant items with high correlations (calculated with Spearman’s ρ) were identified.
After careful consideration of all possible choices without forfeiting reliability, internal consistency or diversity, and adhering to the prespecified patient-centric requirements, 28 of the 37 items were selected by the author team by means of consensus, resulting in an item-set with excellent internal consistency and reliability (α = 0.929), and low inter-item correlation (ρ = 0.224).
Participants EU study
A total of 1189 adults with AE (mean age 42.1 [SD 11.1], range 18–87 years; 56.3% women and 43.7% men) were interviewed (Table 1: participants’ characteristics). Participants originated from Czech Republic (52), Denmark (50), France (180), Germany (180), Italy (180), Netherlands (150), Spain (180), Sweden (37) and United Kingdom (180). The majority were recruited through physicians (84%) and in certain instances, in view of restrictive country regulations or infeasibility, other means of recruitment were necessary, e.g. via support groups or recommendation. This did not compromise adherence to inclusion criteria, as the screening questions ensured eligibility. To test this adherence, the sample from the Netherlands was analysed where 48.7% were recruited through physicians and 51.3% through support groups, and data showed hardly any noticeable structural differences.
AESEC psychometrics
The reliability of the total 28-item AESEC questionnaire was high (α = 0.900) with low inter-item correlation (ρ = 0.208). To further examine the reliability, a split-analysis was performed: reliability was high for both halves (α = 0.853 and 0.842, respectively). The equal length Spearman–Brown coefficient was 0.915, which is well over the acceptable 0.80. A factor analysis (principal component, orthogonal/varimax) was carried out (Table 2). The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.952 and Bartlett’s test of sphericity was significant (χ2 = 11,713.89, df = 378, p < 0.0005), indicating an adequate sample for factor analysis. The analysis yielded three factors with adequate loading of the 28-items over these factors, and there was no correlation between the three factors. The factors could be described as desperate/burdened, insecure/worried and balanced/satisfied. The reliability of the factors was high (α = 0.802–0.882) with a weak/moderate inter-item correlation (ρ = 0.294–0.428). The correlations with POEM, DLQI and HADS-D7 were significant and were moderate with HADS-D7 (ρ = 0.540), moderate with DLQI (ρ = 0.546) and moderate with POEM (ρ = 0.466), providing an indication of construct validity (Table 3).
AESEC score banding
The mean AESEC score of the 1189 participants was 32.2 (SD 14.1; median 31) out of 0–84 (higher means more consequences). In order to give meaning to these AESEC scores, we wanted to categorize these scores into ‘no/small effect’, ‘moderate effect’, ‘large effect’ and ‘very large effect’. The anchors we could use to categorize the scores were the POEM and DLQI scores, although the correlations were only moderate. In order to find suitable cut-off values, we used the receiver operating characteristic (ROC) curves of DLQI and POEM scores versus the total AESEC score, with some assumptions. One assumption was that participants who reported ‘no effect’ on quality of life measured by DLQI should not fall into the AESEC categories ‘large effect’ and ‘very large effect’, making the optimum cut-off value to be about 40. Applying the same for the POEM score ‘Clear to almost clear’, also demonstrated an optimum around 40. Likewise, we assumed that participants with a ‘small effect’ on quality of life should not fall into the category ‘very large effect’ on emotional consequences, demonstrating cut-off values between 50 and 53. As for the cut-off values between the categories ‘no/small effect’ and ‘moderate effect’, the optimum according to ROC analyses seemed to be between 27 and 30, for both DLQI and POEM. This was in line with the visual inspection of the data (Fig. 2).
AESEC score versus mean DLQI/POEM scores—two scenarios for AESEC banding. Not all scores of AESEC (0–84) were reported: score 1 was missing and between 71 and 84 eight were missing. To not distort the trend line, mean scores of POEM and DLQI for these AESEC scores were imputed with the method of last value carried forward
The ROC exercise resulted in two choices: (1) 0–27 or 0–30 for ‘no/small effect’ and therefore 28–40 or 30–40 for ‘moderate effect’; (2) 40–50 or 40–52 for ‘large effect’ and therefore 50–84 or 53–84 for a ‘very large effect’. We analysed per AESEC category how these choices would affect the proportion of participants with regard to their severity scores of DLQI, POEM and HADS-D7. The comparison was in favour of the cut-off values 0–27 for ‘no/small effect’, 28–40 for ‘moderate effect’, 40–52 for ‘large effect’ and 53–84 for a ‘very large effect’, as this did more justice to the severity scores of DLQI, POEM and HADS (Table 4).
AESEC total scores
Of the 1189 participants, 512 (43.1%) individuals scored ‘no/small consequences’, 320 (26.9%) ‘moderate consequences’, 252 (21.2%) ‘large consequences’ and 105 (8.8%) ‘very large consequences’ (Table 5). Regardless of disease severity 56.9% of the participants reported moderate to very large emotional consequences due to living with AE. Yet those participants who experienced moderate to very severe AE symptoms, reported major effects on their lives: large to very large consequences were reported in 43.8% with moderate symptoms, 62.2% with severe symptoms and 66.7% in those with very severe AE symptoms (Table 6).
AESEC item scores
The top 5 negative items mentioned were the following: 72% of the participants reported envy of people with normal skin, 57% that itching drove them crazy, 51% tried to hide their eczema, 50% was sad due to their eczema and 43% reported that eczema made them angry (Fig. 3; Table 7). As for the top 3 positively phrased items, 39% reported to have problems with intimacy, 27% that they cannot do what other people can do, and 25% do not feel in control of their eczema (Fig. 4; Table 7).
Discussion
The AESEC questionnaire is the first available tool to specifically assess and measure the emotional consequences of people living with AE. AESEC addresses an unmet need and has shown that a scoring system on this issue was overdue: More than half (57%) of the participants are emotionally burdened, which is a new finding in the literature.
Within the last few years there have been substantial new discoveries in AE research which have made the development of new treatment strategies possible [19, 20, 28,29,30,31,32,33]. With the introduction of new treatment options and especially the approval of the first biologic for AE in the USA and EU, financial discussions have emerged [34, 35]. All the more important are full evaluations and characterizations of AE beyond the skin symptoms. AE can affect several aspects of life, which has to be acknowledged in dermatological assessment and in choosing the best treatment for every individual with AE based on their specific needs.
Most of the previously available scoring systems for quality of life in general are based on everyday life activities and are time-specific. The DLQI for example is an excellent tool to get a first impression of quality of life in affected patients. However, the 10 questions covering symptoms, home care and shopping, social leisure, personal relationships, sexuality, treatment and embarrassment do not fully cover the impact of AE on individuals’ lives affected by AE. Especially since the majority have AE (almost) all their lives, and also self-management has an impact. In addition, missing days at work, and anxiety in partnerships and families due to AE, have a negative influence on personal well-being and emotional health [14, 16, 17]. This became evident in our study because DLQI only moderately correlated with AESEC. The goal of all healthcare professionals should therefore be not only to treat the affected skin of patients with AE but rather go beyond the skin with a target-oriented approach based on individual suffering. This is in line with the recent report ‘Rosacea: beyond the visible’ that concluded that absence of symptoms of rosacea—a chronic skin condition affecting the face—does not necessarily mean that quality of life is not impaired [38]. For assessing the emotional consequences of living with AE, the AESEC can be used, giving insight into the emotional burden, both as an overall score or, if wanted, in more detail. The results of our study clearly reveal that this burden is substantial.
AESEC is per design structured in both negative and positive statements, as previously explained, unlike DLQI, Skindex-29 and QoLIAD. On some aspects this was a bold choice, as for example it did not enquire if people with AE had problems with intimacy, yet they were purposely asked to answer to the statement ‘I have no problem with intimacy’, which is innately a different question. Therefore, items that are positively phrased really reveal negative emotions when they were answered with ‘rather not’ or ‘does not apply at all’. These negative scores on the positively phrased items underline previous publications which seek to address psychosocial aspects of AE by for example patient education programmes [16, 36, 37] The most commonly reported items revealing negative emotions were “I try to hide my eczema”, “I envy people with normal skin” and “I feel sad about having eczema”, which clearly show the burden of disease that should be considered by all healthcare professionals treating AE.
One of the main strengths of the study is the inclusion of over one thousand patients with AE across nine European countries. Furthermore, the methodology of development and validation by including patients via social media proved, in our opinion, to be very powerful to really be able to grasp the emotional burden of people living with AE and what typically distresses them in daily life. However, the method of telephone interviewing might have also led to interviewer, recall and social desirability bias. Patients might have understated their negative feelings with an unknown interviewer. A further limitation might be the inclusion of people with AE whose disease cannot be adequately controlled with topical treatment, focusing therefore on people with a more severe form of AE. Looking at the severity of the AE symptoms at the time of participation measured with POEM, it is clear that although including participants who are innately moderately to severely affected, there is a variance from almost no symptoms to severe symptoms. Whether this effect is due to systemic immunomodulatory treatment or phototherapy—or a short course of oral corticosteroids—cannot be established based on the data, and is beyond the scope of the study. Yet this variance enabled us to measure emotional consequences of having a more severe form of AE whilst covering the whole spectrum of disease severity.
There are also some limitations regarding the methodology. It was not feasible within this study to do a ‘test–retest procedure’ to further examine the reliability of the AESEC questionnaire. This was due to the large sample and the chosen method of Computer Assisted Telephone Interview. Nor could we therefore investigate the responsiveness of the questionnaire. Both aspects (test–retest and responsiveness) could be subjects for further studies. There is also a limitation with the method of categorizing the AESEC scores into no/small, moderate, large or very large impact. Ideally one would use the methodology that was applied to DLQI [39] and POEM [27], yet the anchors in this study (POEM, DLQI, self-assessed severity) were not suitable to be able to do so. Although we are of the opinion we found the best cut-off values, it might be valuable to address this in another study.
In conclusion, AESEC is a new tool for assessing the emotional consequences of living with AE. AESEC could prove useful in the full assessment of living with AE beyond objective symptoms and time-specific, general quality of life, which becomes more and more essential, especially in times of several new systemic treatment options for AE on the rise.
Abbreviations
- AE:
-
Atopic eczema (atopic dermatitis)
- AESEC:
-
Atopic Eczema Score of Emotional Consequences
- CATI:
-
Computer Assisted Telephone Interview
- DLQI:
-
Dermatology Life Quality Index
- HADS:
-
Hospital Anxiety and Depression Scale
- HOME:
-
Harmonising Outcomes Measures for Eczema initiative
- POEM:
-
Patient Oriented Eczema Measure
- QoLIAD:
-
Quality of Life Index for Atopic Dermatitis
- ROC:
-
Receiver operating characteristic
- SD:
-
Standard deviation
- SF:
-
Short form
References
Weidinger S, Novak N. Atopic dermatitis. Lancet. 2016;387:1109–22.
Barbarot S, Auziere S, Gadkari A, Girolomoni G, Puig L, Simpson EL, et al. Epidemiology of atopic dermatitis in adults: results from an international survey. Allergy. 2018;73:1284–93.
Ring J, Ruzicka Th, Przybilla B, editors. Handbook of atopic eczema. Berlin New York: Springer; 2006.
Sampogna F, Finlay AY, Salek SS, Chernyshov P, Dalgard FJ, Evers AWM, et al. Measuring the impact of dermatological conditions on family and caregivers: a review of dermatology-specific instruments. J Eur Acad Dermatol Venereol. 2017;31:1429–39.
Drucker AM, Wang AR, Li WQ, Sevetson E, Block JK, Qureshi AA. The burden of atopic dermatitis: summary of a report for the national eczema association. J Invest Dermatol. 2017;137:26–30.
Ring J. Atopic dermatitis—eczema. Berlin New York: Springer; 2016.
Nørreslet LB, Ebbehøj NE, Ellekilde BJP, Thomsen SF, Agner T. The impact of atopic dermatitis on work life—a systematic review. J Eur Acad Dermatol Venereol. 2018;32:23–38.
Silverberg JI, Gelfand JM, Margolis DJ, Boguniewicz M, Fonacier L, Grayson MH, et al. Patient-burden and quality of life in atopic dermatitis in US adults: a population-based cross-sectional study. Ann Allergy Asthma Immunol. 2018;3:340–7.
Steinke S, Beikert FC, Langenbruch A, Fölster-Holst R, Ring J, Schmitt J, et al. Measurement of healthcare quality in atopic dermatitis—development and application of a set of quality indicators. J Eur Acad Dermatol Venereol. 2018;12:2237–2243
Yaghmaie P, Koudelka CW, Simpson EL. Mental health comorbidity in patients with atopic dermatitis. J Allergy Clin Immunol. 2013;131:428–33.
Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210–6.
Chren MM, Lasek RJ, Flocke SA, Zyzanski SJ. Improved discriminative and evaluative capability of a refined version of Skindex, a quality-of-life instrument for patients with skin diseases. Arch Dermatol. 1997;133:1433–40.
Whalley D, McKenna SP, Dewar AL, Erdman RA, Kohlmann T, Niero M, et al. A new instrument for assessing quality of life in atopic dermatitis: international development of the Quality of Life Index for Atopic Dermatitis (QoLIAD). Br J Dermatol. 2004;150:274–83.
Kiebert G, Sorensen SV, Revicki D, Fagan SC, Doyle JJ, Cohen J, et al. Atopic dermatitis is associated with a decrement in health-related quality of life. Int J Dermatol. 2002;41:151–8.
Warschburger P, Buchholz HT, Petermann F. Psychological adjustment in parents of young children with atopic dermatitis: which factors predict parental quality of life? Br J Dermatol. 2004;150:304–11.
Lee SH, Lee SH, Lee SY, Lee B, Lee SH, Park YL. Psychological health status and health-related quality of life in adults with atopic dermatitis: a nationwide cross-sectional study in South Korea. Acta Derm Venereol. 2018;98:89–97.
Thyssen JP, Hamann CR, Linneberg A, Dantoft TM, Skov L, Gislason GH, et al. Atopic dermatitis is associated with anxiety, depression, and suicidal ideation, but not with psychiatric hospitalization or suicide. Allergy. 2018;73:214–20.
Dieris-Hirche J, Gieler U, Kupfer JP, Milch WE. Suicidal ideation, anxiety and depression in adult patients with atopic dermatitis. Hautarzt. 2009;60:641–6.
Wollenberg A, Barbarot S, Bieber T, Christen-Zaech S, Deleuran M, Fink-Wagner A, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. J Eur Acad Dermatol Venereol. 2018;32:657–82.
Wollenberg A, Barbarot S, Bieber T, Christen-Zaech S, Deleuran M, Fink-Wagner A, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part II. J Eur Acad Dermatol Venereol. 2018;32:850–78.
Pärna E, Aluoja A, Kingo K. Quality of life and emotional state in chronic skin disease. Acta Derm Venereol. 2015;95:312–6.
Dieris-Hirche J, Gieler U, Petrak F, Milch W, Te Wildt B, Dieris B, et al. Suicidal ideation in adult patients with atopic dermatitis: a German cross-sectional study. Acta Derm Venereol. 2017;97:1189–95.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
Ring J, Zink A, Arents BWM, Seitz IA, Mensing U, Schielein MC, et al. Atopic eczema: burden of disease and individual suffering—results from a large EU-study in adults. J Eur Acad Dermatol Venereol. 2019. https://doi.org/10.1111/jdv.15634
Charman CR, Venn AJ, Williams HC. The patient-oriented eczema measure: development and initial validation of a new tool for measuring atopic eczema severity from the patients’ perspective. Arch Dermatol. 2004;140:1513–9.
Spuls PI, Gerbens LA, Simpson E, Apfelbacher CJ, Chalmers JR, Thomas KS, et al. POEM a core instrument to measure symptoms in clinical trials: a HOME statement. Br J Dermatol. 2017;4:979–84.
Charman CR, Venn AJ, Ravenscroft JC, Williams HC. Translating Patient-Oriented Eczema Measure (POEM) scores into clinical practice by suggesting severity strata derived using anchor-based methods. Br J Dermatol. 2013;6:1326–32.
Lauffer F, Ring J. Target-oriented therapy: emerging drugs for atopic dermatitis. Expert Opin Emerg Drugs. 2016;21:81–9.
Zink A, Gensbaur A, Zirbs M, Seifert F, Suarez IL, Mourantchanian V, et al. Targeting IgE in severe atopic dermatitis with a combination of Immunoadsorption and Omalizumab. Acta Derm Venereol. 2016;96:72–6.
Ruiz-Villaverde R, Dominguez-Cruz J, Armario-Hita JC, Martinez-Pilar L, Alcantara-Luna S, Dupilumab P‑RJJ. Short-term effectiveness and security in real clinical practice. A retrospective multicentric study. J Eur Acad Dermatol Venereol. 2019;1:e21–2.
Bieber T, D’Erme AM, Akdis CA, Traidl-Hoffmann C, Lauener R, Schäppi G, et al. Clinical phenotypes and endophenotypes of atopic dermatitis: where are we, and where should we go? J Allergy Clin Immunol. 2017;139:58–64.
Scheerer C, Eyerich K. Pathogenesis of atopic dermatitis. Hautarzt. 2018;69:191–6.
Subramanian I, Singh VK, Jere A. Elucidating mechanistic insights into drug action for atopic dermatitis: a systems biology approach. Bmc Dermatol. 2018;18:3.
Werfel T, Wollenberg A, Pumnea T, Heratizadeh A. New aspects in systemic treatment of atopic dermatitis. Hautarzt. 2018;69:217–24.
Schielein MC, Tizek L, Rotter M, Konstantinow A, Biedermann T, Zink A. Guideline-compliant prescription of biologicals and possible barriers in dermatological practices in Bavaria. J Eur Acad Dermatol Venereol. 2018;32:978–84.
Heratizadeh A, Werfel T, Gieler U, Kupfer J. Arbeitsgemeinschaft Neurodermitisschulung für Erwachsene (ARNE). [Patient education for adults with atopic dermatitis according to the ARNE concept. Hautarzt. 2018;69:225–31.
Lewis-Jones S. Quality of life and childhood atopic dermatitis: the misery of living with childhood eczema. Int J Clin Pract. 2006;60:984–92.
Tan J, Steinhoff M, Bewley A, Rosacea GU. Beyond the visible online report. 2019. http://hosted.bmj.com/rosaceabeyondthevisible. Accessed 04.2019.
Hongbo Y, Thomas CL, Harrison MA, Salek MS, Finlay AY. Translating the science of quality of life into practice: what do dermatology life quality index scores mean? J Invest Dermatol. 2005;4:659–64.
Acknowledgements
We are grateful to Mathew Francis for his valuable contribution to the development of the questionnaire.
Funding
Unrestricted educational grants for this study were provided by Sanofi Genzyme and Regeneron.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B.W.M. Arents, U. Mensing, I.A. Seitz, N. Wettemann, A. H. Fink-Wagner, G. de Carlo, A. Zink and J. Ring declare that they have no competing interests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Arents, B.W.M., Mensing, U., Seitz, I.A. et al. Atopic eczema score of emotional consequences—a questionnaire to assess emotional consequences of atopic eczema. Allergo J Int 28, 277–288 (2019). https://doi.org/10.1007/s40629-019-0098-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40629-019-0098-y