Abstract
Purpose
The effect of the sodium-glucose 2 (SGLT-2) inhibitors on microvascular complications remains uncertain. We performed a systematic review to determine the efficacy of the SGLT-2 inhibitors on microvascular outcomes in patients with type 2 diabetes.
Methods
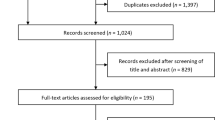
A comprehensive search was performed using Ovid, MEDLINE, EMBASE, Web of Science, and Scopus from inception to May 2019. Randomized trials comparing SGLT-2 inhibitors with placebo or other medication for type 2 diabetes for ≥ 4 weeks were included. Diabetes-related microvascular complications such as nephropathy, retinopathy, neuropathy, and peripheral vascular disease were evaluated. A random-effect model using mean differences for continuous outcomes and risk ratio for dichotomous outcomes was used to synthesize data. PROSPERO (CRD 42017076460).
Results
A total of 40 RCTs with overall moderate quality of evidence were included. SGLT-2 inhibitors reduced the risk of renal-replacement therapy (0.65; 95% CI 0.54–0.79), renal death (0.57; 95% CI 0.49–0.65), and progression of albuminuria (0.69; 95% CI 0.66–0.73). Conversely, they appeared ineffective in maintaining eGFR (0.33; 95% CI − 0.74 to 1.41) or reducing serum creatinine (− 0.07; 95% CI − 0.26 to 0.11), whereas urine albumin–creatinine ratio (− 23.4; 95% CI − 44.6 to − 2.2) was reduced. Risk of amputation was non-significant (1.30; 95% CI 0.93–1.83). No available data were found regarding neuropathy and retinopathy to perform a quantitative analysis.
Conclusion
SGLT-2 inhibitors may reduce the risk of renal patient-important outcomes but fail to improve surrogate outcomes. Apparently, no increased risk of amputations was observed with these medications. No data were available regarding other microvascular complications.




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
McKinlay J, Marceau L (2000) US public health and the 21st century: diabetes mellitus. Lancet 356(9231):757–761
Zimmet P (2003) The burden of type 2 diabetes: are we doing enough. Diabetes Metab 29(4 Pt 2):6s9-18
Singleton JR, Smith AG, Russell JW, Feldman EL (2003) Microvascular complications of impaired glucose tolerance. Diabetes 52(12):2867–2873
Fowler MJ (2008) Microvascular and macrovascular complications of diabetes. Clin Diabetes 26(2):77–82
King H, Aubert RE, Herman WH (1998) Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care 21(9):1414–1431
Glycemic Targets: < em > standards of medical care in diabetes—2018 </em > . Diabetes Care. 2018;41(Supplement 1):S55–S64
Garber AJ, Abrahamson MJ, Barzilay JI et al (2013) American association of clinical endocrinologists’ comprehensive diabetes management algorithm 2013 consensus statement–executive summary. Endocr Pract 19(3):536–557
Rodriguez-Gutierrez R, Montori VM (2016) Glycemic control for patients with type 2 diabetes mellitus: our evolving faith in the face of evidence. Circ Cardiovasc Qual Outcomes 9(5):504–512
Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M et al (2011) Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ 343:d4169
Coca SG, Ismail-Beigi F, Haq N, Krumholz HM, Parikh CR (2012) Role of intensive glucose control in development of renal end points in type 2 diabetes mellitus: systematic review and meta-analysis intensive glucose control in type 2 diabetes. Arch Intern Med 172(10):761–769
Marso SP, Bain SC, Consoli A et al (2016) Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 375(19):1834–1844
Marso SP, Daniels GH, Brown-Frandsen K et al (2016) Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 375(4):311–322
Neal B, Perkovic V, Mahaffey KW et al (2017) Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377(7):644–657
Zinman B, Wanner C, Lachin JM et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373(22):2117–2128
Cherney D, Lund SS, Perkins BA et al (2016) The effect of sodium glucose cotransporter 2 inhibition with empagliflozin on microalbuminuria and macroalbuminuria in patients with type 2 diabetes. Diabetologia 59(9):1860–1870
Cherney DZI, Zinman B, Inzucchi SE et al (2017) Effects of empagliflozin on the urinary albumin-to-creatinine ratio in patients with type 2 diabetes and established cardiovascular disease: an exploratory analysis from the EMPA-REG OUTCOME randomised, placebo-controlled trial. Lancet Diabetes Endocrinol 5(8):610–621
Dziuba J, Alperin P, Racketa J et al (2014) Modeling effects of SGLT-2 inhibitor dapagliflozin treatment versus standard diabetes therapy on cardiovascular and microvascular outcomes. Diabetes Obes Metab 16(7):628–635
Ott C, Jumar A, Striepe K et al (2017) A randomised study of the impact of the SGLT2 inhibitor dapagliflozin on microvascular and macrovascular circulation. Cardiovasc Diabetol 16:26
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Dorsey-Treviño EG, Contreras-Garza BM, González-González JG et al (2018) Systematic review and meta-analysis of the effect of SGLT-2 inhibitors on microvascular outcomes in patients with type 2 diabetes: a review protocol. BMJ Open 8(6):e020692
McGinn T, Wyer PC, Newman TB, Keitz S, Leipzig R, For GG (2004) Tips for learners of evidence-based medicine: 3. Measures of observer variability (kappa statistic). CMAJ 171(11):1369–1373
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14(1):135
Julian PTH, Sally G (2008) Cochrane handbook for systematic reviews of interventions. https://handbook-5-1.cochrane.org/. Accessed 8 May 2019
Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration [computer program]. The Netherlands 2014
Yang XP, Lai D, Zhong XY, Shen HP, Huang YL (2014) Efficacy and safety of canagliflozin in subjects with type 2 diabetes: systematic review and meta-analysis. Eur J Clin Pharmacol 70(10):1149–1158
Rosenstock J, Jelaska A, Zeller C, Kim G, Broedl UC, Woerle HJ (2015) Impact of empagliflozin added on to basal insulin in type 2 diabetes inadequately controlled on basal insulin: a 78-week randomized, double-blind, placebo-controlled trial. Diabetes Obes Metab 17(10):936–948
Rosenstock J, Vico M, Wei L, Salsali A, List JF (2012) Effects of dapagliflozin, an SGLT2 inhibitor, on HbA1c, body weight, and hypoglycemia risk in patients with type 2 diabetes inadequately controlled on pioglitazone monotherapy. Diabetes Care 35(7):1473–1478
Roden M, Weng J, Eilbracht J et al (2013) Empagliflozin monotherapy with sitagliptin as an active comparator in patients with type 2 diabetes: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol 1(3):208–219
Puckrin R, Saltiel MP, Reynier P, Azoulay L, Yu OHY, Filion KB (2018) SGLT-2 inhibitors and the risk of infections: a systematic review and meta-analysis of randomized controlled trials. Acta Diabetol 55(5):503–514
Pace DJ, Dukleska K, Phillips S, Gleason V, Yeo CJ (2018) Euglycemic diabetic ketoacidosis due to sodium-glucose cotransporter 2 inhibitor use in two patients undergoing pancreatectomy. J Pancreat Cancer 4(1):95–99
Wu JH, Foote C, Blomster J et al (2016) Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular events, death, and major safety outcomes in adults with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 4(5):411–419
Fitchett D (2017) SGLT2 inhibitors in the real world: too good to be true? Lancet Diabetes Endocrinol 5(9):673–675
Guyatt G, Rennie D, Meade M, Cook D (2002) Users’ guides to the medical literature: a manual for evidence-based clinical practice, vol 706. AMA Press, Chicago
Murad M, Montori VM, Ioannidis JA et al (2014) How to read a systematic review and meta-analysis and apply the results to patient care: users’ guides to the medical literature. JAMA 312(2):171–179
Fioretto P, Zambon A, Rossato M, Busetto L, Vettor R (2016) SGLT2 Inhibitors and the diabetic kidney. Diabetes Care 39(Suppl 2):S165–S171
Kawanami D, Matoba K, Takeda Y et al (2017) SGLT2 inhibitors as a therapeutic option for diabetic nephropathy. Int J Mol Sci 18(5):1083
Dekkers CCJ, Gansevoort RT, Heerspink HJL (2018) New diabetes therapies and diabetic kidney disease progression: the role of SGLT-2 inhibitors. Curr Diab Rep 18(5):27
Helal I, Fick-Brosnahan GM, Reed-Gitomer B, Schrier RW (2012) Glomerular hyperfiltration: definitions, mechanisms and clinical implications. Nat Rev Nephrol 8(5):293–300
Sangoi MB, de Carvalho JA, Tatsch E et al (2016) Urinary inflammatory cytokines as indicators of kidney damage in type 2 diabetic patients. Clin Chim Acta 460:178–183
Wolkow PP, Niewczas MA, Perkins B et al (2008) Association of urinary inflammatory markers and renal decline in microalbuminuric type 1 diabetics. J Am Soc Nephrol 19(4):789–797
Sano M, Takei M, Shiraishi Y, Suzuki Y (2016) Increased hematocrit during sodium-glucose cotransporter 2 inhibitor therapy indicates recovery of tubulointerstitial function in diabetic kidneys. J Clin Med Res 8(12):844–847
Devineni D, Curtin CR, Marbury TC et al (2015) Effect of hepatic or renal impairment on the pharmacokinetics of canagliflozin, a sodium glucose co-transporter 2 inhibitor. Clin Ther 37(3):610.e614–628.e614
Scheen AJ (2015) Pharmacokinetics, pharmacodynamics and clinical use of SGLT2 inhibitors in patients with type 2 diabetes mellitus and chronic kidney disease. Clin Pharmacokinet 54(7):691–708
Araki E, Onishi Y, Asano M, Kim H, Yajima T (2017) Efficacy and safety of dapagliflozin over 1 year as add-on to insulin therapy in Japanese patients with type 2 diabetes: the DAISY (Dapagliflozin added to patients under insulin therapy) trial. Diabetes Obes Metab 19(4):562–570
Aronson R, Frias J, Goldman A, Darekar A, Lauring B, Terra SG (2018) Long-term efficacy and safety of ertugliflozin monotherapy in patients with inadequately controlled T2DM despite diet and exercise: vERTIS MONO extension study. Diabetes Obes Metab 20(6):1453–1460
Bailey CJ, Gross JL, Hennicken D, Iqbal N, Mansfield TA, List JF (2013) Dapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trial. BMC Med 11:43
Barnett AH, Mithal A, Manassie J et al (2014) Efficacy and safety of empagliflozin added to existing antidiabetes treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol 2(5):369–384
Cho KY, Nakamura A, Omori K et al (2019) Effect of switching from pioglitazone to the sodium glucose co-transporter-2 inhibitor dapagliflozin on body weight and metabolism-related factors in patients with type 2 diabetes mellitus: an open-label, prospective, randomized, parallel-group comparison trial. Diabetes Obes Metab 21(3):710–714
Dagogo-Jack S, Liu J, Eldor R et al (2018) Efficacy and safety of the addition of ertugliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin and sitagliptin: the VERTIS SITA2 placebo-controlled randomized study. Diabetes Obes Metab 20(3):530–540
DeFronzo RA, Lewin A, Patel S et al (2015) Combination of empagliflozin and linagliptin as second-line therapy in subjects with type 2 diabetes inadequately controlled on metformin. Diabetes Care 38(3):384–393
Ferrannini E, Ramos SJ, Salsali A, Tang W, List JF (2010) Dapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: a randomized, double-blind, placebo-controlled, phase 3 trial. Diabetes Care 33(10):2217–2224
Fioretto P, Del Prato S, Buse JB et al (2018) Efficacy and safety of dapagliflozin in patients with type 2 diabetes and moderate renal impairment (chronic kidney disease stage 3A): the DERIVE Study. Diabetes Obes Metab 20(11):2532–2540
Forst T, Guthrie R, Goldenberg R et al (2014) Efficacy and safety of canagliflozin over 52 weeks in patients with type 2 diabetes on background metformin and pioglitazone. Diabetes Obes Metab 16(5):467–477
Grunberger G, Camp S, Johnson J et al (2018) Ertugliflozin in patients with stage 3 chronic kidney disease and type 2 diabetes mellitus: the VERTIS RENAL randomized study. Diabetes Ther 9(1):49–66
Hayashi T, Fukui T, Nakanishi N et al (2017) Dapagliflozin decreases small dense low-density lipoprotein-cholesterol and increases high-density lipoprotein 2-cholesterol in patients with type 2 diabetes: comparison with sitagliptin. Cardiovasc Diabetol 16(1):8
Han KA, Chon S, Chung CH et al (2018) Efficacy and safety of ipragliflozin as an add-on therapy to sitagliptin and metformin in Korean patients with inadequately controlled type 2 diabetes mellitus: a randomized controlled trial. Diabetes Obes Metab 20(10):2408–2415
Hattori S (2018) Empagliflozin decreases remnant-like particle cholesterol in type 2 diabetes patients with insulin resistance. J Diabetes Investigation 9(4):870–874
Hollander P, Liu J, Hill J et al (2018) Ertugliflozin compared with glimepiride in patients with type 2 diabetes mellitus inadequately controlled on metformin: the VERTIS SU randomized study. Diabetes Ther 9(1):193–207
Ito D, Shimizu S, Inoue K et al (2017) Comparison of ipragliflozin and pioglitazone effects on nonalcoholic fatty liver disease in patients with type 2 diabetes: a randomized, 24-week, open-label, active-controlled trial. Diabetes Care 40(10):1364–1372
Jabbour SA, Frias JP, Hardy E et al (2018) Safety and efficacy of exenatide once weekly plus dapagliflozin once daily versus exenatide or dapagliflozin alone in patients with type 2 diabetes inadequately controlled with metformin monotherapy: 52-week results of the duration-8 randomized controlled trial. Diabetes Care 41(10):2136–2146
Kario K, Hoshide S, Okawara Y et al (2018) Effect of canagliflozin on nocturnal home blood pressure in Japanese patients with type 2 diabetes mellitus: the SHIFT-J study. J Clin Hypertens (Greenwich) 20(10):1527–1535
Kohan DE, Fioretto P, Tang W, List JF (2014) Long-term study of patients with type 2 diabetes and moderate renal impairment shows that dapagliflozin reduces weight and blood pressure but does not improve glycemic control. Kidney Int 85(4):962–971
Kovacs CS, Seshiah V, Merker L et al (2015) Empagliflozin as add-on therapy to pioglitazone with or without metformin in patients with type 2 diabetes mellitus. Clin Ther 37(8):1773-1788.e1771
Kuchay MS, Krishan S, Mishra SK et al (2018) Effect of empagliflozin on liver fat in patients with type 2 diabetes and nonalcoholic fatty liver disease: a randomized controlled trial (E-LIFT trial). Diabetes Care 41(8):1801–1808
Lambers Heerspink HJ, de Zeeuw D, Wie L, Leslie B, List J (2013) Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetes. Diabetes Obes Metab 15(9):853–862
Lavalle-Gonzalez FJ, Januszewicz A, Davidson J et al (2013) Efficacy and safety of canagliflozin compared with placebo and sitagliptin in patients with type 2 diabetes on background metformin monotherapy: a randomised trial. Diabetologia 56(12):2582–2592
List JF, Woo V, Morales E, Tang W, Fiedorek FT (2009) Sodium-glucose cotransport inhibition with dapagliflozin in type 2 diabetes. Diabetes Care 32(4):650–657
Lu CH, Min KW, Chuang LM, Kokubo S, Yoshida S, Cha BS (2016) Efficacy, safety, and tolerability of ipragliflozin in Asian patients with type 2 diabetes mellitus and inadequate glycemic control with metformin: results of a phase 3 randomized, placebo-controlled, double-blind, multicenter trial. J Diabetes Investig 7(3):366–373
Nomoto H, Miyoshi H, Sugawara H et al (2017) A randomized controlled trial comparing the effects of dapagliflozin and DPP-4 inhibitors on glucose variability and metabolic parameters in patients with type 2 diabetes mellitus on insulin. Diabetol Metab Syndr 9:54
Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 0(0):null
Perna S, Mainardi M, Astrone P, et al. (2018) 12-month effects of incretins versus SGLT2-Inhibitors on cognitive performance and metabolic profile. A randomized clinical trial in the elderly with type-2 diabetes mellitus. Clin Pharmacol. 10:141–151
Ridderstrale M, Rosenstock J, Andersen KR, Woerle HJ, Salsali A (2018) Empagliflozin compared with glimepiride in metformin-treated patients with type 2 diabetes: 208-week data from a masked randomized controlled trial. Diabetes Obes Metab 20(12):2768–2777
Shimizu M, Suzuki K, Kato K et al (2019) Evaluation of the effects of dapagliflozin, a sodium-glucose co-transporter-2 inhibitor, on hepatic steatosis and fibrosis using transient elastography in patients with type 2 diabetes and non-alcoholic fatty liver disease. Diabetes Obes Metab 21(2):285–292
Softeland E, Meier JJ, Vangen B, Toorawa R, Maldonado-Lutomirsky M, Broedl UC (2017) Empagliflozin as add-on therapy in patients with type 2 diabetes inadequately controlled with linagliptin and metformin: a 24-week randomized, double-blind, parallel-group trial. Diabetes Care 40(2):201–209
Suzuki K, Mitsuma Y, Sato T, Anraku T, Hatta M (2016) Comparison of combined tofogliflozin and glargine, tofogliflozin added to insulin, and insulin dose-increase therapy in uncontrolled type 2 diabetes. J Clin Med Res 8(11):805–814
Takashima H, Yoshida Y, Nagura C et al (2018) Renoprotective effects of canagliflozin, a sodium glucose cotransporter 2 inhibitor, in type 2 diabetes patients with chronic kidney disease: a randomized open-label prospective trial. Diab Vasc Dis Res 15(5):469–472
Terra SG, Focht K, Davies M et al (2017) Phase III, efficacy and safety study of ertugliflozin monotherapy in people with type 2 diabetes mellitus inadequately controlled with diet and exercise alone. Diabetes Obes Metab 19(5):721–728
Wanner C, Inzucchi SE, Lachin JM et al (2016) Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 375(4):323–334
Wilding JP, Charpentier G, Hollander P et al (2013) Efficacy and safety of canagliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin and sulphonylurea: a randomised trial. Int J Clin Pract 67(12):1267–1282
Wiviott SD, Raz I, Bonaca MP et al (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380(4):347–357
Yang W, Ma J, Li Y et al (2018) Dapagliflozin as add-on therapy in Asian patients with type 2 diabetes inadequately controlled on insulin with or without oral antihyperglycemic drugs: a randomized controlled trial. J Diabetes 10(7):589–599
Acknowledgements
We would like to thank the Research Unit from the School of Medicine of the Universidad Autonoma de Nuevo Leon, Monterrey, Mexico and the Knowledge and Evaluation Research (KER) Unit from the Mayo Clinic, Rochester, MN for their support and guidance in the conduct of this systematic review.
Funding
No grant, funding source, or any other kind of financial support was received for the elaboration of this study.
Author information
Authors and Affiliations
Contributions
EGD-T, ADG-C, and RR-G conceived the idea of the study. NA-V and AMF performed the search strategy. EGD-T, BMC-G, FJB-F, VG-N, ADG-C, and GR-T screened potentially eligible articles. EGD-T, BMC-G, and VG-N extracted the data and rated the quality of the evidence. EGDT and NA-V analyzed the data. EGD-T wrote the first manuscript with input of RR-G. RR-G, VMM, and JGG-G critically reviewed, revised, and provided significant contribution to the manuscript. All authors agreed on the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare having no conflicts of interests or financial disclosures.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
The study does not require an informed consent as no participants were recruited.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dorsey-Treviño, E.G., González-González, J.G., Alvarez-Villalobos, N. et al. Sodium-glucose cotransporter 2 (SGLT-2) inhibitors and microvascular outcomes in patients with type 2 diabetes: systematic review and meta-analysis. J Endocrinol Invest 43, 289–304 (2020). https://doi.org/10.1007/s40618-019-01103-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-019-01103-9