Abstract
Pituitary apoplexy is a rare endocrine emergency that occurs in a small number of patients with a pituitary tumor. It is a clinical syndrome characterized by the sudden onset of headache, nausea, vomiting, visual impairment, and decreased consciousness, caused by hemorrhage and/or infarction of the pituitary gland. Pituitary apoplexy has very rarely been described during pregnancy, when it is potentially life-threatening to both the mother and the fetus, if unrecognized. Only a few cases have been published to date. The review of the existing literature underlines that pituitary apoplexy, although rare, should be borne in mind when a pregnant woman presents with severe headache and visual defects of sudden onset. After initial management, which includes intravenous glucocorticoid therapy, fluid and electrolyte replacement, the final selection of medical or surgical treatment should result from a multidisciplinary approach involving expert specialists, keeping into account both severity of clinical presentation and gestational week.

Similar content being viewed by others
References
Bailey P (1898) Pathological report of a case of acromegaly, with special reference to the lesions in the hypophysis cerebri and in the thyroid gland; and a case of hemorrhage into the pituitary. Phila Med J 1:789–792
Wakai S, Fukushima T, Teramoto A, Sano K (1981) Pituitary apoplexy: its incidence and clinical significance. J Neurosurg 55:187–193
Nawar RN, Abdel-Mannan D, Selma WR, Arafah BM (2008) Pituitary tumor apoplexy: a review. J Intensive Care Med 23:75–90
Bills DC, Meyer FB, Laws ER Jr et al (1993) A retrospective analysis of pituitary apoplexy. Neurosurgery 33:602–609
Randeva HS, Schoebel J, Byrne J, Esiri M, Adams CB, Wass JA (1999) Classical pituitary apoplexy: clinical features, management and outcome. Clin Endocrinol 51:181–188
Biousse V, Newman NJ, Oyesiku NM (2001) Precipitating factors in pituitary apoplexy. J Neurol Neurosurg Psychiatry 71:542–545
Rajasekaran S, Vanderpump M, Baldeweg S et al (2011) UK guidelines for the management of pituitary apoplexy. Pituitary apoplexy guidelines development group: may 2010. Clin Endocrinol 74:9–20
Karaka Z, Tanriverdi F, Unluhizarci K, Kelestimur E (2010) Pregnancy and pituitary disorders. Eur J Endocrinol 162:453–475
Motivala S, Gologorsky Y, Kostandinov J, Post KD (2011) Pituitary disorders during pregnancy. Endocrinol Metab Clin North Am 40:827–836
Elster AD, Sanders TG, Vines FS, Chen MY (1991) Size and shape of pituitary gland during pregnancy and post-partum: measurement with MR imaging. Radiology 191:531–535
Gonzales JG, Elizondo G, Saldivar D, Nanez H, Todd LE, Villareal JZ (1988) Pituitary gland growth during normal pregnancy: an in vivo study using magnetic resonance imaging. Am J Med 85:217–220
Dinc H, Esen F, Demirci A, Sari A, Resit GH (1998) Pituitary dimensions and volume measurements in pregnancy and post-partum MR assessment. Acta Radiol 39:64–69
Tiboldi T, Nemessanyi Z, Csernay I, Kovacs K (1967) Effect of oestrogens on pituitary blood flow in rats. Endocrinol Exp 1:73–77
Buster JE, Abrahm GE (1975) The hormonal applications of steroid hormone radioimmunoassay to clinical obstetrics. Obstet Gynecol 46:489–499
Casanueva FF, Molitch ME, Schlechte JA et al (2006) Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol 65:265–273
Maurer RA (1982) Relationship between estradiol, ergocryptine, and thyroid hormone: effects on prolactin synthesis and prolactin messenger ribonucleic acid levels. Endocrinology 110:1515–1520
de Heide LJM, van Tol KM, Doorenbos B (2004) Pituitary apoplexy presenting during pregnancy. Neth J Med 62:39–396
Molitch ME (2011) Prolactinoma in pregnancy. Best Pract Res Clin Endocrinol Metab 25:885–896
Pichon MF, Bression D, Peillon F, Milgrom E (1980) Estrogen receptors in human pituitary adenoma. J Clin Endocrinol Metab 51:897–902
Lamberts SW, Klijn JG, de Lange SA, Singh R, Stefanko SZ, Birkenhäger JC (1979) The incidence of complications during pregnancy after treatment of hyperprolactinemia with bromocriptine in patients with radiologically evident pituitary tumors. Fertil Steril 31:614–619
O’Donovan PA, O’Donovan PJ, Ritchie EH, Feely M, Jenkins DM (1986) Apoplexy into a prolactin secreting macroadenoma during early pregnancy with successful outcome: case report. Br J Obstet Gynaecol 93:389–391
Onesti ST, Wisniewski TH, Post KD (1990) Clinical versus subclinical pituitary apoplexy: presentation, surgical management and outcome in 21 patients. Neurosurgery 26:980–986
Lunardi P, Rizzo A, Missori P, Fraioli B (1991) Pituitary apoplexy in an acromegalic woman operated on during pregnancy by transsphenoidal approach. Int J Gynaecol Obstet 34:71–74
Ohtsubo T, Asakura T, Kadota K et al (1991) A report of a transsphenoidal operation during pregnancy for a pituitary adenoma. No Shinkei Geka 19:867–870
Freeman R, Wezenter B, Silverstein M et al (1992) Pregnancy-associated subacute hemorrhage into a prolactinoma resulting in diabetes insipidus. Fertil Steril 58:427–429
Gondim J, Ramos Júnior F, Pinheiro I, Schops M, Tella Júnior OI (2003) Minimal invasive pituitary surgery in a hemorrhagic necrosis of an adenoma during pregnancy. Minim Invasive Neurosurg 46:173–176
Okafor UV, Onwuekwe IO, Ezegwui HU (2009) Management of pituitary adenoma with mass effect in pregnancy: a case report. Cases J 2:9117
Parihar V, Yadav YR, Sharma D (2009) Ann Indian Acad Neurol 12:54–55
Ginath S, Golan A (2010) Images in clinical medicine. Gestational pituitary-tumor apoplexy. N Engl J Med 12(363):e10
Rosen SG, Kharlip J. Pituitary apoplexy during pregnancy. Endocr Rev 2011, 32 (03_meetingAbstracts): P1-438
Couture N, Aris-Jilwan N, Serri O (2012) Apoplexy of a microprolactinoma during pregnancy: case report and review of literature. Endocr Pract 18:e147–e150
Janssen NM, Dreyer K, van der Weiden RMF (2012) Management of pituitary tumour apoplexy with bromocriptine in pregnancy. J R Soc Med Sh Rep 3:43
Witek P, Zieliński G, Maksymowicz M, Zgliczyński W (2012) Transsphenoidal surgery for a life-threatening prolactinoma apoplexy during pregnancy. Neuro Endocrinol Lett 33:483–488
Kita D, Hayashi Y, Sano H et al (2012) Postoperative diabetes insipidus associated with pituitary apoplexy during pregnancy. Neuro Endocrinol Lett 33:107–112
Kannuki S, Bando K, Shirakawa N et al (1993) MRI findings and endocrinological dysfunction in hemorrhagic pituitary adenoma. No Shinkei Geka 21:1005–1012
Schrupp Berg HL, Edlow JA (2007) Post-partum pituitary apoplexy: a case report. Intern Emerg Med 2:311–314
Krull I, Emanuel C, Philipp KC, Christoph G, Rahel S (2010) Hyponatremia associated come due to pituitary apoplexy in early pregnancy: a case report. Gynecol Endocrinol 26:197–200
Chng E, Tar Khor H. Pituitary apoplexy in a healthy pituitary gland in pregnancy: case report and literature review. Endocr Rev 2013, 34 (03_meetingAbstracts), SUN-192
Mathur D, Lim LF, Mathur M, Sng BL (2014) Pituitary apoplexy with reversible cerebral vasoconstrictive syndrome after spinal anaesthesia for emergency caesarean section: an uncommon cause for postpartum headache. Anaesth Intensive Care 42:99–105
Zayour DH, Selman WR, Arafah BM (2004) Extreme elevation of intrasellar pressure in patients with pituitary tumor apoplexy: relation to pituitary function. J Clin Endocrinol Metab 89:5649–5654
Ranabir S, Baruah MP (2011) Pituitary apoplexy. Ind J Endocrinol Metab 15:S188–S196
Sibal L, Ball SG, Connolly V et al (2004) Pituitary apoplexy: a review of clinical presentation, management and outcome in 45 cases. Pituitary 7:157–163
Ayuk J, McGregor EJ, Mitchell RD, Gittoes NJ (2004) Acute management of pituitary apoplexy - surgery or conservative management? Clin Endocrinol (Oxf) 61:747–752
Lee J-S, Park Y-S, Kwon J-T, Nam T-K, Lee T-J, Kim J-K (2011) Radiological apoplexy and its correlation with acute clinical presentation, angiogenesis and tumor microvascular density in pituitary adenomas. J Korean Neurosurg Soc 50:281–287
Expert Panel on MR safety, Kanal E, Barkovich AJ, Bell C et al (2013) ACR Guidance Document on MR safe practice. J Magn Reson Imaging 37:510–530
Webb JAW, Thomsen HS (2013) Gadolinium contrast media during pregnancy and lactation. Acta Radiol 54:599–600
Murad-Kejbou S, Eggenberger E (2009) Pituitary apoplexy: evolution, management and prognosis. Curr Opin Ophthalmol 20:456–461
Stalldecker G, Mallea-Gil MS, Guitelman M et al (2010) Effect of cabergoline on pregnancy and embryo-fetal development: retrospective study on 103 pregnancies and a review of the literature. Pituitary 13:345–350
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
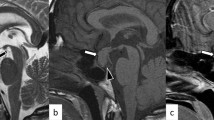
Additional case report: A 27-year-old Caucasian woman with no history of pituitary adenoma was admitted at the 35th week of her first pregnancy because of severe fronto-orbital headache, photophobia, and blurring of vision of sudden onset. Neuroophthalmological examination showed deterioration of visual acuity (5/10 in right eye, 2/10 in left eye), with a generalized and bilateral visual field defect compatible with compression of the optic chiasm, evolving in bilateral narrowing of sight within few hours. MRI revealed an intra- and extrasellar mass, with suprasellar extension and compression of the optic chiasm, deviation of the pituitary stalk, and fluid levels at T1-weighted image consistent with recent bleeding (Fig. 1). Neurosurgery was postponed after delivery, and an urgent cesarean section was performed; Delivery was uneventful, and a healthy son of 3350 g was born. The day after delivery, the pituitary lesion was successfully removed via endonasal endoscopic transsphenoidal surgery. Histologically hemorrhagic material and necrotic changes were shown, compatible with the diagnosis of pituitary adenoma apoplexy. In the next few days, there was a marked improvement of visual field and visual disturbances. Laboratory testing after surgery showed central hypothyroidism and mild hyperprolactinemia. A repeat MRI after 4 months showed total removal of the adenoma, no tumor regrowth, and persistence of pituitary stalk deviation (Fig. 1). Nine months after surgery, hormonal reassessment revealed a normal cortisol secretive response, allowing glucocorticoid withdrawal, confirmed central hypothyroidism requiring replacement therapy, and a normal GH response; because the patient had central hypogonadism due to persistent hyperprolactinemia, cabergoline therapy was started, with restoration of normal prolactin concentration and regular menstrual periods.
Rights and permissions
About this article
Cite this article
Piantanida, E., Gallo, D., Lombardi, V. et al. Pituitary apoplexy during pregnancy: a rare, but dangerous headache. J Endocrinol Invest 37, 789–797 (2014). https://doi.org/10.1007/s40618-014-0095-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-014-0095-4