Abstract
Background
The occurrence of outdoor activity limitation (OAL) among older adults is influenced by multidimensional and confounding factors associated with aging.
Aim
The aim of this study was to apply interpretable machine learning (ML) to develop models for multidimensional aging constraints on OAL and identify the most predictive constraints and dimensions across multidimensional aging data.
Methods
This study involved 6794 community-dwelling participants older than 65 from the National Health and Aging Trends Study (NHATS). Predictors included related to six dimensions: sociodemographics, health condition, physical capacity, neurological manifestation, daily living habits and abilities, and environmental conditions. Multidimensional interpretable machine learning models were assembled for model construction and analysis.
Results
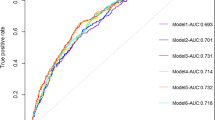
The multidimensional model demonstrated the best predictive performance (AUC: 0.918) compared to the six sub-dimensional models. Among the six dimensions, physical capacity had the most remarkable prediction (AUC: physical capacity: 0.895, daily habits and abilities: 0.828, physical health: 0.826, neurological performance: 0.789, sociodemographic: 0.773, and environment condition: 0.623). The top-ranked predictors were SPPB score, lifting ability, leg strength, free kneeling, laundry mode, self-rated health, age, attitude toward outdoor recreation, standing time on one foot with eyes open, and fear of falling.
Discussion
Reversible and variable factors, which are higher in the set of high-contribution constraints, should be prioritized as the main contributing group in terms of interventions.
Conclusion
The integration of potentially reversible factors, such as neurological performance in addition to physical function into ML models, yields a more accurate assessment of OAL risk, which provides insights for targeted, sequential interventions for older adults with OAL.



Similar content being viewed by others
Data availability
The NHATS dataset can be obtained from www.nhats.org.
References
Simonsick EM, Guralnik JM, Volpato S et al (2005) Just get out the door! Importance of walking outside the home for maintaining mobility: findings from the women’s health and aging study. J Am Geriatr Soc 53:198–203. https://doi.org/10.1111/j.1532-5415.2005.53103.x
Choi NG, DiNitto DM, Marti CN (2022) Older adults’ frequency of going outside during the COVID-19 pandemic: associations with physical distancing, health status, and fall risk factors. J Appl Gerontol. https://doi.org/10.1177/07334648221134178
Nordbakke STD (2019) Mobility, out-of-home activity participation and needs fulfilment in later life. Int J Environ Res Public Health 16:5109. https://doi.org/10.3390/ijerph16245109
Geohagen O, Hamer L, Lowton A et al (2022) The effectiveness of rehabilitation interventions including outdoor mobility on older adults’ physical activity, endurance, outdoor mobility and falls-related self-efficacy: systematic review and meta-analysis. Age Ageing 51:afac120. https://doi.org/10.1093/ageing/afac120
Qin W, Wang Y, Cho S (2021) Neighborhood social cohesion, physical disorder, and daily activity limitations among community-dwelling older adults. Arch Gerontol Geriatr 93:104295. https://doi.org/10.1016/j.archger.2020.104295
Paterson DH, Warburton DER (2010) Physical activity and functional limitations in older adults: a systematic review related to Canada’s Physical Activity Guidelines. Int J Behav Nutr Phys Act 7:1–22. https://doi.org/10.1186/1479-5868-7-38
Sakari-Rantala R, Era P, Rantanen T et al (1998) Associations of sensory-motor functions with poor mobility in 75-and 80-year-old people. Scand J Rehabil Med 30:121–127. https://doi.org/10.1080/003655098444237
Cruz-Almeida Y, Rosso A, Marcum Z et al (2017) Associations of musculoskeletal pain with mobility in older adults: potential cerebral mechanisms. J Gerontol Ser A: Biomed Sci Med Sci 72:1270–1276. https://doi.org/10.1093/gerona/glx084
Kerr J, Sallis JF, Saelens BE et al (2012) Outdoor physical activity and self rated health in older adults living in two regions of the US. Int J Behav Nutr Phys Act 9:1–4. https://doi.org/10.1186/1479-5868-9-89
Aartsen MJ, Smits CHM, Van Tilburg T et al (2002) Activity in older adults: cause or consequence of cognitive functioning? A longitudinal study on everyday activities and cognitive performance in older adults. J Gerontol B Psychol Sci Soc Sci 57:P153–P162. https://doi.org/10.1093/geronb/57.2.P153
Rantakokko M, Iwarsson S, Vahaluoto S et al (2014) Perceived environmental barriers to outdoor mobility and feelings of loneliness among community-dwelling older people. J Gerontol Ser A: Biomed Sci Med Sci 69:1562–1568. https://doi.org/10.1093/gerona/glu069
Choi NG, Kim J, DiNitto DM et al (2015) Perceived social cohesion, frequency of going out, and depressive symptoms in older adults: examination of longitudinal relationships. Gerontol Geriatr Med 1:2333721415615478. https://doi.org/10.1177/2333721415615478
Blankevoort CG, Van Heuvelen MJG, Boersma F et al (2010) Review of effects of physical activity on strength, balance, mobility and ADL performance in elderly subjects with dementia. Dement Geriatr Cogn Disord 30:392–402. https://doi.org/10.1159/000321357
Yu Y, Chen Z, Bu J et al (2020) Do stairs inhibit seniors who live on upper floors from going out? HERD Health Environ Res Des J 13:128–143. https://doi.org/10.1177/1937586720936588
Tsai LT, Rantakokko M, Portegijs E et al (2013) Environmental mobility barriers and walking for errands among older people who live alone vs with others. BMC Public Health 13:1–8. https://doi.org/10.1186/1471-2458-13-1054
Portegijs E, Keskinen KE, Tsai LT et al (2017) Physical limitations, walkability, perceived environmental facilitators and physical activity of older adults in Finland. Int J Environ Res Public Health 14:333. https://doi.org/10.3390/ijerph14030333
Biswas A, Oh PI, Faulkner GE et al (2015) Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med 162:123–132. https://doi.org/10.7326/M14-1651
Isaac V, Stewart R, Artero S et al (2009) Social activity and improvement in depressive symptoms in older people: a prospective community cohort study. Am J Geriatr Psychiatry 17:688–696. https://doi.org/10.1097/JGP.0b013e3181a88441
Grammatikopoulos I, Koutentakis C (2010) Social activity and participation as determinants of anxiety and depression among elderly in primary care. Ann Gen Psychiatry 9 (Suppl 1):S137. https://doi.org/10.1186/1744-859X-9-S1-S137
Satariano WA, Haight TJ, Tager IB (2000) Reasons given by older people for limitation or avoidance of leisure time physical activity. J Am Geriatr Soc 48:505–512. https://doi.org/10.1111/j.1532-5415.2000.tb04996.x
Murdoch WJ, Singh C, Kumbier K et al (2019) Definitions, methods, and applications in interpretable machine learning. Proc Natl Acad Sci 116:22071–22080. https://doi.org/10.1073/pnas.1900654116
Freedman VA, Kasper JD (2019) Cohort profile: the National Health and Aging Trends Study (NHATS). Int J Epidemiol 48:1044–1045. https://doi.org/10.1093/ije/dyz109
Sugiyama T, Thompson CW (2007) Outdoor environments, activity and the well-being of older people: conceptualising environmental support. Environ Plan A 39:1943–1960. https://doi.org/10.1068/a38226
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186. https://doi.org/10.1097/00006199-197005000-00029
Guralnik JM, Simonsick EM, Ferrucci L et al (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85–M94. https://doi.org/10.1093/geronj/49.2.m85
Freedman M, Leach L, Kaplan E et al. (1994) Clock drawing: a neuropsychological analysis. Oxford University Press, USA. Retrieved from: https://psycnet.apa.org/record/1994-98032-000
Thapa R, Garikipati A, Shokouhi S et al (2022) Predicting falls in long-term care facilities: machine learning study. JMIR Aging. 5:e35373. https://doi.org/10.2196/35373
Qiu S, Miller MI, Joshi PS et al (2022) Multimodal deep learning for Alzheimer’s disease dementia assessment. Nat Commun 13:3404. https://doi.org/10.1038/s41467-022-31037-5
Liu X, Dumontier C, Hu P et al (2022) Clinically interpretable machine learning models for early prediction of mortality in older patients with multiple organ dysfunction syndrome (MODS): an international multicenter retrospective study. J Gerontol A Biol Sci Med Sci. https://doi.org/10.1093/gerona/glac107
Khera R, Haimovich J, Hurley NC et al (2021) Use of machine learning models to predict death after acute myocardial infarction. JAMA Cardiol 6:633–641. https://doi.org/10.1001/jamacardio.2021.0122
Speiser JL, Callahan KE, Houston DK et al (2021) Machine learning in aging: an example of developing prediction models for serious fall injury in older adults. J Gerontol A Biol Sci Med Sci 76:647–654. https://doi.org/10.1093/gerona/glaa138
Iwarsson S, Ståhl A, Löfqvist C et al. (2013) Mobility in outdoor environments in old age. Environmental gerontology: making meaningful places in old age, pp 175–198. Retrieved from: https://psycnet.apa.org/record/2013-07285-008
Shimada H, Ishizaki T, Kato M et al (2010) How often and how far do frail elderly people need to go outdoors to maintain functional capacity? Arch Gerontol Geriatr 50:140–146. https://doi.org/10.1016/j.archger.2009.02.015
Vasunilashorn S, Coppin AK, Patel KV et al (2009) Use of the short physical performance battery score to predict loss of ability to walk 400 meters: analysis from the InCHIANTI study. J Gerontol Ser A: Biomed Sci Med Sci 64:223–229. https://doi.org/10.1093/gerona/gln022
Turunen K, Salpakoski A, Edgren J et al (2017) Physical activity after a hip fracture: effect of a multicomponent home-based rehabilitation program—a secondary analysis of a randomized controlled trial. Arch Phys Med Rehabil 98:981–988. https://doi.org/10.1016/j.apmr.2017.01.004
Portegijs E, Rantakokko M, Mikkola TM et al (2014) Association between physical performance and sense of autonomy in outdoor activities and life-space mobility in community-dwelling older people. J Am Geriatr Soc 62:615–621. https://doi.org/10.1111/jgs.12763
Muir SW, Gopaul K, Montero Odasso MM (2012) The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age Ageing 41:299–308. https://doi.org/10.1093/ageing/afs012
Lachman ME, Howland J, Tennstedt S et al (1998) Fear of falling and activity restriction: the survey of activities and fear of falling in the elderly (SAFE). J Gerontol B Psychol Sci Soc Sci 53:P43–P50. https://doi.org/10.1093/geronb/53b.1.p43
Arfken CL, Lach HW, Birge SJ et al (1994) The prevalence and correlates of fear of falling in elderly persons living in the community. Am J Public Health 84:565–570. https://doi.org/10.2105/ajph.84.4.565
Tennstedt S, Howland J, Lachman M et al (1998) A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol B Psychol Sci Soc Sci 53:P384–P392. https://doi.org/10.1093/geronb/53b.6.p384
Zijlstra GAR, Van Haastregt JCM, Van Eijk JTM et al (2007) Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing 36:304–309. https://doi.org/10.1093/ageing/afm021
Gillick MR, Serrell NA, Gillick LS (1982) Adverse consequences of hospitalization in the elderly. Soc Sci Med 16:1033–1038. https://doi.org/10.1016/0277-9536(82)90175-7
Arieli M, Kizony R, Gil E et al (2022) Participation in daily activities after acute illness hospitalization among high-functioning older adults: a qualitative study. J Clin Nurs. https://doi.org/10.1111/jocn.16418
Pérès K, Matharan F, Daien V et al (2017) Visual loss and subsequent activity limitations in the elderly: the French three-city cohort. Am J Public Health 107:564–569. https://doi.org/10.2105/AJPH.2016.303631
Mangione CM, Phillips RS, Seddon JM et al (1992) Development of the “Activities of Daily Vision Scale”: a measure of visual functional status. Med Care. https://doi.org/10.1097/00005650-199212000-00004
Cai Y, Schrack JA, Wang H et al (2021) Visual impairment and objectively measured physical activity in middle-aged and older adults. J Gerontol Ser A 76:2194–2203. https://doi.org/10.1093/gerona/glab103
Eisdorfer CE, Lawton M (1973) The psychology of adult development and aging https://doi.org/10.1037/10044-000
Rantakokko M, Iwarsson S, Kauppinen M et al (2010) Quality of life and barriers in the urban outdoor environment in old age. J Am Geriatr Soc 58:2154–2159. https://doi.org/10.1111/j.1532-5415.2010.03143.x
Cohen-Mansfield J, Shmotkin D, Hazan H (2012) Homebound older persons: prevalence, characteristics, and longitudinal predictors. Arch Gerontol Geriatr 54:55–60. https://doi.org/10.1016/j.archger.2011.02.016
Portegijs E, Rantakokko M, Viljanen A et al (2017) Perceived and objective entrance-related environmental barriers and daily out-of-home mobility in community-dwelling older people. Arch Gerontol Geriatr 69:69–76. https://doi.org/10.1016/j.archger.2016.11.011
Torku A, Chan APC, Yung EHK et al (2021) The influence of urban visuospatial configuration on older adults’ stress: a wearable physiological-perceived stress sensing and data mining based-approach. Build Environ 206:108298. https://doi.org/10.1016/j.buildenv.2021.108298
Cerin E, Lee K, Barnett A et al (2013) Objectively-measured neighborhood environments and leisure-time physical activity in Chinese urban elders. Prev Med 56:86–89. https://doi.org/10.1016/j.ypmed.2012.10.024
Yung EHK, Conejos S, Chan EHW (2016) Social needs of the elderly and active aging in public open spaces in urban renewal. Cities 52:114–122. https://doi.org/10.1016/j.cities.2015.11.022
Clarke PJ (2014) The role of the built environment and assistive devices for outdoor mobility in later life. J Gerontol Ser B: Psychol Sci Soc Sci 69:S8–S15. https://doi.org/10.1093/geronb/gbu121
Herbolsheimer F, Ungar N, Peter R (2018) Why is social isolation among older adults associated with depressive symptoms? The mediating role of out-of-home physical activity. Int J Behav Med 25:649–657. https://doi.org/10.1007/s12529-018-9752-x
Liu TW, Ng GYF, Chung RCK et al (2018) Cognitive behavioural therapy for fear of falling and balance among older people: a systematic review and meta-analysis. Age Ageing 47:520–527. https://doi.org/10.1093/ageing/afy010
Acknowledgements
The authors are grateful to the NHATS participants for their contribution of time and energy to the study.
Funding
This work was supported by the National Key Research and Development Program of China (Grant Nos. 2020YFC2008500 and 2020YFC2008502).
Author information
Authors and Affiliations
Contributions
LF and JZ planned and designed the study, interpreted the results, and drafted the initial version of the manuscript. FW and JZ conducted the data analysis and interpreted the results, and SL contributed to the preparation of the methods and results. This study was completed under the supervision of LT. All the authors have reviewed, edited, and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval and consent to participate
NHATS was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board. Informed consent was obtained from the NHATS participants. This study was exempt from an institutional ethical review because it involved a publicly available dataset.
Consent for publication
Written informed consent was obtained from all the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fan, L., Zhang, J., Wang, F. et al. Exploring outdoor activity limitation (OAL) factors among older adults using interpretable machine learning. Aging Clin Exp Res 35, 1955–1966 (2023). https://doi.org/10.1007/s40520-023-02461-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02461-4