Abstract
Background
Postoperative delirium (POD) is a major complication following a surgical procedure. There is evidence that improving knowledge about POD could enhance POD care and patient outcomes.
Aim
The study aimed to evaluate whether the amount of delirium education among registered nurses working in post-anaesthetics care units (PACU) impacts on their self-reported confidence and competence in recognising and managing delirium as well as prior knowledge on factors that influence the risk of delirium onset for older people.
Method
The current study utilised an online survey on delirium care practice among registered nurses in PACUs. The survey consisted of 27 items. There were questions about confidence and competence in delirium care, knowledge about delirium risk factors, and ranked responses to two case scenario questions to evaluate the application of POD care. There were also demographic questions, including previous experience with delirium care education.
Results
A total of 336 responses were generated from registered nurses working in PACU. Our findings found substantial variability among the respondents about their delirium care education. The amount of delirium education did not influence the PACU registered nurses’ confidence or competence in delirium care. In addition, previous education did not have an impact on their knowledge about delirium risk factors.
Discussion and conclusion
These findings suggested that the quantity of prior education about delirium did not improve the confidence, competence, knowledge, or case scenario questions of PACU registered nurses. Thus, delirium care education needs to be transformed to ensure it has a positive effect on delirium care clinical practice by registered nurses in PACU.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rapid increase in the global aging population emphasises the need for enhanced aged care. Globally, the estimated population of people 65 years and over is 727 million and the number is expected to double by the year 2050 [1]. As such, improved hospital care for older population groups, including delirium care which causes a significant health burden is warranted [2]. Delirium is an acute, reversible disorder of attention and cognition [3]. Delirium can occur during hospital admission and when it occurs after a surgical procedure it is known as postoperative delirium (POD). POD is more common among older people [2] and is one of the major complications experienced by older people following a surgical procedure. There are evidence-based clinical practice guidelines for delirium management, however, the routine practice of delirium diagnosis in clinical settings differ widely [4,5,6,7]. This discrepancy in diagnostic criteria leads to inadequate delirium recognition, subsequently resulting in under-detection of delirium incidence, [5, 8] especially among older individuals. There is a need for a uniform approach in clinical practice relating to delirium. Delirium education is most effective when formal teaching is interactive and engages leadership in combined clinical pathways and evidence-based assessment tools [9, 10]. Fundamentally, more structured education sessions that emphasise evidence-based practices in multimodal/multiphase and incorporating objective structured clinical examination (OSCE) style education can empower nurses to feel they can effectively manage delirium in the workplace as well as maintain their mental health and feel safe [10,11,12].
The impact of POD on older people cuts across all aspects of healthcare including prolonged length of stay in the hospital, falls, mortality and repeat delirium as well as increased medical expense, higher rates of readmission and/or relocation to a nursing home after discharge [6, 7, 13, 14]. An episode of POD also adds the risk of developing cognitive impairment in more than 50% of surgical patients and this risk persist for one-year post-surgery [15,16,17]. Improving delirium care is imperative to address the healthcare burden of delirium and improve post-operative outcomes for older people. One way of achieving this is undertaking research that supports knowledge translation of evidence-based delirium care with registered nurses. One group of registered nurses where there is great potential to improve the implementation of evidence-based delirium care is those working in PACUs as PACUs are critical care units with close observation and the first point of recovery for surgical patients.
Education is the first stage of knowledge translation, as such, it is imperative that the knowledge of clinicians is first established before undertaking knowledge translation research. This study was undertaken as a part of knowledge translation research evaluating the impact of an education intervention on registered nurses working in PACUs, specifically improved confidence and competence in delirium care as well as detecting delirium in PACUs. It is valuable to understand whether the amount of delirium education among registered nurses, whether it be undergraduate, postgraduate, and/ or ongoing professional development experience, impacts on delirium care confidence, competence, and knowledge about recognising and managing POD in older individuals [18, 19].
Our research group at have an established track record in undertaking knowledge translation in the area of delirium care [20, 21] using Pathmas’s 4A model of knowledge translation [22, 23]. The delirium care pathway developed by our research team progressed into becoming the Australian Commission on Safety and Quality in Health Care delirium care national standard [24]. Following the pathway publication, the research team implemented evidence-based delirium care with industry partners through knowledge translation research including local policy development and implementation of education programmes. However, the under-detection of delirium remains a problem [25]. Our research team explored in more depth the impact of education on the confidence, competence, and knowledge among registered nurses in recognising and managing delirium in older people. The team developed a survey aimed at assessing the relationship between the amount of delirium education undertaken and self-reported confidence and competence in delirium care as well as preferences on factors that influence the risk of delirium. Evidence from this study will describe the current levels of confidence and competence about delirium care as well as knowledge about delirium risk factors and management among PACU registered nurses in Australia. It is imperative that registered nurses working in PACU have the appropriate knowledge and skills to deliver evidence-based prevention, recognition, and management of post-surgical complications, including delirium [10, 26]. Once this is established, knowledge translation research can be designed that addresses the gaps in the delivery of evidence-based delirium care in PACU.
Methods
The study was approved by The University of Wollongong Social Sciences Human Research Ethics Committee (HREC) in compliance with the National Statement on Ethical Conduct in Human Research 2007 (HREC 2019/PID00838).
The current study utilised an online survey for data collection. This survey was constructed using SurveyMonkey® and distributed by email invitation to relevant nursing professional organisations in Australia. There was a total of 27 questions in the survey. Questions were adapted from similar surveys on the topic [27, 32] and were categorised into five groups:
-
demographics;
-
educational and professional background;
-
workplace practices and protocols in relation to delirium care in older people;
-
self-reported confidence and competence in recognising and managing delirium as well as prior knowledge on factors that influence the risk of delirium onset for older people; and
-
clinical case scenario-focused questions about POD (Table 1).
The questions about delirium education asked respondents to report on their undergraduate, postgraduate, and ongoing professional development experiences related to delirium. The scenario questions asked respondents to report how they would clinically respond to the delirium cases presented. Response formats to the questions were determined by the type of question asked and comprised of Likert scale items and fixed category responses.
Respondents self-reported their level of confidence and competence in four aspects of POD care:
-
(i)
recognising hyperactive delirium (characterised by increased motor activity, restlessness, agitation, aggression, wandering, hyper-alertness, hallucinations and delusions, and inappropriate behaviour);
-
(ii)
recognising hypoactive delirium (characterised by reduced motor activity, lethargy, withdrawal, drowsiness and staring into space);
-
(iii)
managing hyperactive delirium; and
-
(iv)
managing hypoactive delirium.
Confidence and competence levels were rated on a four-point Likert scale as ‘no confidence/competence,’ ‘slight confidence/competence,’ ‘moderate confidence/competence’ or ‘high confidence/competence.’
Validity and reliability of survey
Validity of the survey questions was undertaken in a range of ways. Content validity of the survey questions was reviewed by the whole research team as well as an independent panel consisting of seven researchers and clinicians with expertise in delirium care representing different multi-disciplinary team members comprising of an anaesthetist, a medical scientist, three nurses, a pharmacist, and a public health specialist. This review process was an iterative process with several rounds of comments sent back and forth. Edits and modifications, including deleting questions continued until they reached a consensus about the survey questions.
Following the content validity, face validity was completed with ten registered nurses working in a local PACU who accepted an invitation to participate in a face-to-face focus group to undertake a ‘read aloud’ activity with a member of the research team. During the ‘read aloud’ activity, the registered nurses provided feedback on the questions to ensure the intended meaning of each question was accurate. The feedback was incorporated to create the draft version of the survey.
Internal consistency testing of the survey questions was undertaken to determine the reliability of the survey. A draft version of the survey was pretested with 21 registered nurses working in a local PACU. Their responses were used solely for internal consistency testing and not included in the analysis for this study. The reliability of the survey questions was measured by checking using Cronbach’s Alpha whereby values above 0.7 are considered as acceptable [28]. The mean score for all survey questions in the current study instrument was 0.72. No further edits were made to the survey questions following the internal validity testing. The reliability of the survey was determined to be ‘acceptable’ and thus a definitive final version of the survey was ready for distribution.
Recruitment
The study population was defined as registered nurses in Australia who worked as preoperative nurses, certified registered nurse anaesthetists, post anaesthesia care unit (PACU) nurses or recovery nurses. A snowballing technique was adopted to recruit respondents from across Australia. The research team drew on their collaborations and contacted professional organisations (n = 4) and hospitals (n = 3) to facilitate the distribution of a survey email invitation. A survey email invitation was sent to primary contacts asking that the email invitation be forwarded to other potential respondents who were invited to also forward the survey email invitation. Calculating a response rate was not possible. However, we concluded that the survey sample was representative of the Australian registered nurse population by comparing the characteristics of the respondents with nurses registered with the Australian Health Practitioner Regulation Authority (AHPRA). According to the 2021 Health Workforce Data [29], 11.6% of registered nurses are male in Australia while we recruited 11.9% of male respondents for this survey. The number of registered nurses who reported that they worked in the major cities was also comparable (population 72.7% vs sample 69.6%). Registered nurses aged 34 and under accounted for 31.9% of the registered nursing population, compared to 35% in the survey sample.
Data analysis
Data were analysed using IBM SPSS Statistics for Windows, Version 21.0. (IBM Corp., Armonk, NY, USA). Frequencies and descriptive statistics for the demographic characteristics of the respondents were performed. Normality of continuous variables was assessed using Shapiro–Wilk tests. A one-way ANOVA (parametric) and Kruskal Wallis-H tests (non-parametric) were used to examine differences between groups for numeric data. Chi-square was used to determine the association between categorical variables about delirium care, such as confidence and competence in recognising and managing POD, knowledge about risk factors and clinical practice. Freidman test was used to analyse ranked data. All data were expressed as percentages or mean ± standard deviation (SD). Significance level was set at 5%.
Results
Respondent demographics
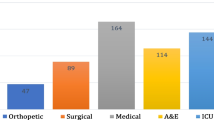
For the final analysis, a total of 336 respondents who answered the survey in part or completely were used. The study population was defined as registered nurses working in PACUs in Australia.
The survey respondents were categorised into three groups. These groups were based on the respondents’ answers to their delirium education during their undergraduate and postgraduate education as well as their ongoing professional development. The three groups are described thus:
-
(a)
Group 1: completed no formal delirium care education—undergraduate, postgraduate, nor ongoing professional development (n = 102);
-
(b)
Group 2: completed delirium care education from one or two of the described education categories—undergraduate, postgraduate, or ongoing professional development (n = 213); and
-
(c)
Group 3: completed delirium care education in all three or more education categories (n = 20).
These three groups were used to explore the association between the level of delirium training and the ability of nurses to recognise and manage delirium in older patients.
Demographic and clinical practice characteristics of respondents were reported as means (SD) and proportions (%) (Table 1). The mean age of respondents was 47 years (± 2 years). Most of the respondents were female (86%). There was a higher proportion of respondents who identified as registered nurses (RN) (45%), followed by clinical nurse specialists (CNS) (22%) and nurse unit managers (NUM) (14%). Approximately two-thirds of respondents reported that their highest qualification was a graduate diploma (35%), or bachelor’s degree (33%) and a low proportion had master's or PhD degrees (17%).
Respondent confidence and competence in the recognition and management of hyperactive and hypoactive delirium
Figure 1 shows the levels of confidence in recognising and managing hyperactive and hypoactive delirium across three levels of delirium education among the respondents. In the four aspects of delirium care, most respondents within the groups ranked themselves as slightly or moderately confident (65–80%), with no confidence or high confidence in the minority of responses (0–20%). Each of the three groups reported more confidence in recognising (hyper/hypoactive) delirium (Fig. 1A, B) than in managing hyper- or hypo-active delirium (Fig. 1C, D). There was a statistically significant relationship between levels of delirium education and confidence in recognising hyperactive delirium (\(\chi\)2 = 17.634, p = 0.024, Fig. 1A) between the respondents.
Figure 2 shows the pooled self-reported competence levels across these areas of delirium care education. Similar levels of confidence between the respondents, all groups identified the highest competence in recognising hyperactive delirium. There was a statistically significant association levels of delirium care education and their competence between the respondents in: (i) recognising hyperactive delirium (p = 0.048, Fig. 2A), and (ii) managing hyperactive delirium (p = 0.022 Fig. 2C).
Respondents were categorised into three groups based on their current positions (specialist nurse and above, unit manager, and registered nurse). No association was observed between position and the number of delirium training undertaken across the three groups (p = 0.273) or competence/confidence levels.
Respondent knowledge of risk factors
To determine the level of knowledge about delirium risk factors a list of 18 possible perioperative risk factors, identified from current literature, was presented to respondents. They were required to state whether each listed risk factor was either “new knowledge to me” or they were “already aware of this risk factor.” As shown in Fig. 5 respondents with no formal delirium care education (Group 1) had a mean score of 11.89 (± 3.81, range 0–18) out of the 18 listed risk factors. The group with one or two formal delirium care education (Group 2) scored a mean of 12.10 (± 3.26, range 3–18) and the group with three formal delirium care education had a mean score of 13.56 (± 3.43, range 8–18).
Respondent care of a patient with postoperative delirium—case scenario 1
Respondents were presented with the case scenario in Table 2. This case scenario represents a typical patient with hyperactive delirium. Two questions asked respondents about the management of the delirium care case scenario. The first question asked respondents to prioritise the listed actions in the order they would complete in the management of POD in an older person. The four available responses (in correct ascending order) were: (1) reassure and reorient the patient, (2) evaluate the current environment, (3) administer pain relief, and (4) administer sedation. Highest priority answers were ranked as 1, with the lowest priority answer ranked as 4. A Freidman test was used to analyse ranked data according to the three categories. This result was used to determine how each group prioritised the possible interventions given in the scenario. Participants’ ranked responses are presented in Table 3.
In the second delirium care case scenario question, respondents were asked to rank management options based on a scenario where the older person’ POD persisted for more than one hour. The four options provided were: (1) Request urgent medical review, (2) Request to administer antipsychotics, (3) Request to increase the level of sedation, and (4) Apply restraints to the patient. Participants’ ranked responses are presented in Table 4.
Discussion
Overview
Findings from this study showed an association between increased delirium education and self-reported confidence and competence in recognising and managing hyperactive delirium among registered nurses. Current evidence shows that targeted educational interventions are successful in knowledge translation in clinical practice relating to delirium among registered nurses [30]. The impact of delirium education on clinical care knowledge for hospitalised people is inconsistent [12, 31], with nurses’ recognition of delirium ranging between 26 and 83% [32]. One meta-analysis found that educational intervention was independently effective in promoting clinicians’ adherence to guidelines [33]. This highlights the need for a consensus on guidelines and continuing professional development education about the recognition and management of delirium. It is important to highlight that the big variability in the study data may have accounted for non-significant results in some of the tests utilised.
Respondents’ confidence and competence
Respondents in this study reported lower familiarity with hypoactive delirium. This observation provides insight into clinical practices and knowledge surrounding the recognition and management of delirium, specifically hypoactive delirium. Previous studies reported that a lack of knowledge and education reduced clinical confidence [34, 35]. One way to extend learning opportunities on specialist clinical topics like delirium care is to supplement these with workplace learning and peer support to improve the confidence and competence of nurses in areas where formal education is lacking [36, 37]. Registered nurses with higher levels of delirium education were significantly more likely to report higher confidence levels in recognising hyperactive or ‘typical’ delirium (p = 0.024). The presentation of hyperactive delirium is usually obvious, including agitation, hyper-arousal, loss of orientation, and language disturbance. Furthermore, the onset of hyperactive delirium presents challenges relating to physical and psychological exhaustion for nursing staff [38] with subsequent workplace education and support pertinent to staff competence and confidence. On the contrary, the more subtle nature of hypoactive delirium compared to the overt presentation of hyperactive delirium is a plausible explanation for this difference in confidence in recognising delirium subtypes [3, 39, 40]. Similarly, self-perception of competence in recognising hyperactive delirium among registered nurses was significantly associated with increased delirium care education. This result supports findings in the literature that competence is a process of knowledge and confidence [40,41,42]. Experience also contributes crucially to developing a sense of competence in the delivery of effective clinical care [42]. Considering the observed frequency of hypoactive delirium is substantially smaller compared to hyperactive delirium [3, 39, 40], registered nurses might perceive themselves less competent in the care of hypoactive delirium simply because of a lack of exposure to this sub-type of delirium.
Case scenario and interventions
A recent systematic review [43] found that while nurses do maintain an in-depth theoretical knowledge of delirium, this knowledge does not always translate to adequate prevention, recognition, and management of delirium. Non-pharmacological treatments are the most effective evidence-based management for POD [44], however, results from this study showed that, on average, pharmacologic interventions were the top two priorities for participants. Additionally, nurses may be following cues learned from peers that do not follow evidence-based guidelines, as nurses commonly learn from peer practice to supplement areas where they are lacking in knowledge [34, 45]. A 2017 study of the experiences and perceptions of care nurses found they were sceptical about assessment tools, distrusted management protocols and found that the unpleasant nature of delirium was a pervasive belief held by nurses. These negative beliefs were said to impact practice and decision making [46]. Conversely, peer collaboration may be a preferred way of learning among nurses because it creates more supportive workplaces. This was especially true when speaking about patients with delirium who were described as patients who caused stress and were taxing [34]. The unpredictable nature of delirium can create concerns for safety, and this is one of Thomas et al.’s (2021) four themes that were described as influencing the nursing care of patients with delirium [45]. However, it is also possible that knowledge of evidence-based delirium care is lacking, and nurses are unaware of the correct management protocols. Clear delirium management protocols must be developed and implemented in PACU, and complimentary education sessions provided when new protocols are introduced to reinforce evidence-based delirium care.
Strengths and limitation
Strengths in this study are seen in a large sample size of varied clinical experience and educational backgrounds. To replicate the current study, the survey would need to be adapted to other clinical settings or countries. Similar to how the survey was developed (from a Swedish study [27]), the scenario questions would need to be edited and amended to reflect clinical practice in different settings.
There is a possibility that the type of training received as well as repetitive training exposure may impact competences. The current study assessed respondents’ quantity of delirium education without evaluation of the delirium education content or frequency of delirium trainings. This limits the study outcomes, however, future studies could analyse delirium education content as well as frequency to understand how this may contribute to clinical practice in relation to delirium. Additionally, survey distribution for this study was restricted to perioperative and registered nurses working in PACUs Australia. Therefore, limitations must be made to the widespread application of findings to other ward practices or non-POD such as delirium tremens or withdrawal delirium. Results should also be interpreted with caution when considering survey answers are subject to self-reporting bias and the voluntary sample could represent respondents more motivated to learn than the greater nursing population. Although some evidence for the validity of self-rated competences has been described [47], undertaking audits of clinical records and observation of clinical practice is a proven method to determine whether levels of self-efficacy match clinical practices [48].
Conclusion
This paper contributes to the understanding of the behaviours of registered nurses care for older patients with POD. Most registered nurses report themselves slightly moderately skilled at caring for patients with hyperactive or hypoactive delirium. Enhanced delirium education can improve some, but not all aspects of registered nurses’ confidence and perceived competence in delirium care. Prior education was an unreliable predictor of registered nurses’ behaviour in a clinical case scenario. Current directives to treat POD with non-pharmacological supportive means may be best for the patient outcomes but also create adverse outcomes for registered nurses’ stress level, confidence, as well as mental and physical health. Further research is needed to optimise the interplay of patient and professional outcomes. Focus should be given to how registered nurses cope with these challenges and how best to build their knowledge and confidence in caring for patients with POD. Future research could explore the geographical differences in this area. In addition, the expansion of multimodal, multiphase peer-support programs represents an acceptable strategy to improve safety, confidence, and competency in perioperative registered nurse practices.
Data availability
The authors declared data availability during submission. Due to ethics approval, there are restrictions and data sharing.
References
DESA U (2009) United Nations Department of Economic and Social Affairs/Population Division: world population prospects: the 2008 revision. Reference Source
Deiner S, Silverstein JH (2009) Postoperative delirium and cognitive dysfunction. BJA Br J Anaesth 103:i41–i46
Inouye SK (2006) Delirium in older persons. N Engl J Med 354:1157–1165
Guthrie PF, Rayborn S, Butcher HK (2018) Evidence-based practice guideline: delirium. J Gerontol Nurs 44:14–24
Koirala B, Hansen BR, Hosie A, Budhathoki C, Seal S, Beaman A, Davidson PM (2020) Delirium point prevalence studies in inpatient settings: a systematic review and meta‐analysis. J Clin Nurs 29:2083–2092
Aldecoa C, Bettelli G, Bilotta F et al (2017) European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol 34:192–214
Hughes CG, Boncyk CS, Culley DJ, Fleisher LA, Leung JM, McDonagh DL, Gan TJ, McEvoy MD, Miller TE; Perioperative Quality Initiative (POQI) 6 Workgroup (2020) American Society for enhanced recovery and perioperative quality initiative joint consensus statement on postoperative delirium prevention. Anesth Analg 130:1572–1590
Greer N, Rossom R, Anderson P, MacDonald R, Tacklind J, Rutks I, Wilt TJ (2011) Delirium: screening, prevention, and diagnosis—a systematic review of the evidence [Internet]. Department of Veterans Affairs (US), Washington (DC). Available from: https://www.ncbi.nlm.nih.gov/books/NBK82554/
Yanamadala M, Wieland D, Heflin MT (2013) Educational interventions to improve recognition of delirium: a systematic review. J Am Geriatr Soc 61:1983–1993
Lieow JL, Chen FS, Song G, Tang PS, Kowitlawakul Y, Mukhopadhyay A (2019) Effectiveness of an advanced practice nurse-led delirium education and training programme. Int Nurs Rev 66:506–513
Solberg LM, Campbell CS, Jones K, Vaughn I, Suryadevara U, Fernandez C, Shorr R (2021) Training hospital inpatient nursing to know (THINK) delirium: a nursing educational program. Geriatr Nurs 42:16–20
Bowen CM, Stanton M, Manno M (2012) Using diffusion of innovations theory to implement the confusion assessment method for the intensive care unit. J Nurs Care Qual 27:139–145
Caplan GA, Teodorczuk A, Streatfeild J, Agar MR (2020) The financial and social costs of delirium. Eur Geriatr Med 11:105–112
Pezzullo L, Streatfeild J, Hickson J, Teodorczuk A, Agar MR, Caplan GA (2019) Economic impact of delirium in Australia: a cost of illness study. BMJ Open 9:e027514
Bickel H, Gradinger R, Kochs E, Förstl H (2008) High risk of cognitive and functional decline after postoperative delirium. Dement Geriatr Cogn Disord 26:26–31
Saczynski JS, Marcantonio ER, Quach Let al (2012) Cognitive trajectories after postoperative delirium. N Engl J Med 367:30–39
Theuerkauf N, Guenther U, Putensen C (2012) Postoperative delirium in the PACU and intensive care unit. Trends Anaesth Crit Care 2:148–155
Akechi T, Ishiguro C, Okuyama T et al (2010) Delirium training program for nurses. Psychosomatics 51:106–111
Swan JT (2014) Decreasing inappropriate unable-to-assess ratings for the confusion assessment method for the intensive care unit. Am J Crit Care 23:60–69
Traynor V, Britten N, Burns P (2016) Developing the delirium care pathways. J Res Nurs 21:582–596
Traynor V, Britten N (2010) Delirium Care Pathways: final report for NSW Health and Health Care of Older Australian Standing Committee. University of Wollongong, Wollongong
Pathman DE, Konrad TR, Freed GL, Freeman VA, Koch GG (1996) The awareness-to-adherence model of the steps to clinical guideline compliance: the case of pediatric vaccine recommendations. Med Care 34:873–889
Mickan S, Burls A, Glasziou P (2011) Patterns of ‘leakage’ in the utilisation of clinical guidelines: a systematic review. Postgrad Med J 87:670–679
ACSQHC (2021) Delirium Clinical Care Standard. 2021 [cited 2022 28 Oct]; Available from: https://www.safetyandquality.gov.au/our-work/clinical-care-standards/delirium-clinical-care-standard
Casey P, Cross W, Mart MW et al (2019) Hospital discharge data under-reports delirium occurrence: results from a point prevalence survey of delirium in a major Australian health service. Intern Med J 49:338–344
Roh YS (2021) The training needs of Korean intensive care unit nurses regarding delirium. Intensive Crit Care Nurs 62:102954
Jildenstål PK, Rawal N, Hallén JL, Berggren L, Jakobsson JGet al (2014) Perioperative management in order to minimise postoperative delirium and postoperative cognitive dysfunction: results from a Swedish web-based survey. Ann Med Surg (Lond) 3:100–107
Taber KS (2018) The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ 48:1273–1296
Department of Health and Aged Care. National Health Workforce Dataset (NHWDS). 2022 [cited 2021; Available from: https://hwd.health.gov.au/datatool/
van Velthuijsen EL, Zwakhalen SMG, Warnier RMJ et al (2018) Can education improve clinical practice concerning delirium in older hospitalised patients? Results of a pre-test post-test study on an educational intervention for nursing staff. BMC Med Educ 18:59. https://doi.org/10.1186/s12909-018-1177-3
Baker ND, Taggart HM, Nivens A, Tillman P (2015) Delirium: why are nurses confused? Medsurg Nurs 24:15–22
Igwe EO, Traynor V, Rodgers S, Waite A, MacLullich A, Foo I (2021) A survey about postoperative delirium in older patients among nurses and anaesthetists: implications for future practice and policy. J Res Nurs 26:341–351
Pereira VC, Silva SN, Carvalho VKS, Zanghelini F, Barreto JOM (2022) Strategies for the implementation of clinical practice guidelines in public health: an overview of systematic reviews. Health Res Policy Syst 20:13. https://doi.org/10.1186/s12961-022-00815-4 doi:
Hosie A, Lobb E, Agar M, Davidson PM, Phillips J (2014) Identifying the barriers and enablers to palliative care nurses’ recognition and assessment of delirium symptoms: a qualitative study. J Pain Symptom Manag 48:815–830
Kjorven M, Rush K, Hole R (2011) A discursive exploration of the practices that shape and discipline nurses’ responses to postoperative delirium. Nurs Inq 18:325–335
Boot R (2012) Delirium: a review of the nurses role in the intensive care unit. Intensive Crit Care Nurs 28:185–189
Phillips LA (2013) Delirium in geriatric patients: identification and prevention. Medsurg Nurs 22:9
Teece A, Baker J, Smith H (2022) Understanding the decision-making of critical care nurses when restraining a patient with psychomotor agitation secondary to hyperactive delirium: a ‘Think Aloud’ study. J Clin Nurs 31:121–133
Godfrey M, Smith J, Green J, Cheater F, Inouye SK, Young JB (2013) Developing and implementing an integrated delirium prevention system of care: a theory driven, participatory research study. BMC Health Serv Res 13:341. https://doi.org/10.1186/1472-6963-13-341
Zenilman ME (2017) Delirium: an important postoperative complication. JAMA 317:77–78
Teixeira CR, Pereira MC, Kusumota L, Gaioso VP, Mello CL, Carvalho EC (2015) Evaluation of nursing students about learning with clinical simulation. Rev Bras Enferm 68:284–291, 311–319 (English, Portuguese) https://doi.org/10.1590/0034-7167.2015680218i
Dehmer JJ, Amos KD, Farrell TM, Meyer AA, Newton WP, Meyers MO (2013) Competence and confidence with basic procedural skills: the experience and opinions of fourth-year medical students at a single institution. Acad Med 88:682–687
Christensen M (2016) Nurses’ knowledge of delirium: a survey of theoretical knowing. Nurs NZ 7:11–18
Inouye SK, Westendorp RGJ, Saczynski JS (2014) Delirium in elderly people. Lancet 383:911–922
Thomas N, Coleman M, Terry D (2021) Nurses’ experience of caring for patients with delirium: systematic review and qualitative evidence synthesis. Nurs Rep 11:164–174
Zamoscik K, Godbold R, Freeman P (2017) Intensive care nurses’ experiences and perceptions of delirium and delirium care. Intensive Crit Care Nurs 40:94–100
Braun E, Woodley A, Richardson JTE, Leidner B et al (2012) Self-rated competences questionnaires from a design perspective. Educ Res Rev 7:1–18
Hysong SJ, Best RG, Pugh JA (2006) Audit and feedback and clinical practice guideline adherence: making feedback actionable. Implement Sci 1:9. https://doi.org/10.1186/1748-5908-1-9
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This study was funded by the Illawarra Health and Medical Research Institute (IHMRI) Clinical Translational Grant Scheme (2018).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The study was approved by The University of Wollongong Social Sciences Human Research Ethics Committee (HREC) in compliance with the National Statement on Ethical Conduct in Human Research 2007 (HREC 2019/PID00838). The procedures used in this study adhere to the tenets of the Declaration of Helsinki and informed consent was obtained from all individual participants included in the study.
Informed consent
Study respondents were provided with Participant Information Sheet (PIS) prior to completing the survey. Survey completion counted as consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ormonde, C., Igwe, E.O., Nealon, J. et al. Delirium education and post-anaesthetics care unit nurses’ knowledge on recognising and managing delirium in older patients. Aging Clin Exp Res 35, 995–1003 (2023). https://doi.org/10.1007/s40520-023-02390-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02390-2