Abstract
Background
Recorded and live online physical exercise (PE) interventions are known to provide health benefits. However, the effects of prioritizing the number of live or recorded sessions remain unclear.
Aims
To explore which recorded-live sessions ratio leads to the best implementation and benefits in older adults.
Methods
Forty-six community-dwelling adults (> 60y.o.) were randomized into two groups completing a 12-week online PE intervention. Each group had a different ratio of live-recorded online sessions as follows: Live-Recorded-Live sessions (LRL; n = 22) vs. Recorded-Live-Recorded sessions (RLR; n = 24).
Results
Drop-out rates did not reach significance (LRL:14% vs. RLR: 29%, p = 0.20), and adherence was similar (> 85%) between groups. Both groups reported similar levels of satisfaction (> 70%), enjoyment (> 75%), and perceived exertion (> 60%). Both groups increased physical health and functional capacities, with greater improvements in muscle power (LRL: LRL: + 35 ± 16.1% vs. RLR: + 7 ± 13.9%; p = 0.010) and endurance (LRL: + 34.7 ± 15.4 vs. RLR: + 27.0 ± 26.5, p < 0.001) in the LRL group.
Discussion
Both online PE intervention modalities were adapted to the participants’ capacities and led to a high level of enjoyment and retention. The greater physical improvements observed in the LRL group are likely due to the higher presence of the instructor compared to the RLR group. Indeed, participants received likely more feedback to appropriately adjust postures and movements, increasing the quality of the exercises.
Conclusion
When creating online PE interventions containing both recorded and live sessions, priority should be given to maximizing the number of live sessions and not the number of recorded sessions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A physically active lifestyle is essential for healthy aging. However, several external factors, such as lack of transportation, weather (i.e., heat waves), or pandemic restrictions, represent key barriers to physical exercise (PE) in older adults, which may lead to sedentary behavior (> 50%). However, online PE interventions, also referred to as web-based PE interventions or programs [1,2,3], have been used by health professionals to deliver PE programs, which may help older adults overcome these barriers. We recently observed that during the COVID-19 pandemic, a live, online, fully remote 12-week intervention (3x/week on Zoom© with a certified exercise instructor (kinesiologist)) led to lower participant drop-out rates and greater health improvements in physical performance, functional capacities, quality of life, perceived health and level, compared to a pre-recorded, online, self-guided, fully remote 12-week intervention in older adults [3]. These results were in line with previous studies [4,5,6].
However, the use of a live, online, fully remote intervention presents some limitations, which could affect its scalability. In a real-life setting, the live intervention requires the presence of a kinesiologist at each session and is therefore more expensive and logistically complex than a fully recorded intervention. Thus, to improve public health recommendations (and balance benefits and limitations), we investigated the use of a combined remote exercise modality that includes both live and recorded sessions to determine the ratio of each modality that would be most effective to improve health in older adults. Importantly, to the best of our knowledge, no previous study has investigated the feasibility, acceptability, and health benefits of implementing these combined modalities in older adults, especially during a COVID-19 lockdown where the population was confined to their homes.
The main objective of this study was to investigate the feasibility and acceptability of two web-based PE interventions combining live and pre-recorded online sessions and their efficacy on health parameters in inactive but non-frail community-dwelling older adults. The secondary objective was to compare the efficacy of these two interventions on physical health. Based on our previous study [3], we hypothesized that both combined modalities would be feasible, acceptable, and effective to improve physical health. Furthermore, we also hypothesized that the modality with the higher ratio of live training sessions would lead to a lower drop-out rate and greater improvements in physical functioning than the intervention with the higher ratio of recorded training sessions, which is in line with previous studies [3,4,5,6].
Methods
Design
This 12-week community-based feasibility randomized interventional trial was approved by the Centre de Recherche de l’Institut Universitaire de Gériatrie de Montréal (CRIUGM) ethics committee (CERVN 20–21-05), and all participants signed a consent form. Participants were screened remotely through a Zoom meeting and were included in the study if they: (a) were aged 60 years and over, (b) had an internet connection, a home digital device with a webcam and an e-mail address, (c) lived independently in the community, (d) were inactive (less than 7 500 steps per day and less than 150 min of exercise per week) based on the Rapid Assessment of Physical Activity questionnaire [7], (e) did not have a contraindication to practice PE, (f) did not use walking aids or were non-frail (based on the Study of Osteoporotic Fractures questionnaire)[8], and (g) were not diagnosed with neurological, cardiovascular, lung, or cognitive diseases/disorders (according to the Telephonic-Mini Mental State Examination)[9]. Participants were recruited through CRIUGM’s volunteer database between September and December 2020 (during the second COVID-19 lockdown).
Intervention and randomization
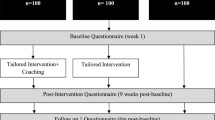
Face-to-face interventions were not possible in fall 2020 due to the second COVID-19 mandatory lockdown. To refine the exercise recommendation from our previous study performed during the first COVID-19 lockdown (for more detail see [3]), we implemented a 12-week intervention using online remote exercise sessions with a different combination of live and pre-recorded sessions. Given the uncertainty of the second lockdown duration in Quebec, participants were randomized using cluster method into: 1) a Live-Recorded-Live (LRL) group, in which participants had live exercise sessions with a kinesiologist on Mondays and Fridays on Zoom© and had a recorded session on Wednesdays on a dedicated website with an access code (www.trainingrecommend.com); or 2) a Recorded-Live-Recorded (RLR) group, where participants followed the same exercise sessions but with an inverse modality of delivery (recorded sessions on Mondays and Fridays and a Live session on Wednesdays) as presented in Fig. 1.
Briefly (for additional details see [3]), in order to ensure the safety of the online interventions, we created three difficulty levels (L1 = non-fit to L3 = fit) and stratified the randomization using a mobility decisional tree during the baseline assessment. Following randomization, participants followed three sessions per week (1 h/session) for 12 consecutive weeks. All training sessions were structured in three blocks of exercises designed to improve muscle function, cardiovascular capacity as well as flexibility. One session per week was predominantly focused on one of the three blocks of exercises. The intervention was identical to the intervention published in Granet et al. 2022 [3]. Full details of the intervention are available as a freely accessible supplementary material of the previously cited publication (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9384240/bin/glac127_suppl_supplementary_material.pdf). Briefly, each session was divided into 3 phases: 1) low-intensity global warm-up using 8 different exercises for a 10-min duration; 2) core of the session for a duration of 45 min and dispatched in circuits of 3 to 5 min of exercise, followed by 30 to 60 s of rest. The core of the session changed every session of the week. The first session of the week focused on balance and coordination. The second session focused on muscle function and cardiovascular capacity and the third session on flexibility (full details of each session are provided in [3]); 3) cool down and stretching period using 5 exercises focusing on the whole body for a duration of 5 min.
Additionally, all participants completed the same exercises and sessions, but the amplitude, position (sitting or standing), intensity, and number of repetitions were adapted during the live sessions according to their level and to allow an adequate progression. The intensity and difficulty of the sessions were adjusted every four weeks. Finally, all the training sessions were supervised by the same certified exercise instructor (certified kinesiologist).
Thus, among the participants recruited and randomized, two LRL groups (Group1 (L3): n = 14 [W: n = 10/ M: n = 4); Group 2 (L2): n = 8; (W: n = 7/ M: n = 1) and two RLR groups (Group1 (L3): n = 14 [W: n = 13/ M: n = 1); Group 2 (L2): n = 10; (W: n = 8/ M: n = 2) were trained.
Measures
Pre- and post-evaluations were conducted by the same assessor (certified kinesiologist), who was not involved in the intervention to limit bias.
Intervention feasibility and acceptability
We assessed feasibility using adherence to the intervention via the proportion of the 36 sessions attended. During the live sessions, adherence was noted by the kinesiologist, whereas for the recorded sessions, adherence was measured using the completion of an online questionnaire at the end of each session. As commonly recommended, participants were expected to complete 80% of the exercise sessions (29/36 sessions) for the study to be considered feasible [10]. Acceptability was also assessed throughout the intervention using five variables rated after each exercise training session via Limesurvey©. Participants rated the difficulty level of the proposed exercises, their overall satisfaction with the training session, perceived exertion, and enjoyment during the training session (for more detail see [3]). We also assessed the participants’ technological ability using three questions assessing: (1) whether they considered themselves technology savvy or not; 2) the number of years that they have used technological tools; and 3) the type of technology they have used (tablet, desktop computer/laptop, or smartphone).
Objective and subjective physical health measures
We briefly describe the tests and questionnaires used to assess functional capacities, physical performance, and physical health below (for more details see [3]).
A) Functional capacities
Short Physical Performance Battery (SPPB)
Based on the results of three tests, the SPPB score (x/12) is calculated using bipodal balance, 4-m walking speed [11], and the 5-repetition sit-to-stand test ranked from 0 to 4. This scale is recognized to assess lower extremity function and mobility in older adults [12].
Unipodal balance
With their arms by their sides, participants were asked to stand on one leg for a maximum of 60 s. Unipodal balance capacity is a predictor of fall risk [13].
Timed-up and go [14]
This test consisted in standing from a sitting position on a chair, walking a 3-m distance, turning around, and then sitting down again. The TUG was performed at normal and fast speeds. This measure is related to the risk of falls [15].
B) Physical performance
- Muscle power
Based on the time needed for the participant to perform 10 sit-to-stand repetitions, a power index was calculated using the validated Takaï equation: \(P=\frac{\left(L-A\right)\times BM\times g\times 10}{T}\) [16], where P = power (watts); L ≡ leg length (the distance from the greater trochanter of the femur to the lateral malleolus) (m); A = height of the chair (m); BM = body mass; g = acceleration due to gravity (9.8 m∙s–2); 10 = number of repetitions; T = time to perform the test, respectively.
Muscle endurance
Participants performed as many sit-to-stand repetitions as they could in 30 s. This test is recognized as a valid indicator of lower body muscular endurance in community-dwelling older adults [17].
C) Anthropometrics
Body mass index (BMI)
Using self-reported body mass (kg) and height (m), BMI was calculated using the following equation: body mass (kg)/height (m2)].
D) Physical health questionnaires
Quality of life
Measured using the EQ-5D questionnaire [18].
Mental health
Psychological distress (anxiety and depression) was evaluated using the Kessler Psychological Distress Scale (K10) [19], while loneliness was evaluated with the UCLA-Loneliness Scale-3 (UCLA-3) questionnaires [20].
Motivation toward PE
The “Échelle de motivation envers l'activité physique en contexte de santé” questionnaire was used to assess motivation toward PE [EMAPS; [21]].
Statistical analyses
Data distributions were tested using the Shapiro–Wilk test. Baseline characteristics were summarized using descriptive statistics. Continuous variables were expressed by means ± standard deviation. Categorical variables were expressed in percentages. A Chi-squared test or Fisher test was used to compare the frequency of observations between groups.
Independent parametric t-tests were used to identify potential between-group differences at baseline (before the start of the intervention). Two-way repeated-measures ANOVA [factors time (pre, post) and group (LRL vs. RLR)] was used to test the effects of each intervention on physical health variables. When a main effect or interaction reached significance, Bonferroni post hoc tests were performed to adjust for multiple comparisons. Partial eta squared (ηp2) were used to report effect sizes, where an ηp2 between 0.06 and 0.01 was considered to be a low effect, between 0.1 and 0.06 was considered a medium, and an ηp2 larger than 0.1 was considered a large effect size [22]. The percentage change from baseline ((pre-post/pre) × 100) was estimated to evaluate and compare the clinical significance of our interventions. All statistical analyses were performed using SPSS 27.0 (Chicago, IL, USA). The significance was set at p ≤ 0.05 (two-tailed) for all analyses.
Results
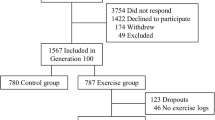
A total of 46 participants were eligible and randomized into two groups: 1) LRL group: Pre: n = 22 (women: 18/men: 4) and Post: n = 19 (women: 15/men: 4). Three participants dropped out due to lack of interest (n = 2) or a medical issue that was unrelated to the intervention (n = 1; unrelated to the program). 2) RLR group: Pre: n = 24 (women: 20/men: 4) and Post: n = 17 (women: 13/men: 4). Seven participants dropped out due to lack of interest (n = 3), a medical issue that was unrelated to the program (n = 3; unrelated to the program) or a move (n = 1).
Baseline participant characteristics were similar between groups (all p ≥ 0.05): Participants were highly educated (% university level: LRL = 81% vs. RLR = 67%, p = 0.56), cognitively intact (T-MMSE (x/30): LRL = 25.2 ± 1.0 vs. RLR = 25.4 ± 1.1, p = 0.90), and functionally (walking speed (m/s): LRL = 0.93 ± 0.20 vs. RLR = 0.91 ± 0.20, p = 0.85; SPPB (x/12): LRL = 10.9 ± 1.1 vs. RLR = 10.7 ± 1.5, p = 0.72) and physically healthy (BMI (kg/m2): LRL = 28.4 ± 3.9 vs. RLR = 27.5 ± 5.5, p = 0.82). The number of prescribed drugs (> 5; %): LRL = 0% vs. RLR = 9.5%, p = 0.15), percentage of women (% women: LRL = 81% vs. RLR = 81%, p = 1.00), and mean age (age (y): LRL = 71.0 ± 7.7 vs. RLR = 69.3 ± 3.5, p = 0.58) were also similar.
Intervention feasibility and acceptability
Among the 46 participants who took part in the intervention, 36 participants completed the study. Group difference in the dropout rate did not reach significance [14% LRL group [Pre: n = 22 (17 women/5 men) to Post: n = 19 (14 women/5 men)] vs. 29% RLR group [Pre: n = 24 (17 women/7 men) to Post: n = 17 (14 women/3 men); p = 0.20]. The reasons for dropping out were similar between groups and occurred throughout the intervention.
Adherence to the intervention was similar between groups [LRL 92% (min–max: 33–36) vs. RLR 85% (min–max:24–36); p = 0.32] among participants who completed the intervention. Moreover, the modality of the session did not influence adherence, which was similar between groups (Monday: LRL = 86% vs. RLR = 74%, p = 0.29; Wednesday: LRL = 73% vs. RLR = 77%, p = 0.66; Friday: LRL = 81% vs. RLR = 77%, p = 0.41).
Acceptability, satisfaction (satisfied or very satisfied (%): LRL = 71% vs. RLR = 74%, p = 0.52), enjoyment (enjoy or enjoy a lot (%): LRL = 89% vs. RLR = 79%, p = 0.38), perceived difficulty (easy or quite easy (%): LRL = 76% vs. RLR = 65%, p = 0.47), and perceived exertion (a little easy /a little difficult (%): LRL = 58/32% vs. RLR = 60/30%, p = 0.32/p = 0.37, respectively) were similar in both groups.
Additionally, satisfaction regarding the modality of the session (live vs. recorded) was slightly but not statistically different between groups (satisfied or very satisfied (%): Monday: LRL = 61% vs. RLR = 52%, p = 0.36; Wednesday LRL = 67% vs. RLR = 68%, p = 0.47; Friday: LRL = 75% vs. RLR = 50%, p = 0.26). Enjoyment was also slightly but not statistically different (enjoy or enjoy a lot (%): Monday: LRL = 93% vs. RLR = 77%, p = 0.45; Wednesday: LRL = 83% vs. RLR = 78%, p = 0.52; Friday: LRL = 95% vs. RLR = 84%, p = 0.40). The perceived difficulty was similar in both groups (easy or quite easy (%): Monday: LRL = 67% vs. RLR = 58%, p = 0.41; Wednesday: LRL = 60% vs. RLR = 50%, p = 0.35; Friday: LRL = 72% vs. RLR = 56%, p = 0.67).
Objective physical health effects of the intervention
The participants’ pre- and post-intervention physical performance is presented in Table 1. A time effect was observed for normal walking speed (p = 0.005, ηp2 = 0.12), normal (p = 0.003, ηp2 = 0.25), and fast Timed-Up and Go (p = 0.007, ηp2 = 0.21), 5-repetition Sit-to-Stand test (p = 0.011, ηp2 = 0.19), muscle power (p = 0.02, ηp2 = 0.27), muscle endurance (p < 0.001, ηp2 = 0.37), and SPPB score (p = 0.012, ηp2 = 0.18). A time × group effect was found for the 5-repetition Sit-to-Stand test (p = 0.013, ηp2 = 0.18), muscle power (p = 0.006, ηp2 = 0.27), and muscle endurance (p < 0.001, ηp2 = 0.34), with the LRL group showing greater improvement than the RLR group.
In addition to greater statistical improvement, the LRL group also had a more clinically significant improvement for muscle power (minimal change expected > 10%: LRL: + 35 ± 16.1 vs. RLR: + 7 ± 13.9, p = 0.010, d = 0.852), muscle endurance (minimal change expected > 7%: 30-s Sit-to-Stand (%): LRL: + 34.7 ± 15.4 vs. RLR: + 27.0 ± 26.5, p < 0.001, d = 1.232), and 5-repetition Sit-to-Stand time (minimal change expected:– 2.3 s; 5-STS (sec): LRL:– 2.38 ± 1.1 s; RLR:– 0.1 ± 1.8 s; p = 0.007, d = – 1.003).
Subjective physical health effects of the intervention
Pre- and post-intervention subjective health parameters are presented in Table 1. No significant change was observed.
Discussion
The purpose of this study was to evaluate and compare the feasibility, acceptability, and health effects of two online exercise interventions, which included a different proportion of live and recorded sessions, in community-dwelling older adults. First, participants from both groups reported that it was “easy” to perform the sessions (LRL:76% vs. RLR: 65%). These results suggest that even if the intensity and the level of difficulty increased every three weeks during the 12-week intervention period, both combined remote exercise interventions were adapted to the participants’ capacities. Furthermore, both groups reported that they were equally “satisfied” with the training program followed during the intervention (LRL:71% vs. RLR:74%). These results are relevant because the level of satisfaction is one of the main factors that enable older adults to participate and stay motivated in their practice of PE [23].
We also observed a high and similar level of enjoyment across modalities (LRL:89% vs. RLR:79%). This aspect is also important as enjoyment is another main reason for older adults to participate in PE and integrate it into their lifestyle habits [24]. Overall, participant perception is very important, especially in older adults, as exercise adherence is related to concordance with their needs and the level of enjoyment during practice [25]. Indeed, we showed a high adherence and acceptability, independent of the modality performed (LRL:92% vs. RLR:85%). Additionally, we observed that the live sessions had slightly higher adherence than the recorded sessions. However, the day of the week when the live or recorded sessions were performed did not seem to impact adherence. Nevertheless, it is important to note that the drop-out rate in the RLR group was higher than in the LRL group (RLR:29% vs.LRL:14%). On average, a drop-out rate around 20% is expected during a 12-week intervention in older adults [14]. One reason that could explain the difference in the dropout rate between both combined remote exercise interventions is the increased interaction due to session settings (group & live vs. alone & recorded). Indeed, it has been shown that PE interventions with group-based activities may reduce loneliness and social isolation by enhancing the feeling of connectedness [26, 27]. Also, group settings allow participants to interact more and more easily with other participants, which is a known factor for decreasing the feeling of loneliness and social isolation [28].
Moreover, we observed that both remote combined exercise interventions improved physical health significantly. However, regarding normal walking speed, only the LRL group showed clinical improvement (minimal change expected > 0.1 m.s−1; delta change (m/sec) = LRL: + 0.13 vs. RLR: + 0.04). More specifically, the LRL group went from normal walking speed to good walking speed (LRL: pre:0.92 m/sec to post: 1.05 m/sec), which is associated with lower health risks and mortality in older adults [29]. In addition, the significant effects observed on muscle power and muscular endurance in both groups are important as these parameters are recognized to be the main predictors of fall risk in older adults [30]. In addition, it has been suggested that a substantial and meaningful clinical change on SPPB (range from 0.4 to 1.5 points; [12]) reduces the risk of adverse health outcomes [31]. Based on our findings on SPPB, our interventions should also be considered effective for improving functional capacities [12, 32]. However, only LRL was associated with a clinically significant change that can reduce the risk of adverse health outcomes (LRL: + 0.8 vs. RLR: + 0.2 point; [31]). Overall, our results are in line with other studies reporting that participation in exercise programs improves health-related fitness, reduces risky behaviors, and helps reduce the use of various health services [33]. However, the differences between the two groups are likely because, during live supervised sessions, the instructor provides instructions to correct participants’ movements, thus improving the quality of the exercise performed. Furthermore, the participants’ motivation, adherence, and engagement are potentiated by the presence of an instructor during in-person training sessions [34] which could have impacted the effectiveness of the intervention on health parameters. Consequently, as the LRL group has a higher ratio of live session with a kinesiologist than the RLR group, the previous arguments could justify the greater observed improvements in the LRL group.
Our subjective health results show that depression, loneliness, and quality of life remained stable in both groups in both interventions, even if the study was conducted during the second COVID-19 lockdown. This point is important as the COVID-19 pandemic has been shown to increase feelings of loneliness in older adults, which impacts physical and mental health [35]. As mentioned previously, these results could be explained by the modalities of our remote interventions (live, interactive, and group) but also by their design. We used follow-up phone calls every three weeks for each participant to ensure their safety and confirm their adherence, which could have positively impacted their feelings of depression or loneliness. Indeed, studies have shown that regular follow-up phone calls, provided by layperson callers, could impact feelings of loneliness and depression over a four-week period, but this has not been confirmed in the longer term in older adults [36]. A social desirability bias may have occurred as participants knew they were being assessed throughout the study.
Nonetheless, our study presents some limitations. First, due to our per-protocol analysis, we only reported results from participants who completed the pre- and post-intervention assessments. Moreover, individuals who participated in our study were fairly educated, healthy, and were already using some technological tools daily. Thus, our findings cannot be generalized to the population since 40% of older adults did not have access to these technologies before the COVID-19 pandemic and did not have the skills to use them. However, a recent study has shown that remote exercise programs are also feasible and acceptable to prevent loss of mobility in pre-disabled older adults during the COVID-19 pandemic [37]. In addition, kinesiologists who performed the assessments were not blinded to the intervention. However, they were not involved in the delivery or creation of the exercise intervention to limit this potential bias. Exercise kinesiologists were blinded to the objectives of the study. Moreover, due to the novelty of the question addressed and the circumstances (study conducted during the second COVID-19 lockdown), we did not perform a power calculation. Thus, our sample size may not have allowed us to observe superiority or inferiority between groups. Finally, the lack of follow-up data to assess whether both groups will maintain their PE levels after the end of the intervention is an additional limitation.
Nevertheless, this study also has some strengths, such as the same number and type of exercises in both interventions, the use of validated measures allowing us to adequately compare one intervention against the other, and the use of a reproducible tool to ensure the safety as well as the tailoring of the intervention to the participants. Additionally, this study suggests great opportunities for promoting healthy aging while providing and specifying the role of remote modalities. Indeed, these remote modalities could be used to fight against sedentary behaviors in multiple structures for the elderly such as geriatric centers and home care where movement is a vital issue and requires continuous encouragement [38]. Finally, future studies should explore the physiological mechanisms responsible for the improved physical performance and functional capacities, such as mitochondrial activity, neuromuscular junction, or metabolic inflammation which are known factors impacting the aging process [39, 40].
Conclusion
This study shows that online exercise interventions combining different types of session modalities are safe and can promote a physically active lifestyle in older adults. Both of these remote combined modalities could help fight against a sedentary/inactive lifestyle caused by lockdowns, extreme weather, or transportation difficulties, providing viable alternatives to full face-to-face training. These results offer insights regarding the different impacts of remote training as well as the optimal ratio for live or recorded training sessions. Indeed, our results show that the modality with the higher ratio of live training leads to greater improvements in muscle function as well as a lower drop-out rate. Overall, our findings are important to help health professionals offer the best modality for their patients according to their motivation but also their financial situation, schedule, or travel (lack of transportation; weather limitations, etc.) constraints.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Ballin M, Hult A, Björk S, Lundberg E, Nordström P, Nordström A (2020) Web-based exercise versus supervised exercise for decreasing visceral adipose tissue in older adults with central obesity: a randomized controlled trial. BMC Geriatrics 20:173. https://doi.org/10.1186/s12877-020-01577-w
Pischke CR, Voelcker-Rehage C, Ratz T, Peters M, Buck C, Meyer J, von Holdt K, Lippke S (2022) Web-based versus print-based physical activity intervention for community-dwelling older adults: crossover randomized trial. JMIR Mhealth Uhealth 10:e32212. https://doi.org/10.2196/32212
Granet J, Peyrusqué E, Ruiz F, Buckinx F, Abdelkader LB, Dang-Vu TT, Sirois MJ, Gouin JP, Pageaux B, Aubertin-Leheudre M (2022) Web-based physical activity interventions are feasible and beneficial solutions to prevent physical and mental health declines in community-dwelling older adults during isolation periods. J Gerontol A Biol Sci Med Sci Jun 8:glac127. https://doi.org/10.1093/gerona/glac127
Schwartz H, Har-Nir I, Wenhoda T, Halperin I (2021) Staying physically active during the COVID-19 quarantine: exploring the feasibility of live, online, group training sessions among older adults. Transl Behav Med 11:314–322. https://doi.org/10.1093/tbm/ibaa141
Wichmann F, Pischke CR, Jürgens D et al (2020) Requirements for (web-based) physical activity interventions targeting adults above the age of 65 years - qualitative results regarding acceptance and needs of participants and non-participants. BMC Public Health 20:907. https://doi.org/10.1186/s12889-020-08927-8
Franco MR, Tong A, Howard K, Sherrington C, Ferreira PH, Pinto RZ, Ferreira ML (2015) Older people's perspectives on participation in physical activity: a systematic review and thematic synthesis of qualitative literature. Br J Sports Med 49:1268–1276. https://doi.org/10.1136/bjsports-2014-094015
Topolski TD, LoGerfo J, Patrick DL, Williams B, Walwick J, Patrick MB (2006) The Rapid Assessment of Physical Activity (RAPA) among older adults. Prev Chronic Dis 3:A118
Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, Tracy JK, Hochberg MC, Rodondi N, Cawthon PM; Study of Osteoporotic Fractures Research Group (2007) Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci 62:744–751. https://doi.org/10.1093/gerona/62.7.744
Newkirk LA, Kim JM, Thompson JM, Tinklenberg JR, Yesavage JA, Taylor JL (2004) Validation of a 26-point telephone version of the Mini-Mental State Examination. J Geriatr Psychiatry Neurol 17:81–87. https://doi.org/10.1177/0891988704264534
Martel D, Lauzé M, Agnoux A, Fruteau de Laclos L et al (2018) Comparing the effects of a home-based exercise program using a gerontechnology to a community-based group exercise program on functional capacities in older adults after a minor injury. Exp Gerontol 108:41–47. https://doi.org/10.1016/j.exger.2018.03.016
Peyrusqué E, Kergoat MJ, Bolduc A, Buckinx F, Law C, Veillette N, Fonseca R, Aubertin-Leheudre M (2021) Maintenance of Autonomy Through exercise in Hospital Setting (MATCH): a feasibility study. J Am Med Dir Assoc 22:873–875. https://doi.org/10.1016/j.jamda.2020.12.043
Guralnik JM, Simonsick EM, Ferrucci L, Glynn R.J, Berkman LF. Blazer DG, Scherr PA, Wallace RB (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85–M94. https://doi.org/10.1093/geronj/49.2.m85
Springer BA, Marin R, Cyhan T, Roberts H, Gill NW (2007) Normative values for the unipedal stance test with eyes open and closed. J Geriatr Phys Ther 30:8–15. https://doi.org/10.1519/00139143-200704000-00003
Unver B, Baris RH, Yuksel E, Cekmece S, Kalkan S, Karatosun V (2017) Reliability of 4-meter and 10-meter walk tests after lower extremity surgery. Disabil Rehabil 39:2572–2576. https://doi.org/10.1080/09638288.2016.1236153
Shumway-Cook A, Brauer S, Woollacott M (2000) Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther 80:896–903
Takai Y, Ohta M, Akagi R, Kanehisa H, Kawakami Y, Fukunaga T (2009) Sit-to-stand test to evaluate knee extensor muscle size and strength in the elderly: a novel approach. J Physiol Anthropol 28:123–128. https://doi.org/10.2114/jpa2.28.123
Jones CJ, Rikli RE, Beam WC (1999) A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport 70:113–119. https://doi.org/10.1080/02701367.1999.10608028
Balestroni G, Bertolotti G (2012) L'EuroQol-5D (EQ-5D): uno strumento per la misura della qualità della vita [EuroQol-5D (EQ-5D): an instrument for measuring quality of life]. Monaldi Archives for Chest Disease = Archivio Monaldi per le malattie del torace 78:155–159. https://doi.org/10.4081/monaldi.2012.121
Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Walters EE, Zaslavsky AM (2002) Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 32:959–976. https://doi.org/10.1017/s0033291702006074
Russell DW (1996) UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess 66:20–40. https://doi.org/10.1207/s15327752jpa6601_2
Boiché J, Gourlan M, Trouilloud D, Sarrazin P (2019) Development and validation of the 'Echelle de Motivation envers l'Activité Physique en contexte de Santé': a motivation scale towards health-oriented physical activity in French. J Health Psychol 24:386–396. https://doi.org/10.1177/1359105316676626
Cohen J (2013) Statistical power analysis for the behavioral sciences. Routledge
Devereux-Fitzgerald A, Powell R, Dewhurst A, French DP (2016) The acceptability of physical activity interventions to older adults: a systematic review and meta-synthesis. Soc Sci Med 158:14–23. https://doi.org/10.1016/j.socscimed.2016.04.006
Allender S, Cowburn G, Foster C (2006)Understanding participation in sport and physical activity among children and adults: a review of qualitative studies. Health Educ Res 21:826–835. https://doi.org/10.1093/her/cyl063
Finch H (1997) Health Education, Physical activity "at our age": qualitative research among people over the age of 50. London: Health Education Authority
Franke T, Sims-Gould J, Nettlefold L, Ottoni C, McKay HA (2021) "It makes me feel not so alone": features of the Choose to Move physical activity intervention that reduce loneliness in older adults. BMC Public Health 21:312. https://doi.org/10.1186/s12889-021-10363-1
Beauchamp MR, Liu Y, Dunlop WL, Ruissen GR, Schmader T, Harden SM, Wolf SA, Puterman E, Sheel AW, Rhodes RE (2021) Psychological mediators of exercise adherence among older adults in a group-based randomized trial. Health Psychol 40:166–177. https://doi.org/10.1037/hea0001060
Sebastião E, Mirda D (2021) Group-based physical activity as a means to reduce social isolation and loneliness among older adults. Aging Clin Exp Res 33:2003–2006. https://doi.org/10.1007/s40520-020-01722-w
Abellan van Kan G, Rolland Y, Andrieu S, Bauer J, Beauchet O et al (2009) Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging 13:881–889. https://doi.org/10.1007/s12603-009-0246-z
Stel VS, Smit JH, Pluijm SM, Lips P (2004) Consequences of falling in older men and women and risk factors for health service use and functional decline. Age Ageing 33:58–65. https://doi.org/10.1093/ageing/afh028
Vasunilashorn S, Coppin AK, Patel KV, Lauretani F, Ferrucci L, Bandinelli S, Guralnik JM (2009) Use of the Short Physical Performance Battery Score to predict loss of ability to walk 400 meters: analysis from the InCHIANTI study. J Gerontol A Biol Sci Med Sci 64:223–229. https://doi.org/10.1093/gerona/gln022
Perera S, Mody SH, Woodman RC, Studenski SA (2006) Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 54:743–749. https://doi.org/10.1111/j.1532-5415.2006.00701.x
Sari N (2011) Exercise, physical activity and healthcare utilization: A review of literature for older adults. Maturitas 70:285–289. https://doi.org/10.1016/j.maturitas.2011.08.004
Ratamess NA, Faigenbaum AD, Hoffman JR, Kang J (2008) Self-selected resistance training intensity in healthy women: the influence of a personal trainer. J Strength Cond Res 22:103–111. https://doi.org/10.1519/JSC.0b013e31815f29cc
Berg-Weger M, Morley JE (2020) Editorial: loneliness and social isolation in older adults during the COVID-19 pandemic: implications for gerontological social work. J Nutr Health Aging 24:456–458. https://doi.org/10.1007/s12603-020-1366-8
Kahlon MK, Aksan N, Aubrey R, Clark N, Cowley-Morillo M, Jacobs EA, Mundhenk R, Sebastian KR, Tomlinson S (2021) Effect of layperson-delivered, empathy-focused program of telephone calls on loneliness, depression, and anxiety among adults during the COVID-19 pandemic: a randomized clinical trial. JAMA Psychiatry 78:616–622. https://doi.org/10.1001/jamapsychiatry.2021.0113
Buckinx F, Aubertin-Leheudre M, Daoust R, Hegg S, Martel D, Martel-Thibault M, Sirois MJ (2021) Feasibility and acceptability of remote physical exercise programs to prevent mobility loss in pre-disabled older adults during isolation periods such as the COVID-19 pandemic. J Nutr Health Aging 25:1106–1111. https://doi.org/10.1007/s12603-021-1688-1
Rincé G, Couturier C, Berrut G, Dylis A, Montero-Odasso M, Deschamps T (2021) Impact of an individual personalised rehabilitation program on mobility performance in older-old people. Aging Clin Experimental Res 33:2821–2830. https://doi.org/10.1007/s40520-021-01812-3
Lippi L, Uberti F, Folli A, Turco A, Curci C, d'Abrosca F, de Sire A, Invernizzi M (2022) Impact of nutraceuticals and dietary supplements on mitochondria modifications in healthy aging: a systematic review of randomized controlled trials. Aging Clin Exp Res 34:2659–2674. https://doi.org/10.1007/s40520-022-02203-y
Lippi L, de Sire A, Mezian K, Curci C, Perrero L, Turco A, Andaloro S, Ammendolia A, Fusco N, Invernizzi M (2022) Impact of exercise training on muscle mitochondria modifications in older adults: a systematic review of randomized controlled trials. Aging Clin Exp Res 34:1495–1510. https://doi.org/10.1007/s40520-021-02073-w
Acknowledgements
The authors would like to thank all the trainees and research assistants who took part in the study. Finally, we would like to thank all the older adults who participated in this study.
Funding
This work was supported by operational funds from MAL (UQAM-FRQS). The study’s website (www.trainingrecommend.com) was partly supported by a grant from the Centre de recherche de l’Institut Universitaire de Gériatrie de Montréal (CRIUGM COVID-19 grant support). MAL (senior salary award), TDV (senior salary award), BP (junior 1 salary award), and FB (post-doctoral fellowship) were supported by the Fonds de recherche du Québec en santé (FRQS). JPG was supported by a Canada Research Chair grant. FB received also a post-doctoral fellowship from the Canadian Institutes of Health Research (CIHR). JG, EP, and FR received a scholarship from Centre de recherche de l’Institut Universitaire de Gériatrie de Montréal (CRIUGM or CRIUGM-AGEWELL scholarship).
Author information
Authors and Affiliations
Contributions
MAL designed and led the project and supervised all the steps of this article. JG recruited, performed some assessments, analyzed the data, and wrote the manuscript. EP, FR, FB, and LBA performed some assessments and revised the manuscript. BP, TTDV, JPG, and MJS contributed to the design or methods of the research and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was performed according to the principles of the Declaration of Helsinki. This study has been approved by the Ethics Committee of the Centre de recherche de l’Institut Universitaire de Gériatrie de Montréal (CRIUGM; CERVN 20–21-05).
Informed consent
All participants signed a consent form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Granet, J., Peyrusqué, E., Ruiz, F. et al. Online physical exercise intervention in older adults during lockdown: Can we improve the recipe?. Aging Clin Exp Res 35, 551–560 (2023). https://doi.org/10.1007/s40520-022-02329-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02329-z