Abstract
Background and aim
To compare blood and salivary levels of lipofuscin in healthy adults and to analyze the relationship between the lipofuscin level and the healthy adults’ age.
Methods
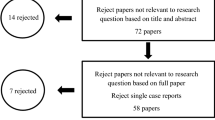
One hundred and twenty-two healthy volunteers were recruited and divided into three groups according to their age: young (n = 42, 20–44 years old), middle-aged (n = 51, 45–59 years old), and elderly (n = 29, 60–74 years old). One ml saliva and 5 ml whole blood were collected from each person. An ELISA kit was used to measure both the plasma and salivary lipofuscin levels. The differences between the groups were compared with independent-sample t test, and the relationship between the salivary lipofuscin level and the age was assessed with linear regression analysis.
Results
The mean ± SD of the lipofuscin level in the saliva and plasma of 122 subjects was 68.93 ± 1.32 and 78.05 ± 1.75 μmol/l, respectively. No gender-dependent differences were observed in either the salivary or the plasma lipofuscin level (saliva: p = 0.443, plasma: p = 0.459). The salivary and plasma lipofuscin levels of the elderly subjects were significantly higher than those of the young (saliva: 80.72 ± 13.53 mmol/l versus 59.12 ± 1.92 mmol/l, p = 0.0003; plasma: 93.31 ± 3.14 mmol/l versus 67.43 ± 2.54 mmol/l, p = 0.0002) and middle-aged (saliva: 80.72 ± 13.53 mmol/l versus 70.31 ± 11.17 mmol/l, p = 0.0004; plasma: 93.31 ± 3.14 mmol/l versus 78.12 ± 2.40 mmol/l, p = 0.0002) subjects. Similarly, the salivary and plasma lipofuscin levels of the middle-aged subjects were significantly higher than those of the young subjects (saliva: 70.31 ± 11.17 mmol/l versus 59.12 ± 1.92 mmol/l, p < 0.0001; plasma: 78.12 ± 2.40 mmol/l versus 67.43 ± 2.54 mmol/l, p = 0.0019). The lipofuscin levels in the saliva and plasma were significantly positively correlated with the subject age (r = 0.551, p = 0.0001; r = 0.528, p < 0.0001). Furthermore, the salivary lipofuscin level and plasma lipofuscin level also were found to have a positive correlation (r = 0.621, p < 0.0001).
Conclusion
No gender-dependent differences were observed in either the salivary or plasma lipofuscin levels. The salivary and plasma lipofuscin levels were positively correlated, and the age is positively correlated with lipofuscin content in saliva.





Similar content being viewed by others
References
Hannover A (1842) Mikroskopische untersdgelsen auf nervensystem. Videnskapsselsk Naturvidensk Math Afu 10:1–112
Brunk ULFT, Terman A (2002) Lipofuscin: mechanisms of age-related accumulation and influence on cell function. Free Radic Biol Med 33:611–619
Brunk ULFT, Terman A (2002) The mitochondrial-lysosomal axis theory of aging. Eur J Biochem 269:1996–2002
Knight JA (2001) The biochemistry of aging. Adv Clin Chem 35:1–62
Rikans LE, Hornbrook KR (1997) Lipid peroxidation, antioxidant protection and aging. Biochim Biophys Acta 1362:116–127
Terman A, Brunk ULFT (1998) Lipofuscin: mechanisms of formation and increase with age. Apmis 106:265–276
Kim SU, Warren KG, Kalia M (1979) Tissue culture of adult human neurons. Neurosci Lett 11:137–141
Samorajski T, Ordy JM, Keefe JR (1965) The fine structure of lipofuscin age pigment in the nervous system of aged mice. J Cell Biol 26:779–795
Tonna EA (1975) Accumulation of lipofuscin (age pigment) in aging skeletal connective tissues as revealed by electron microscopy. J Gerontol 30:3–8
Brizzee KR, Johnson FA (1970) Depth distribution of lipofuscin pigment in cerebral cortex of albino rat. Acta Neuropathol 16:205–219
Wu CX, Wei XB (2006) Influence of effective parts of zingiber officinale on senium of rats resulting from high fat die. J Shandong Med Coll 3:010
Li GL, Liu L, Hu H (2010) Age-related carbonyl stress and erythrocyte membrane protein carbonylation. Clin Hemorheol Microcirc 46:305–311
Terman A, Brunk ULFT (2004) Lipofuscin. Int J Biochem Cell Biol 36:1400–1404
Double KL, Dedov VN, Fedorow H et al (2008) The comparative biology of neuromelanin and lipofuscin in the human brain. Cell Mol Life Sci 65(11):1669–1682
Nozynski J, Zakliczynski M, Konecka-Mrowka D et al (2013) Advanced glycation end products and lipofuscin deposits share the same location in cardiocytes of the failing heart. Exp Gerontol 48(2):223–228
WHO Regional Office for Europe (2008) Healthy ageing profiles. http://www.euro.who.int/__data/assets/pdf_file/0011/98399/E91887.pdf. Accessed July 2013
Atil H, Unver Y (2001) Multiple comparisons. Online J Biol Sci 1(8):723–727
Beregi E, Regius O (1983) Lipofuscin in lymphocytes and plasma cells in aging. Arch Gerontol Geriatr 2(3):229–235
Weiter JJ, Delori FC, Wing GL (1986) Retinal pigment epithelial lipofuscin and melanin and choroidal melanin in human eyes. Invest Ophthalmol Vis Sci 27(2):145–152
Jung T, Bader N, Grune T (2007) Lipofuscin. Ann NY Acad Sci 1119(1):97–111
Höhn A, Grune T (2013) Lipofuscin: formation, effects and role of macroautophagy. Redox Biol 1(1):140–144
Head E (2013) A canine model of human aging and Alzheimer’s disease. Biochim Biophys Acta 1832(9):1384–1389
Calderón L, Franco M, Mora A (2013) Early Alzheimer’s and Parkinson’s disease pathology in urban children: friend versus foe responses—it is time to face the evidence. Biomed Res Int 2013:161687
Ablonczy Z, Higbee D, Anderson DM (2013) Lack of correlation between the spatial distribution of A2E and lipofuscin fluorescence in the human retinal pigment epithelium. Invest Ophthalmol Vis Sci 54(8):5535–5542
Fernandez CJP, Mullins RF, Manea AM (2013) Lipofuscin in human glaucomatous optic nerves. Exp Eye Res 111:61–66
Acknowledgments
The authors thank all volunteers and teachers at the Dental Institute of the General Hospital of the People’s Liberation Army of China. This work was supported by the Key Project of the Chinese National Programs for Fundamental Research and Development (973 Program) (2007CB-507405) and by Program 973.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standard
The use of clinical data was requested and approved by local ethical committee although exams were performed according to clinical indications.
Informed consent
All patients gave written informed consent to the procedure.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feng, FK., E, LL., Kong, XP. et al. Lipofuscin in saliva and plasma and its association with age in healthy adults. Aging Clin Exp Res 27, 573–580 (2015). https://doi.org/10.1007/s40520-015-0326-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-015-0326-3