Abstract
Introduction
Pharyngocutaneous fistula (PCF) remains the most frequent complication following total laryngectomy (TL). Pharyngeal closure with a surgical stapler (SAPC) has been proposed as an effective closure technique that decreases the rate of PCF, reduces surgical time, decreases the length of hospital stay, and shortens the time required before safely initiating oral feeding.
Methods
This study involved a systematic review and meta-analysis of patients with laryngeal cancer who underwent TL and with subsequent stapler pharyngeal closure, in order to analyse the current literature regarding the role of SAPC after TL.
Results
The incidence of PCF in the stapler-assisted suture group (SASG) was 9.5% (95% CI 8.2–15.9%), with a mean absolute deviation of 1.12, while in the hand-suture group (HSG) group the incidence was 23.4% (95% CI 23–26.1%), with a mean absolute deviation of 5.71 (p = 0.01).
Conclusions
SAPC may decrease the risk of PCF in patients following TL. Based on the current data, SAPC appears to shorten the surgical time and the length of hospital stay. Nevertheless, prospective randomized trials are required to validate these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laryngeal cancer represents a major global health problem. |
The occurrence of pharyngocutaneous fistula (PCF) is the most common and feared surgical complication following total laryngectomy (TL). |
The most critical and time-consuming surgical step in TL is the closure of the pharyngeal mucosa. |
Performing a stapler-assisted pharyngeal closure in patients undergoing TL may decrease the risk of PCF. |
Due to the low evidence level, additional prospective randomized trials investigating the impact of this technique on surgical time, length of hospital stay, and complication rates are required to determine whether these results can be translated into improved surgical safety. |
Introduction
Laryngeal cancer (LC) represents a major global health problem. In 2019, LC affected 177,422 patients worldwide, causing 94,771 deaths [1, 2]. Total laryngectomy (TL) is the treatment of choice for some LCs, and due to the extent of this surgery, it is reserved for patients with advanced-stage LC. Multiple post-operative complications have been described following TL, including wound infection, surgical bleeding, chyle leak, and pharyngocutaneous salivary fistula (PCF) [3].
The occurrence of PCF is the most common and feared surgical complication following TL. Post-operative PCF is associated with significant morbidity, extended hospital stays, higher healthcare costs, and delayed complementary treatment [4, 5]. Proposed risk factors of PCF are contentious, and include previous tracheotomy, hypothyroidism, low post-operative haemoglobin, and previous treatment with radiotherapy (RT) or chemoradiotherapy (CRT) [6, 7].
Stapler devices, initially developed by Hultl et al., have been utilized in general surgery since the mid-twentieth century [8]. The first application of mechanical sutures in head and neck surgery was for the treatment of Zenker's diverticulum in 1969 [10]. The first reported use of the linear stapler for pharyngeal closure following TL was by Lukyanchenko et al. in 1971 [10].
The most critical and time-consuming surgical step in TL is the closure of the pharyngeal mucosa. The classic technique has three variants of manual pharyngeal closure: the linear, the T-type, and the “tobacco pouch”. Different types of stapler closure techniques have also been described [11]. In the closed type [4, 10, 12] the larynx is skeletonized, the trachea is cut, and the epiglottis is tractioned with an Allis clamp inferiorly through the tracheal lumen in a blind manner. The stapler is subsequently placed inferiorly to the oesophageal mucosal edge. The advantage of this technique is the avoidance of a pharyngeal mucosal opening. However, a small section of the epiglottis can inadvertently be added to the stapled suture line, causing a PCF [12]. To avoid this, a semi-closed technique [6] was described. A small median pharyngotomy incision at the level of the supraglottic larynx enables traction of the epiglottis outside of the stapled suturing line. However, this technique requires a small opening of the pharyngeal mucosa [11]. Talmi et al. described an open technique in which the mucosal edges are closed using a stapler after a standard laryngectomy [13]. This technique enables the assessment of tumour extent and margins, which is not possible in a closed technique [13].
Following the original descriptions in the literature, this technique gained popularity, and certain advantages were observed, including the reduction in surgical time; earlier commencement of oral feeding; shorter in-hospital stay; decreased incidence of PCF; and decreased contamination of the surgical field by secretions from the mouth and pharynx due to the watertight closure [14].
In a systematic review of four studies performed by Aires et al. authors examined the effects of stapler-assisted pharyngeal closure (SAPC) after TL. The authors reported a lower incidence of PCF, a shorter time to starting oral feeding, and a shorter hospitalization period when compared to hand-suture closure [15].
This review aims to analyse the current literature regarding the role of SAPC after TL to assess and provide up-to-date evidence.
Methods
This systematic review adopted the population, intervention, comparison, outcome, timing, and setting (PICOTS) [16] modelling throughout and aimed to follow the guidelines proposed by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [17]. Papers included in the meta-analysis were selected according to the inclusion and exclusion criteria. This article is an initiative of the Young Otolaryngologist Group of the International Federation of Otolaryngologic Societies (YO-IFOS), and members and invitees of the International Head and Neck Scientific Group (IHNSG), in compliance with ethics guidelines and following the principles of the Helsinki Declaration.
Types of Studies
The authors considered prospective and retrospective controlled or uncontrolled studies investigating the role of the SAPC. Studies had to be published in English, Italian, German, Spanish, or French in peer-reviewed journals. Only studies reporting data for > 10 patients per arm were considered for inclusion.
-
Participants, inclusion/exclusion criteria: Publications were considered for analysis if they reported on the results of human patients with LC who underwent TL and with subsequent closure using an SAPC. The studies needed to describe the type of stapler device used, type of closure (closed or open technique), and PCF rate, and they had to include a control group of patients who underwent manual closure. Surgical time, time to the initiation of oral feeding, and the length of hospital stay were considered requirements for analysis. The following were exclusion criteria: supraglottic and hypopharyngeal carcinomas; case series, case reports, and studies without a control group (manual closure); the use of mechanical stapling for post-laryngectomy open pharyngotomy closure; and articles only related to salvage TL.
-
Intervention and comparison: This study investigated the role of SAPC following TL for the treatment of laryngeal cancer.
-
Outcomes: The primary outcome evaluated in this study was the incidence of PCF. The secondary outcomes were the length of hospital stay until discharge, surgical time, and the period until initiation of oral feeding.
-
Follow-up period: A 3-month period was regarded as the minimum median follow-up period to evaluate the surgical outcome following surgery.
-
Setting: Surgical hospital studies.
Search Strategy
This review involved a systematic search of the electronic databases including MEDLINE/PubMed, Embase, Google Scholar, SciELO, Scopus, Cochrane Database of Systematic Reviews, and Cochrane Central Register of Controlled Trials, conducted by three independent authors (C.CH.E., JM.P.G., and M.M.Y.), identifying articles published between January 1971 and January 2020 on the use of different stapler devices in pharyngeal closure following TL. Studies were screened if they had database abstracts, available full texts, or titles referring to the condition. The following keywords were used: “laryngectomy”; “total laryngectomy”; “surgical stapler”; “pharyngocutaneous fistula”; “stapler closure”; “pharyngeal closure”. The grey literature was not included.
Assessment of Quality and Risk of Bias Analysis
The methodological quality of the identified studies was appraised using the Oxford Centre for Evidence-Based Medicine (OCEBM) levels of evidence [18]. According to this, prospective or retrospective studies (grading A-B) were included. The bias analysis of included studies was evaluated with the CLARITY Group's tool to assess risk of bias [19].
Statistical Analysis
A meta-analysis of selected studies with an odds ratio (OR) comparing information about PCF, surgical time, length of stay, and time until initiation of oral feeding was performed. The comparison was made by the Cochrane Review Manager 5.4 (Nordic Cochrane Centre, Cochrane Collaboration, 2020, Copenhagen, Denmark). The heterogeneity was checked using the Q test and I2 test. A random-effects model was considered most appropriate if the I2 value was > 50%.
Cochrane Review Manager uses the Mantel–Haenszel and inverse variance method for calculating the weighted summary OR under the random-effects model, due to the heterogeneity. The pooled OR with 95% CI is given for the random-effects model.
Furthermore, a chi-square test with Yates correction for continuity was applied with a two-tailed p value for the comparison of proportions according to sex and histological differentiation from independent samples. A value of p ≤ 0.05 was considered statistically significant.
Results
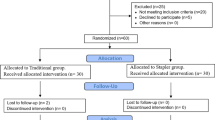
The literature search resulted in a total of 516 manuscripts. Twenty-four studies met our inclusion criteria. Among them, 16 were excluded for the following reasons: the use of mechanical stapling for post-laryngectomy open pharyngotomy closure (N = 2), case series (N = 4), single-arm studies (N = 8), and studies only including patients who underwent salvage TL (N = 2). In total, eight studies were included in our final statistical analysis (Fig. 1) [4, 11, 12, 20,21,22,23,24]. According to the OCEBM grading system, seven studies received a grading of 2b and one study was graded as 3b. The demographic data of the included studies are summarized in Tables 1, 2, and 3. Risk of bias, according to the CLARITY Group, are included in Table 4.
The stapler-assisted suture group (SASG) consisted of 242 patients, while the hand-suture group (HSG) consisted of 380 patients. A comparison of age, sex, T stage, N stage, and previous treatment is summarized in Table 3, with data only included from those articles which had a description of all these variables. The demographic data were similar between the groups. However, we found a difference between the groups according to previous RT or CRT, and the type of neck dissection performed. This makes both cohorts adequately partially homogenous for comparison.
The incidence of PCF in the SASG was 9.5% (95% CI 8.2–15.9%), with a mean absolute deviation of 1.12, while in the HSG group it was 23.4% (95% CI 23–26.1%), with a mean absolute deviation of 5.71 (p = 0.01) (Fig. 2). The absolute risk reduction was 14% (95% CI, 13.5% to 16.3%; p = 0.04; I2 = 53%), and the number needed to treat was 7 to obtain this benefit.
Three articles include data about the length of hospital stay [4, 21, 23]. After comparison, patients who underwent stapler-assisted closure had a shorter hospital stay when compared to those who underwent manual suture, with an average difference of 4 days (95% CI 0.05–8.19 days; p = 0.05; I2 = 81%) (Fig. 3). Despite the absence of surgical time data in all the papers published after the meta-analysis of Aires et al. [15], we decided to include the data and the results obtained. Surgical time was 79.92 min shorter on average when a SAPC was performed compared to the HSG (95% CI, 23.31–136.54 min; p = 0.006). Of note is the heterogeneity among the studies (I2 = 97%) (Fig. 4).
Two articles include information on the time from surgery until the initiation of oral feeding [21, 22]. We cannot make a comparison due to the absence of a standard deviation by the group in the paper of Özturk et al. [22]. However, in both studies, the average time required for the removal of nasogastric feeding tubes (NGT) or until initiation of oral feeding was shorter in the SASG in comparison with the HSG. The difference between groups was significantly in favour of mechanical suturing in the study by Santaolalla et al. (95% CI 4.01–11.73 days; p ≤ 0.001).
Discussion
According to the results of the current meta-analysis, the incidence of PCF was 18% among the studies included. The risk of PCF was lower, the length of hospital stays shorter, and surgical time quicker in the SASG compared to the HSG. Furthermore, the time until initiation of oral feeding or until the removal of the NGT was shorter in the SASG. However, the heterogeneity among the studies, despite the use of a random-effects model, was considerably higher in all the subgroups analysed (53–97%), limiting the validity of our results.
PCF continues to be the most common complication after TL. Its incidence ranges from 9 to 25% in patients after primary TL, and 14% to 57% in patients following salvage laryngectomy [25, 26]. Different stapler-assisted closure techniques have been described in the last four decades. However, hand closure continues to be the preferred technique in most head and neck units.
In the most extensive stapler-assisted TL series, Bedrin et al. published their 25-year experience on the use of the linear stapler, which also represents the largest series, with 1415 patients. They concluded that the use of SAPC techniques decreases surgical time, provides a watertight closure, improves haemostasis, and prevents field contamination. These outcomes are achieved without increasing the PCF rate and with good speech and deglutition outcomes [10].
However, there are some notable limitations that need consideration before the regular use of staplers for pharyngeal closure following TL. This includes the inability to visualize the tumour during resection, thereby limiting the assessment of the extent of the primary tumour into other subsites such as the hypopharynx, and also limiting the need to obtain tumour-free resection margins [20]. Therefore, this procedure needs to be reserved for intra-laryngeal or laryngeal tumours with anterior extra-laryngeal extension, based on a careful preoperative assessment [27, 28]. Additionally, it is important to consider that the utilization of frozen sections after resection for the evaluation of surgical margins becomes difficult and unsuitable after the use of a stapler [22].
As described by Aires et al., favourable outcomes following TL include a tension-free suture line, watertight closure of the pharynx, and haemostasis with preserved viability of the mucosa. The use of the stapler allows surgeons to reach these objectives. Furthermore, at the end of the procedure, double-staggered rows of staples remain in the pharynx and the laryngeal specimen, minimizing the risk of contamination of the surgical field with secretions from the aerodigestive tract [15].
Although this meta-analysis excludes those studies which only include patients following salvage TL, a recent paper published by Galli et al. [29] concluded that the use of a stapler in salvage TL allows the authors to decrease the operative time and hospitalization length, while also providing faster re-initiation of oral feeding and a decreased fistula rate. However, as highlighted by this author, its role in salvage laryngectomy should be validated by further studies. Another study by Allegra et al. [30] demonstrates the feasibility of SASG use in patients older than 70 years.
This study has some limitations. As mentioned previously, there are significant differences among data reported in the included papers. In the studies performed by Goncąlves et al. [12] and Dedivitis et al. [20], authors described data collection as prospective. However, the first paper compared their results with a historical cohort and both studies describe the PCF rate only. The absence of other data and variables in this study can be considered inconsistent for a prospective study. Furthermore, in both studies, we identify bias in the patients’ selection criteria, and heterogeneity regarding the type of neck dissection description, previous RT, and clinical staging. In the article of Santaolalla et al. [21], there was a lack of data regarding age, sex, comorbidities, TNM staging, the primary site of the tumour, risk factors, and the criteria for patient selection. A bias in patient selection was observed in the study of Calli et al. [4], and in the studies performed by Miles et al. [24] and Sannikorn et al. [23], there is a lack of information on TNM staging, systemic treatment, neck dissection, and previous tracheostomy. In the study performed by Miles et al. [24], patients were not classified according to sex, and in the study performed by Özturk et al. [22], the authors do not include specific information regarding neck dissection. Finally, as we described above, only three articles included data on the length of hospital stay [4, 21, 23], and only two articles had information about time until initiation of oral feeding [21, 22]. These inconsistencies were the main limitations to performing an analysis with unbiased objective results. Other factors that can contribute to the heterogeneity are the differences among staplers used across the literature, and the different stapler supported techniques.
Well-designed prospective randomized trials are required to understand the potential benefit of this technique in patients undergoing TL, with a homogeneous surgical technique, proper randomization of patients according to previous treatment received, or exclusion of those who received previous surgical or non-surgical treatment, and the inclusion of an economic analysis to thoroughly compare the hand-suturing technique to the stapler-assisted suturing technique.
Conclusion
Performing a stapler-assisted pharyngeal closure in patients undergoing TL may decrease the risk of PCF. However, due to the low evidence level, additional prospective randomized trials investigating the impact of this technique on surgical time, length of hospital stay, and time period until the initiation of oral feeding are required to determine whether these results can be translated into improved surgical safety.
References
Global Cancer Observatory. Retrieved. Larynx fact sheet. 2019.
Nocini R, Molteni G, Mattiuzzi C, Lippi G. Updates on larynx cancer epidemiology. Chin J Cancer Res. 2020;32:18–25.
LeBlanc BJ, Shi R, Mehta V, Mills G, Ampil F, Nathan CAO. Improvements in survival and disparities for advanced-stage laryngeal cancer. JAMA Otolaryngol Head Neck Surg. 2015;141:169–73.
Calli C, Pinar E, Oncel S. Pharyngocutaneous fistula after total laryngectomy: Less common with mechanical stapler closure. Ann Otol Rhinol Laryngol. 2011;120:339–44.
Dedivitis RA, Ribeiro KC, Castro MA, et al. Pharyngocutaneous fistula following total laryngectomy. Acta Otorhinolaryngol Ital. 2007;27:2–5.
Benson EM, Hirata RM, Thompson CB, Ha PK, Fakhry C, Saunders JR, et al. Pharyngocutaneous fistula after total laryngectomy: a single-institution experience, 2001–2012. Am J Otolaryngol. 2015;36(1):24–31.
Sayles M, Grant DG. Preventing pharyngo-cutaneous fistula in total laryngectomy: a systematic review and meta-analysis. Laryngoscope. 2014;124(5):1150–63.
Zeebregts CJ, Heijmen RH, van den Dungen JJ, van Schilfgaarde R. Non-suture methods of vascular anastomosis. Br J Surg. 2003;90:261–71.
Halevy A, Sadé J. The use of thoracoabdominal staplers in ENT surgery. Arch Otorhinolaryngol. 1983;237:185–90.
Bedrin L, Ginsburg G, Horowitz Z, Talmi YP. 25-year experience of using a linear stapler in laryngectomy. Head Neck. 2005;27:1073–9.
Ismi O, Unal M, Vayisoglu Y, Yesilova M, Helvaci I, Gorur K, Ozcan C. Staple esophageal closure during total laryngectomy. J Craniofac Surg. 2017;28:e35–40.
Goncąlves AJ, de Souza JA, Menezes MMB, et al. Pharyngocutaneous fistulae following total laryngectomy comparison between manual and mechanical sutures. Eur Arch Otorhinolaryngol. 2009;266:1793–8.
Talmi YP, Finkelstein Y, Gal R, Shvilli Y, Sadov R, Zohar Y. Use of a linear stapler for postlaryngectomy pharyngeal repair: a preliminary report. Laryngoscope. 1990;100:552–5.
Paddle P, Husain I, McHugh L, Franco R Jr. Outcomes of mechanical stapling for postlaryngectomy open pharyngotomy closure. Laryngoscope. 2017;127:605–10.
Aires FT, Dedivitis RA, Castro MA, Bernardo WM, Cernea CR, Brandao LG. Efficacy of stapler pharyngeal closure after total laryngectomy: a systematic review. Head Neck. 2014;36:739–42.
Thompson M, Tiwari A, Fu R, Moe E, Buckley DI. A framework to facilitate the use of systematic reviews and meta-analyses in the design of primary research studies. Rockville: Agency for Healthcare Research and Quality (US); 2012.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:1000097.
Howick J, Chalmers I, Glasziou P et al (2011) The 2011 Oxford CEBM levels of evidence (introductory document). https://www.cebm.net/index.aspx?o=5653. Published 2011. Accessed 16 Sept 2019.
Viswanathan M, Berkman ND, Dryden DM, Hartling L. Assessing risk of bias and confounding in observational studies of interventions or exposures: further development of the RTI item bank. Agency for Healthcare Research and Quality; 2013
Dedivitis RA, Aires FT, Pfuetzenreiter E Jr, Castro MAF, Guimaraes AV, Ribeiro DA. Stapler suture of the pharynx after total laryngectomy. Acta Otorhinolaryngol Ital 2013
Santaolalla Montoya F, Ruiz de Galarreta JC, Sánchez del Rey A, Martínez Ibargüen A, Zabala López de Maturana A. Comparative study of the use of manual and mechanical suturing in the closure of the mucosal defect in total laryngectomy. Acta Otorrinolaringol Esp. 2002;53:343–50.
Öztürk K, Turhal G, Öztürk A, Kaya İ, Akyıldız S, Uluöz Ü. The Comparative Analysis of Suture versus Linear Stapler Pharyngeal Closure in Total Laryngectomy: A Prospective Randomized Study. Turk Arch Otorhinolaryngol. 2019;57:166–70.
Sannikorn P, Pornniwes N. Comparison of outcomes for staple and conventional closure of the pharynx following total laryngectomy. J Med Assoc Thai. 2013;96(Suppl 3):S89-93.
Miles BA, Larrison D, Myers LL. Comparison of complication rates associated with stapling and traditional suture closure after total laryngectomy for advanced cancer. Ear Nose Throat J. 2013;92:392–9.
Cavalot AL, Gervasio CF, Nazionale G, Albera R, Bussi M, Staffieri A, et al. Pharyngocutaneous fistula as a complication of total laryngectomy: review of the literature and analysis of case records. Otolaryngol Head Neck Surg. 2000;123:587–92.
Chiesa Estomba CM, González García JA, Sistiaga Suarez JA, Thomas Arrizabalaga I, Larruscain Sarasola E, Altuna MX. Efficacy of the myofascial pectoralis major flap in the reduction of salivary fistulas after salvage total laryngectomy. Acta Otorrinolaringol Esp. 2018;69:99–104.
Simoncelli C, Altissimi G. Mechanical sutures of the pharynx during total laryngectomy: proposal of a closed technique. Acta Otorhinolaryngol Ital. 1990;10:465–74.
Altissimi G, Frenguelli A. Linear stapler closure of the pharynx during total laryngectomy: a 15-year experience (from closed technique to semiclosed technique). Acta Otorhinolaryngol Ital. 2007;27:118–22.
Galli J, Salvati A, Di Cintio G, Mastrapasqua RF, Parrilla C, Paludetti G, Almadori G. Stapler use in salvage total laryngectomy: a useful tool? Laryngoscope. 2020. https://doi.org/10.1002/lary.28737.
Allegra E, Mantia I, Azzolina A, Natale M, Trapasso S, Saita V. Total laryngectomy with horizontal mechanical closure of the pharyngoesophagectomy: evaluation of the effectiveness in elderly patients. Int Arch Otorhinolaryngol. 2019;23:e338–42.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions:
Conceptualization, Carlos M Chiesa-Estomba, Miguel Mayo-Yanez and Jose M Palacios-García; methodology, Jerome Lechien; validation, Jose A González-García, and Jon A Sistiaga-Suarez; formal analysis, Miguel Mayo-Yanez; investigation, Carlos M Chiesa-Estomba, Miguel Mayo-Yanez and Gerrit Viljoen; data curation, Maria R Barillari; writing—original draft preparation, Carlos M Chiesa-Estomba and Gerrit Viljoen; writing—review and editing, Jesus Herranz González-Botas and Tareck Ayad; supervision, Alio Ferlito.
Disclosures
Carlos M Chiesa-Estomba, Miguel Mayo-Yanez, Jose M Palacios-García, Jerome Lechien, Gerrit Viljoen, Petros D Karkos, Maria R Barillari, Jose A González-García, Jon A Sistiaga-Suarez, Jesus Herranz González-Botas, Tareck Ayad and Alio Ferlio confirm that they have no conflicts of interest to disclose.
Compliance with Ethics Guidelines
This systematic review is an initiative of the “Young Otolaryngologist Group of the International Federation of Otolaryngologic Societies” (YO-IFOS), and members and invitees of the International Head and Neck Scientific Group (IHNSG), were in compliance with ethics guidelines and followed the principles of the Helsinki Declaration of 1964 and its later amendments. Ethical approval by a committee was not required.
Data Availability
All data generated or analyzed during this study are included in this published article, figures and tables.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article was written by members and invitees of the International Head and Neck Scientific Group (www.IHNSG.com).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chiesa-Estomba, C.M., Mayo-Yanez, M., Palacios-García, J.M. et al. Stapler-Assisted Pharyngeal Closure After Total Laryngectomy: A Systematic Review and Meta-Analysis. Oncol Ther 10, 241–252 (2022). https://doi.org/10.1007/s40487-022-00193-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40487-022-00193-5