Abstract
Purpose
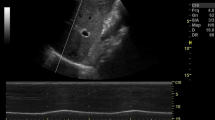
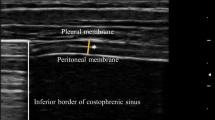
We have focused on the two-dimensional (B-mode) and the time-motion (M-mode) analysis of the zone of apposition to determine the reliability of diaphragm ultrasonography in the clinical environment.
Methods
Ten healthy volunteers were enrolled and studied by three operators with different skills in ultrasonography. For every volunteer, each operator acquired three images of the diaphragm for each side, both in B-mode and in M-mode. Then a fourth operator calculated the thickening fraction (TF), by means of the formula TF = (TEI − TEE)/TEE (TEI is the thickness at end inspiration and TEE the thickness at end expiration). Afterwards, intraclass correlation coefficients (ICCs) were computed on TF to establish reproducibility and repeatability both in the B- and M-modes. A Coefficient of Repeatability or repeatability (CR) ≤ 0.3 was considered acceptable.
Results
Both B-mode (CRs 0.16–0.26) and M-mode (CRs 0.10–0.15) were sufficiently repeatable to assess TF, except for the less experienced operator (CRs B-Mode 0.20–0.32). Reproducibility was moderate to good between operators with CRs much narrower for the M-Mode (0.13–0.14).
Conclusions
The results of our study have shown that diaphragm ultrasound is repeatable and reproducible when carried out by a radiologist or an intensivist with a basic curriculum in ultrasonography. The method is more accurate when using the M-mode for less experienced operators, and in this case, repeatability and reproducibility are not sufficient to make clinical decisions. No TF value lower than 36% was obtained using both techniques. This suggests the existence of a cut-off value that could be used as an initial tool to discriminate healthy subjects from those affected by diaphragmatic dysfunction.
Clinical trial registration
EUDRACT 2015-004635-12.


Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- M-mode:
-
Time-motion ultrasonography
- B-mode:
-
Two-dimensional morphological ultrasonography
- ZOA:
-
Zone of apposition of the diaphragm to the rib cage
- MV:
-
Mechanical ventilation
- NIV:
-
Non-invasive ventilation
- ICU:
-
Intensive care unit
- R&R:
-
Repeatability and reproducibility
- TEI:
-
Diaphragm thickness at end inspiration
- TEE:
-
Diaphragm thickness at end expiration
- TF:
-
Thickening fraction
- ANOVA:
-
Analysis of variance
References
Kharma N (2013) Dysfunction of the diaphragm: imaging as a diagnostic tool. Curr Opin Pulm Med 19(4):394–398
Wait JL, Nahormek PA, Yost WT, Rochester DP, Rochester P (1989) Diaphragmatic thickness-lung volume relationship in vivo volume relationship in vivo. J Appl Physiol 67:1560–1568
Boussuges A, Gole Y, Blanc P (2009) Diaphragmatic motion studied by M-mode ultrasonography methods, reproducibility, and normal values. Chest 135(2):391–400
Kim SH, Na S, Choi JS, Na SH, Shin S, Koh SO (2010) An evaluation of diaphragmatic movement by M-mode sonography as a predictor of pulmonary dysfunction after upper abdominal surgery. Anesth Analg 110(5):1349–1354
Lerolle N, Guérot E, Dimassi S, Zegdi R, Faisy C, Fagon J-Y, Diehl J-L (2009) Ultrasonographic diagnostic criterion for severe diaphragmatic dysfunction after cardiac surgery. Chest 135(2):401–407
Summerhill EM, El-Sameed YA, Glidden TJ, McCool FD (2008) Monitoring recovery from diaphragm paralysis with ultrasound. Chest 133(3):737–743
Oppersma E, Hatam N, Doorduin J, van der Hoeven JG, Marx G, Goetzenich A, Fritsch S, Heunks LMA, Bruells CS (2017) Functional assessment of the diaphragm by speckle tracking ultrasound during inspiratory loading. J Appl Physiol 123(5):1063–1070
Vivier E, Mekontso Dessap A, Dimassi S, Vargas F, Lyazidi A, Thille AW, Brochard L (2012) Diaphragm ultrasonography to estimate the work of breathing during non-invasive ventilation. Intensiv Care Med 38(5):796–803
Bellani G, Pesenti A (2014) Assessing effort and work of breathing. Curr Opin Crit Care 20(3):352–358
Vivier E, Muller M, Putegnat JB, Steyer J, Barrau S, Boissier F, Bourdin G, Mekontso-Dessap A, Levrat A, Pommier C et al (2019) Inability of diaphragm ultrasound to predict extubation failure a multicenter study. Chest 155(6):1131–1139
Fagley RE, Haney MF, Beraud AS, Comfere T, Kohl BA, Merkel MJ, Pustavoitau A, von Homeyer P, Wagner CE, Wall MH (2015) Critical care basic ultrasound learning goals for American Anesthesiology Critical Care Trainees: recommendations from an expert group. Anesth Analg 120(5):1041–1053
Koo TK, Li MY (2017) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 16(4):346–346
Guillory RK, Gunter OL (2008) Ultrasound in the surgical intensive care unit. Curr Opin Crit Care 14(4):415–422
DeBruin PF, Ueki J, Bush A, Khan Y, Watson A, Pride NB (1997) Diaphragm thickness and inspiratory strength in patients with Duchenne muscular dystrophy. Thorax 52(5):472–475
Hardy F, Walker J, Sawyer T (2009) Sonographic measurement of diaphragm movement in patients with tetraplegia. Spinal Cord 47(11):832–834
Yoshioka Y, Ohwada A, Sekiya M, Takahashi F, Ueki J, Fukuchi Y (2007) Ultrasonographic evaluation of the diaphragm in patients with amyotrophic lateral sclerosis. Respirology 12(2):304–307
DiNino E, Gartman EJ, Sethi JM, McCool FD (2014) Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax 69(5):423–427
Kim WY, Suh HJ, Hong S-B, Koh Y, Lim C-M (2011) Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med 39(12):2627–2630
Blaivas M, Brannam L, Hawkins M, Lyon M, Sriram K (2004) Bedside emergency ultrasonographic diagnosis of diaphragmatic rupture in blunt abdominal trauma. Am J Emerg Med 22(7):601–604
Hassan M, Rizk R, Essam H, Abouelnour A (2017) Validation of equations for pleural effusion volume estimation by ultrasonography. J Ultrasound 20(4):267–271
Subotic DR, Stevic R, Gajic M, Vesovic R (2013) Diaphragm motion and lung function prediction in patients operated for lung cancer—a pilot study on 27 patients. J Cardiothorac Surg 8:213–213
Lloyd T, Tang YM, Benson MD, King S (2006) Diaphragmatic paralysis: the use of M mode ultrasound for diagnosis in adults. Spinal Cord 44(8):505–508
Nason LK, Walker CM, McNeeley MF, Burivong W, Fligner CL, Godwin JD (2012) Imaging of the diaphragm: anatomy and function. Radiographics 32(2):E51–E70
Cohn D, Benditt JO, Eveloff S, McCool FD (1997) Diaphragm thickening during inspiration. J Appl Physiol 83(1):291–296
Harper CJ, Shahgholi L, Cieslak K, Hellyer NJ, Strommen Ja, Boon AJ (2013) Variability in diaphragm motion during normal breathing, assessed with B-mode ultrasound. J Orthop Sports Phys Ther 43(12):927–931
Sæverud HA, Falk RS, Dowrick A, Eriksen M, Aarrestad S, Skjønsberg OH (2019) Measuring diaphragm movement and respiratory frequency using a novel ultrasound device in healthy volunteers. J Ultrasound. https://doi.org/10.1007/s40477-019-00412-2
Goligher EC, Laghi F, Detsky ME, Farias P, Murray A, Brace D, Brochard LJ, Sebastien-Bolz S, Rubenfeld GD, Kavanagh BP et al (2015) Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. Intensiv Care Med 41(4):642–649
Boon AJ, Harper CJ, Ghahfarokhi LS, Strommen Ja, Watson JC, Sorenson EJ (2013) Two-dimensional ultrasound imaging of the diaphragm: quantitative values in normal subjects. Muscle Nerve 47(6):884–889
Ranieri G, Luigi M, Belsito F, Rocco M, Blasi RAD (2015) Propofol sedation reduces contraction and motion of diaphragm in humans: preliminary results. Crit Care 19(Suppl 1):P481–P481
Grams ST, von Saltiél R, Mayer AF, Schivinski CIS, de Nobre SLF, Nóbrega IS, Jacomino MEMLP, Paulin E (2014) Assessment of the reproducibility of the indirect ultrasound method of measuring diaphragm mobility. Clin Physiol Funct Imaging 34(1):18–25
Arbelot C, Dexheimer Neto FL, Gao Y, Brisson H, Chunyao W, Lv J, Valente Barbas CS, Perbet S, Prior Caltabellotta F, Gay F et al (2020) Lung ultrasound in emergency and critically ill patients: number of supervised exams to reach basic competence. Anesthesiology 132(4):899–907
Acknowledgements
CA, FP, IC, SM, and VG had access to all of the data in the study; CA took responsibility for the integrity of the data and the accuracy of data analysis. FP, IC, SM and MB contributed substantially to the study design, data collection, analysis, and interpretation. IC and FP wrote this manuscript. AC, BM, and VG revised and approved the proof, before submission.
Funding
Chiara Adembri was funded by the University of Florence.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
All procedures performed in the present study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethical approval has been obtained for Comitato Etico Area Vasta Toscana Centro with EUDRACT number 2015-004635-12.
Informed consent
Informed consent has been collected from all participants enrolled in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cappellini, I., Picciafuochi, F., Bartolucci, M. et al. Evaluation of diaphragm thickening by diaphragm ultrasonography: a reproducibility and a repeatability study. J Ultrasound 24, 411–416 (2021). https://doi.org/10.1007/s40477-020-00462-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-020-00462-x