Abstract
Background
Assessment of quality of life (QoL) in people living with sleep disorders using questionnaires is necessary to compare intervention benefits. Knowledge of the content and concepts covered by specific QoL instruments is essential to determine which instruments are best suited for conducting economic evaluations of sleep-related interventions.
Objectives
This review aims to identify the QoL instruments that have been applied in economic evaluations of sleep disorder interventions and compare their conceptual overlap and content coverage using the framework of the International Classification of Functioning, Disability and Health (ICF).
Methods
A systematic review of full economic evaluations in sleep published in peer-reviewed journals from conception to 30 May, 2023 was conducted. MEDLINE, PsychInfo, ProQuest, Cochrane, Scopus, CINAHL, Web of Science and Emcare were searched for eligible studies. Studies incorporating either generic or sleep-specific QoL instruments as the primary or secondary measures of effectiveness within a full economic evaluation were included. Quality appraisal against the JBI Critical Appraisal Checklist for Economic Evaluations and EURONHEED checklists and mapping of QoL items to ICF categories were performed by two reviewers, with a third helping settle any potential differences.
Results
Sixteen instruments were identified as having been used in sleep health economic evaluations. The EQ-5D-3L, Epworth Sleepiness Scale, and Insomnia Severity Index were the most widely used, but the latter two are predominantly diagnostic tools and not specifically designed to guide economic evaluations. Other instruments with broader ICF content coverage have been least used, and these include the Sleep Apnea Quality of Life Index, Functional Outcomes of Sleep Questionnaire, 15 Dimensions, Short-Form 6 Dimensions, 12-item Short Form Survey, 36-item Short Form Survey and the GRID Hamilton Rating Scale for Depression.
Conclusions
This study provides an overview of current QoL instruments used in economic evaluations of sleep with respect to their content coverage. A combination of generic and sleep-specific instruments with broader ICF content coverage is recommended for such evaluations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Multiple quality-of-life instruments have been used in economic assessments of sleep interventions, highlighting the importance of understanding their content and covered concepts. |
Of the 16 instruments identified in this review, the Sleep Apnea Quality of Life Index (SAQLI) and the 30-item Functional Outcomes of Sleep Questionnaire (FOSQ-30) along with five non-sleep instruments (15 dimensions [15D], Short Form 6-Dimensions [SF-6D], 12-item Short Form Survey [SF-12], 36-item Short Form Survey [SF-36] and the GRID Hamilton Rating Scale for Depression [GRID-HAMD]) had the broadest content coverage based on the International Classification of Functioning, Disability and Health framework. |
Choosing the appropriate instrument should factor in both quality-of-life coverage and the specific sleep disorder under consideration. For evaluating body functions, the 15D and SAQLI (for obstructive sleep apnoea) or GRID-HAMD (for insomnia) are recommended (cost-effectiveness analysis and cost-utility analysis). When focusing on activities and participation, combinations such as 15D or SF-6D with 10-item FOSQ (FOSQ-10), Epworth Sleepiness Scale or GRID-HAMD are suggested (cost-effectiveness analysis and cost-utility analysis). For utility measurement, especially in guiding resource allocation across various healthcare settings or sleep disorders (cost-utility analysis only), the 15D and SF-6D are recommended choices. |
1 Introduction
Sleep disorders are a major and under-recognised public health issue with a substantial clinical and economic burden on individuals and society [1,2,3,4,5,6,7,8,9,10]. The International Classification of Sleep Disorders version 3 records more than 50 clinically diagnosable sleep disorders [11], with obstructive sleep apnoea (OSA) and insomnia the two most common sleep disorders in the general population [12]. Obstructive sleep apnoea is a sleep-breathing disorder characterised by abnormal breathing reductions (hypopnea) or cessation of airflow (apnoea) during sleep, caused by intermittent partial or complete upper airway obstruction. These lead to blood gas disturbances, cardiovascular system stress, and frequent cortical arousals that fragment sleep. These physiological sequelae can cause pathological sleepiness and negatively impact daytime function, health, and safety [11, 13]. Insomnia is another complex sleep disorder characterised by self-reported difficulties initiating sleep, maintaining sleep, and/or undesired early morning awakenings from sleep with associated daytime impairment [11, 13]. Estimates of the regional and global prevalence of insomnia and OSA vary from 4 to 23% [12, 14,15,16,17] and 9 to 38% [18,19,20], respectively. Sleep disorder impacts vary according to the nature of the underlying sleep problems, but can include pathological daytime sleepiness that increases traffic and workplace accident risks, reduced mental and physical health, productivity, and well-being, and cardiovascular sequelae, including increased risks of hypertension, myocardial infarction, stroke, and premature mortality [20,21,22,23,24,25].
In 2013, annual cost estimates of sleep disorder impacts on communities were estimated at $680 billion across five Organisation for Economic Co-operation and Development countries (USA, Germany, UK, Japan and Canada) [26] and $5.1 billion in Australia [5]. The annual social and economic cost of sleep disorders in Australia was estimated at $35.4 billion in 2021 [27], albeit down from $45.21 billion in 2017 [28]. Sleep tests and sleep disorder interventions (e.g. sleep tests and treatments) are associated with significant healthcare costs, but societal costs of untreated sleep problems are also very high and negative quality-of-life (QoL) impacts are prominent [27].
Given the high prevalence and the significant societal burden potentially attributable to sleep disorders, it is essential to ascertain QoL impacts. Furthermore, healthcare systems worldwide are confronted with perpetually increasing healthcare expenditures, with health spending as a share of gross domestic product across Organisation for Economic Co-operation and Development countries rising from 8.8% in 2019 to 9.7% in 2020 and up by 6% in 2021 [29]. Therefore, robust valid cost-effectiveness evidence is necessary to inform decision making around the allocation of limited healthcare resources among competing health interventions. Accordingly, a comprehensive approach to managing symptomatic or at-risk people with sleep disorders and the evaluation of novel interventions and models of care need to carefully consider how these interventions can improve QoL and clinical outcomes.
The QoL of an individual can be influenced by several factors, including but not limited to the individual’s perspective of the disease and their accompanying coping mechanisms, emotional and psychosocial well-being, independence, material welfare, and the external environment predisposing individuals’ activity and development [30]. To provide a reliable estimate of the cost effectiveness of an intervention that can improve QoL in people with sleep disorders, it is imperative to ascertain the best instrument to comprehensively estimate QoL, particularly in its application within economic evaluations. Instruments to measure QoL can be preference or non-preference based. The former is generated using preferences of the general population sample elicited using one or more valuation methods. For example, a visual analogue scale, time trade-off, discrete choice experiment and standard gamble [31, 32]. Preference-based instruments are widely used in a cost-utility analysis (CUA), a type of economic evaluation where the primary QoL instrument is usually quality-adjusted life-years (QALYs) [32]. Non-preference-based instruments are inappropriate for a CUA because they lack the algorithm for calculating QALYs. However, non-preference-based instruments can still be used in a cost-effectiveness analysis (CEA), where the outcome of relevance can be natural units such as life-years gained, cases detected, events prevented, or indeed non-preference-based QoL [32].
Several instruments have been used to measure QoL within sleep disorders research, including generic instruments such as the EuroQol 5-Dimensions suite of measures (5-level or EQ-5D-5L and 3-level or EQ-5D-3L) and the Short Form surveys (6-Dimension or SF-6D and 36-item or SF-36), and sleep-specific instruments such as the Epworth Sleepiness Scale (ESS) to estimate perceived sleepiness in different daily living situations and the Insomnia Severity Index (ISI) to estimate the likelihood of clinical insomnia and its daytime impacts [33, 34]. However, there is still debate about the most appropriate instruments to measure QoL, specifically in sleep health research [33, 35]. Different QoL instruments can lead to varying conclusions about an intervention conducted in the same population [35]. Instruments such as the ESS and ISI are also predominantly used as diagnostic tools and not strictly QoL instruments. Further, sleep (and circadian) factors strongly influence many aspects of daily mental and physical performance and well-being, thus broad QoL impacts from sleep disorders should be anticipated [36,37,38,39,40,41]. Hence, it is vital to establish an appropriately sensitive, specific, reproducible, and standardised approach to measure QoL as an outcome of treatment that can be applied widely within the economic evaluation framework. To achieve this, it is crucial to clearly differentiate between two key concepts: sensitivity to changes in specific diseases and sensitivity to changes in overall QoL and health-related QoL (HRQoL). While the former is primarily essential for evaluating the clinical effectiveness of treatments for sleep disorders, the latter is required for economic analyses such as CEAs and CUAs. This distinction underscores the need for careful consideration when selecting QoL instruments for economic evaluations in sleep research. The chosen instruments must be sensitive to changes in both specific sleep disorder symptoms and overall QoL and HRQoL to provide valuable insights for both clinical and economic decision making. A preliminary search of PROSPERO, MEDLINE and the Cochrane Database of Systematic Reviews was performed, and no current or ongoing systematic reviews on the topic were identified.
Therefore, this paper sought to identify QoL instruments that have been used in economic evaluations of interventions used within sleep health studies in various contexts. It outlines the methods and results that identify instruments used to measure QoL in individuals suspected of having or suffering from sleep disorders within the economic evaluation framework. The paper also compares the domains and dimensions of these instruments in terms of their content coverage [42] and the conceptual overlap based on the International Classification of Functioning, Disability and Health (ICF) Core Set framework [43]. The ICF was selected as it is the most extensive attempt to classify health concepts within a biopsychosocial model of health, function and disability [43]. The findings will provide evidence-based information for researchers to determine the most suitable outcome measurement approach for the economic evaluation of sleep disorders.
1.1 Review Objectives
We aimed to (1) identify the contexts and populations in which QoL instruments have been used in the published economic evaluation literature in sleep health research and (2) to compare the content of QoL instruments by linking them to meaningful concepts within the ICF framework [43].
2 Methods
The protocol for this review was registered with the International Prospective Register of Systematic Reviews (PROSPERO), registration number CRD42023399598 and International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY), registration number INPLASY202350068. This review followed the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2020 guidelines for systematic reviews [44, 45]. The PRISMA checklists for the main text and abstracts are provided in Appendices 1 and 2 of the Electronic Supplementary Material (ESM).
2.1 Search Strategy
An initial search was limited to MEDLINE, the National Health Service Economic Evaluation Database and the Cost-Effectiveness Analysis Registry to identify articles on the topic. The text words used in the titles and abstracts and the index terms used to describe the articles were used to develop a full search strategy in MEDLINE, PsychInfo, ProQuest, Cochrane, Scopus, CINAHL, Web of Science and Emcare (Appendix 3 of the ESM). The search strategy was adapted for each database and/or information source and was last used on 30 May, 2023.
2.2 Study Selection
Studies that met the following inclusion criteria were considered: (1) measured QoL and/or HRQoL as the primary or secondary measure of effectiveness in the economic evaluation. Health-related QoL was defined as any description of the physical, role function, social, and psychological aspects of well-being and function [46]; (2) used a preference-based generic and/or preference or non-preference-based sleep-specific QoL instrument; (3) study design was a full economic evaluation applied in sleep health research [32], i.e. a CUA, CEA, cost-benefit analysis, cost-minimisation analysis, or cost-consequence analysis; and (4) published in peer-reviewed journals in the English language from conception to 30 May, 2023.
Studies were excluded if: (1) they were not related to a common primary sleep disorder (e.g. insomnia, OSA, and restless leg syndrome); (2) QoL/HRQoL was measured using an instrument specifically designed for the study; or (3) they were published as dissertations, commentaries, conference papers or review articles or studies for which the full-text article could not be obtained.
2.3 Article Screening
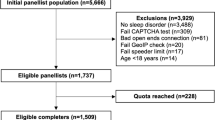
All citations identified during the search were imported into EndNote X9 (Clarivate Analytics, Philadelphia, PA, USA) and the Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI SUMARI) [47]. The reference lists of all included sources of evidence were screened for additional studies. Titles and abstracts, followed by full texts of eligible studies, were screened by two independent reviewers for assessment against inclusion criteria. Reasons for excluding full-text papers that did not meet the inclusion criteria were recorded and reported. Any potential disagreement between reviewers at each stage was resolved through discussion or with a third reviewer. The search and inclusion process results were reported in full in the final systematic review and presented in a PRISMA flow diagram [48] (Fig. 1).
2.4 Assessment of Methodological Quality
Two independent reviewers assessed the quality of eligible studies against the JBI Critical Appraisal Checklist for Economic Evaluation [49], a standardised critical appraisal instrument (Appendix 4 of the ESM). As economic evaluation studies often employ various cost perspectives and report distinctive health economic measures in different contexts and regions, the European Network of Health Economic Evaluation Databases (EURONHEED) checklist was used to assess further generalisability and transferability of included studies [50] (Appendix 5 of the ESM). The critical appraisal results were reported in a narrative format and tabulated.
2.5 Data Extraction and Synthesis
Data were extracted from studies using a standardised data extraction tool. Extracted data included specific details about the intervention/s and comparator/s examined, study population/participants and context, study methods, results for resource use, and cost and cost-effectiveness measures. The findings were presented in a narrative format, including tables and figures where appropriate.
2.6 Instrument Conceptual Overlap and Content Coverage
The conceptual overlap between these instruments and their content coverage was assessed by comparison of their dimensions using the ICF Core Set framework [43] (Appendices 6 and 7 of the ESM). The ICF has been linked to many patient-reported outcome development efforts, for example, the Patient-Reported Outcomes Measurement Information System (PROMIS) [51, 52]. In this exercise, conducted by BK and TJW (and AN as the tie-breaker), instrument dimensions were divided into three ICF domains: ‘body functions and structures’ (measuring impairments to [i] physiological and psychological functions of body systems and [ii] anatomical parts of the body such as limbs), ‘activities and participation’ (referring to constructs that cover the full range of life areas such as execution of tasks or actions and involvement in life situations) and ‘environmental factors’ (referring to the physical, social, and attitudinal environment in which people live and conduct their lives, which can be either barriers or facilitators to their function) [43]. Each domain was also broken down into chapters and collapsed into categories. Content coverage was expressed as a percentage of the number of ICF chapters mapped onto by each QoL instrument divided by the potential total number of ICF chapters available.
3 Results
3.1 Study Inclusion
Figure 1 displays the study selection based on the PRISMA guidelines [48] and shows that from 7990 database citations and 15 additional references initially identified, 1900 duplicates and 5551 titles not meeting the criteria were excluded, leaving 554 (539 + 15) full-text articles for a further eligibility assessment. Of the 554, only 57 articles met the criteria as full economic evaluations, measuring QoL and/or HRQoL in sleep health research for the final analysis.
3.2 Methodological Quality
The methodological quality for all included studies was considered good to excellent when assessed against the JBI Critical Appraisal Checklist For Economic Evaluation [49] and EURONHEED [50] (Appendices 4 and 5 of the ESM). The average score for all included studies was 89% against the EURONHEED [50] checklist.
3.3 Characteristics of Included Studies
A summary of the characteristics of the 57 included studies is presented in Table 1.
3.3.1 Study Design
The study designs for OSA interventions varied; 30 were CUAs [53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82], four were CEAs [83,84,85,86] and five were cost minimisation analyses [87,88,89,90,91]. In assessments of insomnia interventions, 16 studies were CUAs [35, 92,93,94,95,96,97,98,99,100,101,102], one reported a CEA [101], and another combined a CEA and a cost-benefit analysis [96]. Economic evaluations were most frequently conducted alongside a randomised controlled trial (n = 30) [35, 54, 55, 57,58,59,60,61,62, 66, 82,83,84,85,86,87,88,89,90,91,92,93, 95,96,97, 99,100,101,102,103]. One retrospective case-crossover [64] and one cohort study [63] ran economic evaluations concurrently. Twenty-five studies were model based, 14 using a Markov model [53, 56, 65, 67,68,69,70,71, 73, 75, 77, 78, 80, 98], five using a decision-tree model [74, 104,105,106,107], one using both Markov and decision-tree models [76], one using a semi-Markov model [79] and one using a decision analytic model [81]. Additionally, two studies used randomised controlled trial-based modelling [94, 108], and one used a case-control-based model [72].
3.3.2 Population
Participants’ numbers ranged from 37 [92] to 830 [94], with model-based studies simulating up to 100,000 participants [98]. Most studies had a mean age of 50 years, but some focussed on distinct age groups: four on those aged 65 years and older [61, 62, 105, 106], one on adolescents aged 12–19 years [95] and one on premature infants [81]. Recruitment strategies varied: in insomnia studies, some involved clinically diagnosed patients, others included those with symptoms but no diagnosis, a few focused on self-referred patients for therapy workshops and one targeted undiagnosed individuals seeking treatment [35, 92, 93, 96,97,98,99,100,101,102,103,104,105,106,107,108]. Two insomnia studies involved populations with comorbid conditions, including depression and schizophrenia [92, 97]. In OSA studies, some included clinically confirmed OSA cases, while others recruited newly diagnosed or suspected cases and one focussed on at-risk infants without a formal diagnosis [54,55,56,57, 59, 61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85, 87, 89,90,91, 109].
3.3.3 Geographical Location, Setting and Timeframe
The included studies were conducted mainly in the UK (n = 12) [35, 60,61,62, 65, 66, 70,71,72,73, 93, 97], USA (n = 11) [74, 75, 78, 79, 90, 94, 98, 100, 106, 108, 110] and Spain (n = 10) [53,54,55,56,57,58, 64, 82, 83, 89]. Japan [76, 92, 104, 105] and Canada [68, 77, 80, 101] each had four studies, The Netherlands had three studies [59, 95, 99], and Germany [96, 102] and France [69, 85] had two studies each. Single studies were conducted in Colombia [67], New Zealand [107], South Korea [103], Finland [63], Australia [84] and Hong Kong [91]. Most studies (n = 28) were conducted in clinical settings, 25 in community settings, and one in a workplace environment. The economic evaluations’ time horizons ranged from 1 day [81] to a lifetime [65]. Studies were published between 2003 [56] and 2023 [67], as shown in Table 1.
3.4 QoL Instruments
3.4.1 Frequency of Use
Of the 57 studies included (Table 1), 32 had one type of QoL apiece: 27 generic [53, 56, 59, 63,64,65, 67,68,69, 71, 72, 74,75,76,77, 79,80,81, 93, 94, 97, 98, 103,104,105, 108, 110], four sleep specific [84, 87, 96, 101], and one depression specific [92]). Thirteen studies used a combination of one generic and one sleep-specific instrument [35, 54, 55, 57, 58, 82, 83, 85, 88, 90, 95, 99, 102], nine used two generic instruments each [60,61,62, 66, 70, 73, 78, 106, 107], two had two sleep-specific instruments [89, 91], one utilised one generic and one depression-specific instrument [110], and one used a combination of a generic, a sleep-specific and osteoarthritis-specific tool [100]. Table 2 summarises the frequency of use of specific instruments to measure QoL.
A total of 16 different QoL instruments were used in the 57 economic evaluations. The EQ-5D-3L (n = 24) and the ESS (n = 10) were the most common generic and sleep-specific QoL instruments used, respectively. In the OSA studies, 11 instruments were used. The EQ-5D-3L was the most frequently used (n = 21) followed by ESS (n = 10), SF-6D (n = 6) and EQ-5D-5L (n = 5). Unspecified EQ-5D and SF-36 were used in three studies, while the FOSQ was employed in two studies. The Sleep Apnea Quality of Life Index (SAQLI), Quebec Sleep Questionnaire (QSQ), 15 dimensions quality of life (15D), Health Utilities Index mark II (HUI-2) and the Nottingham Health Profile (NHP) were each used in one study. Fewer instruments (n = 10) were utilised in insomnia studies: the ISI (n = 6), SF-36, EQ-5D-5L (n = 5 each), EQ-5D-3L, SF-6D (n = 3 each) and GRID-HAMD (n = 2) were most common. The Holland Sleep Disorder Questionnaire (HSDQ), unspecified EQ-5D, the short-form 12 dimensions (SF-12), and the Western Ontario and McMaster Universities Arthritis Index (WOMAC) were each used in single insomnia studies. Table 2 shows that the most frequently used instruments had between five and eight questions that took between 2 and 5 minutes to complete. The only exception was the SF-36, which has 36 questions and takes between 10 and 15 minutes to complete.
3.4.2 Descriptions of QoL Instruments
The EQ-5D-3L, EQ-5D-5L, SF-6D, 15D, and HUI3 are preference-based QoL instruments yielding utility scores (where higher scores denote better QoL), subsequently employed in calculating QALYs [31]. The EQ-5D-3L and EQ-5D-5L both measure five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. They are widely used in economic evaluations and generate utility scores that range from − 0.59 to 1 [31]. The SF-6D measures eight dimensions: physical functioning, role limitations due to physical health problems, role limitations due to mental health problems, social functioning, pain, mental health, vitality and general health perceptions. SF-6D utility scores range from 0.301 to 1 [31]. The 15D has 15 dimensions: mobility, vision, hearing, breathing, sleeping, eating, speech, elimination, usual activities, mental function, discomfort and symptoms, depression, distress, vitality, and sexual activity. Utility scores for the instrument range from 0.11 to 1 [31, 114]. The HUI3 comprises eight domains: vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain. Utility scores for the instrument range from − 0.36 to 1 [31].
The ESS measures the propensity to fall asleep during eight daily activities (sitting and reading, watching television, sitting inactive in a public place, as a passenger in a car for an hour without a break, lying down to rest in the afternoon, sitting and talking to someone, sitting quietly after lunch without alcohol, and sitting in a car, while stopped for a few minutes in traffic) [115]. Summary scores can range from 0 to 24 [116, 117]. The ISI is a widely used 7-item tool for quantifying perceived insomnia severity and its potential daytime impacts relating to sleep-onset difficulty, sleep maintenance difficulty, early morning awakenings, sleep dissatisfaction and interference with work, social and mood functioning [118]. It produces summary scores that range from 0 to 28 [119]. The FOSQ-30 is a widely used instrument constructed to assess the impact of excessive somnolence on adult functional status. It examines five domains: activity levels, vigilance, intimacy and sexual relationships, productivity, and social outcomes. Summary scores ranging from 5 to 20 can be calculated [119]. The SAQLI assesses four QoL domains linked to sleep apnoea: daily functionality, social interactions, emotional well-being and symptoms, with an additional domain, treatment-related symptoms, specifically designed for individuals undergoing a therapeutic intervention. [123]. Summary scores that range from 1 to 7 can be calculated [128]. The QSQ assesses HRQoL in patients with OSA and evaluates the impact of apnoea on five domains, namely hypersomnolence, daytime symptoms, night-time symptoms, emotions, and social interactions [116]. Summary scores that range from 1 to 7 can be calculated [119]. The HSDQ is a 32-item used to screen for six potential sleep disorders: insomnia, parasomnia, circadian rhythm sleep disorder, hypersomnia, restless legs/periodic limb movement disorder, and sleep-related breathing disorder. Averaged scores that range from 1 to 5 can be calculated [129].
The WOMAC is an instrument widely used in evaluating osteoarthritis [130]. Its 24 items can be divided into three subscales (pain, stiffness, and physical function) with total scores that range from 0 to 96 [131]. The 17-item GRID-HAMD is a depression rating scale, which also captures insomnia QoL constructs and enables a rater to measure the intensity and frequency of QoL constructs [132]. Summary scores that range from 0 to 52 can be calculated [132]. Higher scores for the FOSQ-30, SAQLI, and QSQ indicated better outcomes, whereas the converse was true for the ESS, ISI, HSDQ, WOMAC and GRID-HAMD.
3.5 Instrument Conceptual Overlap and Content Coverage
Table 3 shows the distribution of sleep-specific and generic instruments across the major ICF categories and level 2 chapters of the ICF, summarised further in Appendices 6 and 7 of the ESM. One hundred and eighty-seven instrument items/dimensions were compared and matched to 17 ICF chapters and 80 level-two categories. There was 94% agreement between the two linkers (BK and TJW) for 176 items/dimensions (127 sleep specific and 49 generic). Linkages of the rest of the items (8: 6 sleep specific and 5 generic) were determined through a structured discussion with a third expert (AN).
Table 3 shows there was a conceptual overlap between the sleep and generic QoL instruments in terms of their coverage of the ICF’s ‘Body Functions’ and ‘Activities and Participation’ domains. For the body functions domain, the most overlap was in the ‘b1—mental functions’ chapter, onto which at least one item/dimension from all instruments was mapped. However, more sleep items (71–100% of the total number of items in an instrument) than generic dimensions (20–50% of the total number of dimensions in an instrument) were linked to this chapter. The chapters with the least overlap were ‘b3—voice and speech functions’, ‘b4—functions of the cardiovascular, haematological, immunological and respiratory systems’, ‘b5—functions of the digestive, metabolic and endocrine systems’, and ‘d3—communication’, i.e. only covered by three sleep instruments and one generic instrument. Only the SAQLI was linked to all six ‘Body Functions’ chapters. All items from one sleep instrument (ESS) solely matched onto the ‘Mental Function’ chapter. All generic instruments were linked to up to three ‘Body Functions’ chapters (‘b1—mental functions’, ‘b2—sensory functions and pain’ and ‘b6—genitourinary and reproductive functions’) except for HUI-2, which was additionally linked to ‘b3—voice and speech functions’ and the 15D, which mapped onto all body function chapters.
There seemed to have been a more widespread overlap between the sleep and generic instruments in the ‘Activities and Participation’ domain. However, no single instrument covered all nine chapters of this domain. The chapters in this domain with the most overlap between the instruments were ‘d2—general tasks and demands’ and ‘d7—interpersonal interactions and relationships’ (each covered by seven and four of the sleep and generic instruments, respectively). The chapters with the least overlap were ‘d1—learning and applying knowledge’, which was covered by only one sleep instrument (ESS) and ‘d3—communication’, which was only covered by three sleep instruments. Amongst the sleep and depression-related instruments, the FOSQ-30, ESS, SAQLI, and GRID-HAMD covered the most chapters of the ‘activities and participation’ domain (i.e. eight for the FOSQ-30 and seven for the other instruments). Amongst the generic instruments, the SF-6D, 15D, and SF-36/SF-12 covered the most (seven) of this domain’s chapters. The EQ-5D and NHP, respectively, covered six and five chapters of the ‘activities and participation’ domain.
Considered separately, there was a more apparent overlap amongst generic instruments (100% overlap for six ICF chapters; two for the ‘body functions’ domain and four for ‘activities and participation') than amongst the sleep instruments (100% overlap for only one ICF chapter from the ‘body functions’ domain). Consequently, there seemed to have been more diversity in the concepts covered by the sleep-specific instruments than in the generic instruments.
In terms of the extent of concepts covered, the instruments with the broadest coverage were the SAQLI linked to 76% of all ICF chapters (100%, 67%, and 50% of all ‘body functions’, ‘activities and participation’, and ‘environmental factors’ chapters, respectively), 15D linked to 76% of all ICF chapters (100% and 78% of all ‘body functions’ and ‘activities and participation’ chapters, respectively) and the GRID-HAMD mapped to 71% of the ICF chapters (83% and 78% of all ‘body functions’ and ‘activities and participation’ chapters, respectively).
4 Discussion
This review found an ample choice of instruments available to evaluate the various aspects of QoL among sleep disorder cohorts in economic evaluations. Whilst QoL is multi-dimensional, instruments in sleep disorder cohorts must capture domains important for this cohort. Reimer and Flemons argue for using broad-based instruments in study cohorts to cover concepts that include physical, mental, and social function, the burden of symptoms and an overall sense of well-being [133]. Instruments with broader coverage of QoL concepts have also been recommended in the sleep literature, given that sleep and circadian factors are strongly correlated with broad concepts of daily mental and physical performance and well-being [36,37,38,39]. Our review has shown that nearly 45% of economic evaluations of sleep disorder interventions have a mix of generic and sleep-specific instruments, perhaps in recognition that neither type of instrument may be sufficiently comprehensive to cover the breadth of potential sleep-related QoL constructs. However, the instruments with the most comprehensive coverage of sleep-related constructs were the SAQLI and FOSQ-30 (amongst sleep instruments) and the 15D, SF-6D, SF-36/SF-12, and GRID-HAMD (amongst non-sleep instruments).
While the comprehensiveness of an instrument is a key consideration when selecting an instrument, attention must also be paid to other instrument attributes, including acceptable measurement properties (e.g. ceiling effects, specificity, sensitivity, validity, reliability, and responsiveness), parsimony, ease of completion and scoring, and the potential to provide helpful clinical data [134]. Overall, the most frequently used generic QoL instruments were EQ-5D-3L (n = 17) and SF-36 (n = 11). Several attributes may account for the popularity of the EQ-5D-3L, including its translations, scoring algorithms adapted to several cultures and countries, absence of license fees for non-commercial usage, and its recommended use by the UK National Institute for Health and Care Excellence in economic evaluations [135]. Further, the brevity and ease of administration of the EQ-5D-3L, which uses 3-level Likert scales, delivers a practical advantage with respect to its burden on respondents compared with other instruments with more dimensions. Nevertheless, it must be considered that the EQ-5D-3L has a higher ceiling effect than other generic instruments, such as the SF-36, SF-6D [111, 112], 15D [136], and NHP, with the 15D and SF-6D showing the lowest effect [137, 138]. However, it should be noted that the EQ-5D-5L, which consists of a 5-level Likert scale used in three studies [54, 82, 97], has been shown to reduce this ceiling effect [139, 140]. In the context of sleep health, several studies suggest that the EQ-5D is less sensitive to intervention effects on health status when compared with alternative generic instruments such as the SF-36, SF-12, 15D, HUI-2, or SF-6D, which better detect improvements in line with those indicated by condition-specific clinical metrics [62, 114, 141]. The downside to the SF-36, SF-12, 15D, HUI-2, and SF-6D is that they are relatively longer instruments and may, therefore, lead to a higher respondent burden. Indeed, participant burden and related feasibility impacts are important considerations when selecting an evaluation tool, particularly where health economic outcomes are incorporated as secondary outcomes in research studies. We did not find evidence of the performance of non-sleep instruments in sleep cohorts regarding other measurement properties in the literature, such as sensitivity, validity, reliability, and responsiveness [142].
Multiple studies [35, 53,54,55, 57, 58, 60,61,62, 64, 66, 82,83,84,85, 87,88,89,90,91,92,93, 96, 98,99,100,101,102, 143] identified in this review used sleep-specific instruments. Of all sleep-specific instruments, the ESS (n = 9) was the tool most commonly reported in the economic analyses that we identified, followed by the ISI (n = 6) and FOSQ-30 (n = 2).
The popularity of the ESS is likely driven by its simplicity and brevity in measuring the propensity to fall asleep during daily activities [115]. It also forms part of the diagnostic criteria or assessment for further testing or treatment eligibility and may lead to floor effects when used on non-sleepy people with OSA. Poor test-retest reliability in short time intervals and sensitivity and specificity in interventions in moderate-to-severe OSA cohorts have been noted and must be considered when interpreting the ESS as a potential indicator of QoL [116, 117]. It also had a lower coverage of QoL concepts than the FOSQ-30.
The ISI is a widely accepted and valid tool to quantify perceived insomnia severity and its potential daytime impacts by capturing QoL domains relevant to those with insomnia. This includes a domain that assesses distress caused by sleep disturbance, which impacts QoL [118]. The ISI has shown sensitivity to treatment response [120, 121]. However, it has the lowest coverage of QoL concepts among all sleep instruments.
The FOSQ is more strongly correlated with the ESS than the SAQLI, making it more effective for the evaluation of the impact of sleepiness on QoL. It was also more responsive to continuous positive airway pressure therapy for OSA than the SAQLI [123]. The length of the FOSQ (35 items) brings into question its utility for clinical practice, and large-scale studies may be difficult when treatment progression needs to be monitored [124]. Alternatively, a more recently developed and validated 10-item FOSQ (FOSQ-10) [124] would be more convenient in practice than its predecessor. The FOSQ-10, however, has a lower coverage of QoL concepts than the SAQLI or its 35-item version.
The SAQLI is a sleep-specific instrument for patients with OSA that takes a broad scope on QoL. Notably, its ‘emotional functioning’ domain effectively measures mental health-related aspects of QoL [123], a relevant consideration in patients with sleep disorders. Another domain, tailored specifically for treatment-related symptoms, was created for individuals undergoing therapeutic interventions. This addition enhances its utility in clinical settings, enabling the tracking of symptom improvements and the monitoring of treatment side effects. It has the most comprehensive coverage of QoL concepts of all sleep-specific instruments. The drawbacks of using the SAQLI is the requirement of a trained interviewer to administer the questionnaire and the complex scoring algorithm [119].
The 17-item GRID-HAMD had the second broadest coverage of sleep-associated QoL concepts of all sleep-related instruments and should therefore be considered in economic evaluations of insomnia interventions. However, its requirement for trained individuals familiar with mood assessments in depressed populations limits its widespread use [132]. The rest of the non-generic instruments (QSQ, HSDQ, and WOMAC) had a low coverage of QoL concepts and would, therefore, not be appropriate for economic evaluations.
Generic preference-based instruments should be considered for use in economic evaluations of sleep disorders, where it is essential to make standardised comparisons across disease areas within a CUA. However, given that some of the measurement properties of non-sleep QoL instruments, when used in sleep populations, have yet to be reported or demonstrated, we recommend a combination approach of generic (within CUAs) and sleep-specific instruments (within CEAs) in economic evaluations of sleep disorder interventions. The choice of the instrument used should consider QoL coverage of sleep-related constructs and the sleep disorder being addressed. If the primary interest is to evaluate concepts relating to body functions, the 15D and SAQLI (for OSA) or GRID-HAMD (for insomnia) should be considered (CEA and CUA). If the goal is to evaluate concepts relating to activities and participation, either the 15D or SF-6D could be paired with the FOSQ-10, ESS, or GRID-HAMD (CEAs and CUAs). For utility measurement, especially in guiding resource allocation across various healthcare settings or sleep disorders (CUA only), the 15D and SF-6D are recommended choices. Given the prominence of certain instruments, such as the ESS and EQ-5D suite of instruments, in sleep-related economic evaluations, transitioning to alternative instruments demands a comprehensive evidence-based approach. Initially, a stronger case for alternative instruments’ superiority in psychometric properties, adaptability to change and alignment with research objectives must be established through robust evidence. A shift to alternative instruments also requires training researchers and practitioners in applying, scoring and comprehending these alternative tools. Accessibility plays a pivotal role; ensuring affordability and availability of new instruments through open-source models or cost-effective licensing options can widen their adoption. Finally, efforts are needed to create preference weights for sleep-specific tools to guide their utilisation in CUAs to expand their utility in healthcare assessments.
A key area for future research should be to investigate whether current QoL instruments employed in an economic evaluation of sleep disorders adequately capture all dimensions relevant to people with such conditions rather than dimensions presumed to be relevant based on expert opinion [144]. Patient-centred perspectives should also concurrently compare the measurement properties of both sleep and non-sleep instruments in sleep populations most relevant to and negatively impacted by the QoL effects of poor sleep. Future research should also be dedicated to developing a sleep-specific preference-based instrument enabling a QALY calculation to facilitate the economic evaluation of sleep health technologies.
A limitation of this review was that, because of heterogeneity and a lack of data from the studies included, a meta-analysis was not conducted on some studies that assessed OSA interventions and all studies that evaluated insomnia interventions. There were also no economic analysis data on interventions for sleep disorders other than insomnia and OSA (e.g. narcolepsy, restless legs syndrome, central sleep apnoea and circadian rhythm disturbance) or on comorbid insomnia and OSA.
5 Conclusions
Given the breadth and variability of tools used to evaluate QoL impacts in sleep disorders, there is a clear need for a preference-based ‘gold standard’ instrument to support economic evaluations of sleep health interventions that includes domains considered most important to people with sleep disorders. Inadequacies within existing generic and sleep-specific QoL instruments, when used alone, support the conclusion that a QoL assessment within sleep health economic evaluations is best captured using a combination of the two.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
References
Deloitte Access Economics. Re-awakening Australia: the economic cost of sleep disorders in Australia, 2010. Report: Sleep Health Foundation. 2011.
Sivertsen B, Björnsdóttir E, Øverland S, Bjorvatn B, Salo P. The joint contribution of insomnia and obstructive sleep apnoea on sickness absence. J Sleep Res. 2013;22(2):223–30.
Deloitte Access Economics. Asleep on the job: costs of inadequate sleep in Australia. Report: Sleep Health Foundation. 2017.
AlGhanim N, Comondore VR, Fleetham J, Marra CA, Ayas NT. The economic impact of obstructive sleep apnea. Lung. 2008;186(1):7–12.
Hillman DR, Lack LC. Public health implications of sleep loss: the community burden. Med J Aust. 2013;199(8):S7-10.
Bin YS, Marshall NS, Glozier N. The burden of insomnia on individual function and healthcare consumption in Australia. Aust N Z J Public Health. 2012;36(5):462–8.
Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. 2009;32(1):55–64.
Botteman M. Health economics of insomnia therapy: implications for policy. Sleep Med. 2009;10(Suppl. 1):S22–5.
Wickwire EM, Shaya FT, Scharf SM. Health economics of insomnia treatments: the return on investment for a good night’s sleep. Sleep Med Rev. 2016;30:72–82.
Glick DR, Abariga SA, Thomas I, Shipper AG, Gunia BC, Grandner MA, et al. Economic impact of insufficient and disturbed sleep in the workplace. Pharmacoeconomics. 2023;41(7):771–85.
Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–94.
Ohayon MM. Epidemiological overview of sleep disorders in the general population. Sleep Med Res. 2011;2(1):1–9.
Thorpy MJ. Classification of sleep disorders. Neurotherapeutics. 2012;9(4):687–701.
National Institutes of Health. National Institutes of Health State of the Science Conference statement on manifestations and management of chronic insomnia in adults, June 13–15, 2005. Sleep. 2005;28(9):1049–57.
Chung KF, Yeung WF, Ho FY, Yung KP, Yu YM, Kwok CW. Cross-cultural and comparative epidemiology of insomnia: the Diagnostic and Statistical Manual (DSM), International Classification of Diseases (ICD) and International Classification of Sleep Disorders (ICSD). Sleep Med. 2015;16(4):477–82.
Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125–33.
Appleton SL, Reynolds AC, Gill TK, Melaku YA, Adams RJ. Insomnia prevalence varies with symptom criteria used with implications for epidemiological studies: role of anthropometrics, sleep habit, and comorbidities. Nat Sci Sleep. 2022;14:775–90.
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81.
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–5.
Lechat B, Naik G, Reynolds A, Aishah A, Scott H, Loffler KA, et al. Multinight prevalence, variability, and diagnostic misclassification of obstructive sleep apnea. Am J Respir Crit Care Med. 2022;205(5):563–9.
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353(19):2034–41.
Lechat B, Appleton S, Melaku YA, Hansen K, McEvoy RD, Adams R, et al. The association of co-morbid insomnia and sleep apnea with prevalent cardiovascular disease and incident cardiovascular events. J Sleep Res. 2022;31(5): e13563.
Krishnan S, Chai-Coetzer CL, Grivell N, Lovato N, Mukherjee S, Vakulin A, et al. Comorbidities and quality of life in Australian men and women with diagnosed and undiagnosed high-risk obstructive sleep apnea. J Clin Sleep Med. 2022;18(7):1757–67.
Lechat B, Appleton S, Melaku YA, Hansen K, McEvoy RD, Adams R, et al. Comorbid insomnia and sleep apnoea is associated with all-cause mortality. Eur Respir J. 2022;60(1):2101958.
Terán-Santos J, Jiménez-Gómez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. Cooperative Group Burgos-Santander. N Engl J Med. 1999;340(11):847–51.
Hafner M, Stepanek M, Taylor J, Troxel WM, van Stolk C. Why sleep matters: the economic costs of insufficient sleep: a cross-country comparative analysis. Rand Health Q. 2017;6(4):11.
Streatfeild J, Smith J, Mansfield D, Pezzullo L, Hillman D. The social and economic cost of sleep disorders. Sleep. 2021. https://doi.org/10.1093/sleep/zsab132.
Hillman D, Mitchell S, Streatfeild J, Burns C, Bruck D, Pezzullo L. The economic cost of inadequate sleep. Sleep. 2018. https://doi.org/10.1093/sleep/zsy083.
Organisation for Economic Co-operation and Development. Health expenditure. 2022. Available from: https://www.oecd.org/els/health-systems/health-expenditure.htm. [Accessed 11 Apr 2023].
Felce D, Perry J. Quality of life: its definition and measurement. Res Dev Disabil. 1995;16(1):51–74.
Brazier J, Ratcliffe J, Saloman J, Tsuchiya A. Measuring and valuing health benefits for economic evaluation. 2nd ed. Oxford: Oxford University Press; 2017.
Drummond M, Sculphe M, Torrance G, O’Brien B, Stoddart G. Methods for the economic evaluation of health care programs. New York: Oxford University Press; 2015.
Natsky AN, Vakulin A, Chai-Coetzer CL, Lack L, McEvoy RD, Lovato N, et al. Economic evaluation of cognitive behavioural therapy for insomnia (CBT-I) for improving health outcomes in adult populations: a systematic review. Sleep Med Rev. 2020;54: 101351.
Kaambwa B, Mpundu-Kaambwa C, Adams R, Appleton S, Martin S, Wittert G. Suitability of the Epworth Sleepiness Scale (ESS) for economic evaluation: an aasessment of its convergent and discriminant validity. Behav Sleep Med. 2018;16(5):448–70.
Bonin EM, Beecham J, Swift N, Raikundalia S, Brown JS. Psycho-educational CBT-Insomnia workshops in the community: a cost-effectiveness analysis alongside a randomised controlled trial. Behav Res Ther. 2014;55:40–7.
Hofmeister D, Schulte T, Mehnert-Theuerkauf A, Geue K, Zenger M, Esser P, et al. The association between sleep problems and general quality of life in cancer patients and in the general population. Front Psychol. 2022;13: 960029.
Flemons WW, Reimer MA. Development of a disease-specific health-related quality of life questionnaire for sleep apnea. Am J Respir Crit Care Med. 1998;158(2):494–503.
Uchmanowicz I, Markiewicz K, Uchmanowicz B, Kołtuniuk A, Rosińczuk J. The relationship between sleep disturbances and quality of life in elderly patients with hypertension. Clin Interv Aging. 2019;14:155–65.
Lee S, Kim JH, Chung JH. The association between sleep quality and quality of life: a population-based study. Sleep Med. 2021;84:121–6.
Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117–26.
Belenky G, Wesensten NJ, Thorne DR, Thomas ML, Sing HC, Redmond DP, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12(1):1–12.
Messick S. Test validity and the ethics of assessment. Am Psychol. 1980;35(11):1012–27.
World Health Organization. Towards a common language for functioning, disability and health ICF: the international classification of functioning, disability and health. Geneva: World Health Organization; 2002.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1–9.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
de Wit M, Hajos T. Health-related quality of life. In: Gellman MD, Turner JR, editors. Encyclopedia of behavioral medicine. New York: Springer; 2013. p. 929–31.
Munn Z, Aromataris E, Tufanaru C, Stern C, Porritt K, Farrow J, et al. The development of software to support multiple systematic review types: the Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI SUMARI). Int J Evid Based Healthc. 2019;17(1):36–43.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178–89.
The Joanna Briggs Institute. The Joanna Briggs Institute reviewers’ manual 2014. Adelaide: Joanna Briggs Institute; 2014.
Nixon J, Rice S, Drummond M, Boulenger S, Ulmann P, de Pouvourville G. Guidelines for completing the EURONHEED transferability information checklists. Eur J Health Econ. 2009;10(2):157–65.
Tucker CA, Cieza A, Riley AW, Stucki G, Lai JS, Bedirhan Ustun T, et al. Concept analysis of the patient reported outcomes measurement information system (PROMIS((R))) and the international classification of functioning, disability and health (ICF). Qual Life Res. 2014;23(6):1677–86.
Tucker CA, Escorpizo R, Cieza A, Lai JS, Stucki G, Ustun TB, et al. Mapping the content of the patient-reported outcomes measurement information system (PROMIS(R)) using the International Classification of Functioning, Health and Disability. Qual Life Res. 2014;23(9):2431–8.
Turino C, de Batlle J, Woehrle H, Mayoral A, Castro-Grattoni AL, Gómez S, et al. Management of continuous positive airway pressure treatment compliance using telemonitoring in obstructive sleep apnoea. Eur Respir J. 2017;49(2):1601128.
Sánchez-Quiroga M, Corral J, Gómez-de-Terreros FJ, Carmona-Bernal C, Asensio-Cruz MI, Cabello M, et al. Primary care physicians can comprehensively manage patients with sleep apnea: a noninferiority randomized controlled trial. Am J Respir Crit Care Med. 2018;198(5):648–56.
Sánchez-de-la-Torre M, Nadal N, Cortijo A, Masa JF, Duran-Cantolla J, Valls J, et al. Role of primary care in the follow-up of patients with obstructive sleep apnoea undergoing CPAP treatment: a randomised controlled trial. Thorax. 2015;70(4):346–52.
Mar J, Rueda JR, Durán-Cantolla J, Schechter C, Chilcott J. The cost-effectiveness of nCPAP treatment in patients with moderate-to-severe obstructive sleep apnoea. Eur Respir J. 2003;21(3):515–22.
Lugo VM, Garmendia O, Suarez-Girón M, Torres M, Vázquez-Polo FJ, Negrín MA, et al. Comprehensive management of obstructive sleep apnea by telemedicine: clinical improvement and cost-effectiveness of a virtual sleep unit. A randomized controlled trial. PLoS One. 2019;14(10): e0224069.
Isetta V, Negrín MA, Monasterio C, Masa JF, Feu N, Álvarez A, et al. A Bayesian cost-effectiveness analysis of a telemedicine-based strategy for the management of sleep apnoea: a multicentre randomised controlled trial. Thorax. 2015;70(11):1054–61.
de Vries GE, Hoekema A, Vermeulen KM, Claessen JQPJ, Jacobs W, van der Maten J, et al. Clinical- and cost-effectiveness of a mandibular advancement device versus continuous positive airway pressure in moderate obstructive sleep apnea. J Clin Sleep Med. 2019;15(10):1477–85.
Quinnell TG, Bennett M, Jordan J, Clutterbuck-James AL, Davies MG, Smith IE, et al. A crossover randomised controlled trial of oral mandibular advancement devices for obstructive sleep apnoea-hypopnoea (TOMADO). Thorax. 2014;69(10):938–45.
McMillan A, Bratton DJ, Faria R, Laskawiec-Szkonter M, Griffin S, Davies RJ, et al. A multicentre randomised controlled trial and economic evaluation of continuous positive airway pressure for the treatment of obstructive sleep apnoea syndrome in older people: PREDICT. Health Technol Assess. 2015;19(40):1–188.
McMillan A, Bratton DJ, Faria R, Laskawiec-Szkonter M, Griffin S, Davies RJ, et al. Continuous positive airway pressure in older people with obstructive sleep apnoea syndrome (PREDICT): a 12-month, multicentre, randomised trial. Lancet Respir Med. 2014;2(10):804–12.
Lojander J, Räsänen P, Sintonen H, Roine RP. Effect of nasal continuous positive airway pressure therapy on health-related quality of life in sleep apnoea patients treated in the routine clinical setting of a university hospital. J Int Med Res. 2008;36(4):760–70.
Catala R, Villoro R, Merino M, Sangenis S, Colomes L, Hernandez Flix S, et al. Cost-effectiveness of continuous positive airway pressure treatment in moderate-severe obstructive sleep apnea yndrome. Arch Bronconeumol. 2016;52(9):461–9.
Blissett DB, Steier JS, Karagama YG, Blissett RS. Breathing synchronised hypoglossal nerve stimulation with inspire for untreated severe obstructive sleep apnoea/hypopnoea syndrome: a simulated cost-utility analysis from a national health service perspective. Pharmacoeconomics. 2021;5(3):475–89.
Sharples L, Glover M, Clutterbuck-James A, Bennett M, Jordan J, Chadwick R, et al. Clinical effectiveness and cost-effectiveness results from the randomised controlled Trial of Oral Mandibular Advancement Devices for Obstructive sleep apnoea-hypopnoea (TOMADO) and long-term economic analysis of oral devices and continuous positive airway pressure. Health Technol Assess. 2014;18(67):1–296.
Robles A, Gil-Rojas Y, Amaya D, Hernández F, Escobar-Cordoba F, Venegas M, et al. Cost-utility and budget impact analysis of CPAP therapy compared to no treatment in the management of moderate to severe obstructive sleep apnea in Colombia from a third-party payer perspective. Expert Rev Pharmacoecon Outcomes Res. 2023;23(4):399–407.
Tan MC, Ayas NT, Mulgrew A, Cortes L, FitzGerald JM, Fleetham JA, et al. Cost-effectiveness of continuous positive airway pressure therapy in patients with obstructive sleep apnea-hypopnea in British Columbia. Can Respir J. 2008;15(3):159–65.
Poullie AI, Cognet M, Gauthier A, Clementz M, Druais S, Spath HM, et al. Cost-effectiveness of treatments for mild-to-moderate obstructive sleep apnea in France. Int J Technol Assess Health Care. 2016;32(1–2):37–45.
McDaid C, Griffin S, Weatherly H, Duree K, van der Burgt M, van Hout S, et al. Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea-hypopnoea syndrome: a systematic review and economic analysis. Health Technol Assess. 2009;13(4):43–274.
Guest JF, Helter MT, Morga A, Stradling JR. Cost-effectiveness of using continuous positive airway pressure in the treatment of severe obstructive sleep apnoea/hypopnoea syndrome in the UK. Thorax. 2008;63(10):860–5.
Guest JF, Panca M, Sladkevicius E, Taheri S, Stradling J. Clinical outcomes and cost-effectiveness of continuous positive airway pressure to manage obstructive sleep apnea in patients with type 2 diabetes in the UK. Diabetes Care. 2014;37(5):1263–71.
Weatherly HL, Griffin SC, Mc Daid C, Duree KH, Davies RJ, Stradling JR, et al. An economic analysis of continuous positive airway pressure for the treatment of obstructive sleep apnea-hypopnea syndrome. Int J Technol Assess Health Care. 2009;25(1):26–34.
Billings ME, Kapur VK. Medicare long-term CPAP coverage policy: a cost-utility analysis. J Clin Sleep Med. 2013;9(10):1023–9.
Pietzsch JB, Garner A, Cipriano LE, Linehan JH. An integrated health-economic analysis of diagnostic and therapeutic strategies in the treatment of moderate-to-severe obstructive sleep apnea. Sleep. 2011;34(6):695–709.
Okubo R, Kondo M, Hoshi SL, Yamagata K. Cost-effectiveness of obstructive sleep apnea screening for patients with diabetes or chronic kidney disease. Sleep Breath. 2015;19(3):1081–92.
Sankar A, Dixon PR, Sivanathan L, Memtsoudis SG, de Almeida JR, Singh M. Cost-effectiveness analysis of preoperative screening strategies for obstructive sleep apnea among patients undergoing elective inpatient surgery. Anesthesiology. 2020;133(4):787–800.
Sadatsafavi M, Marra CA, Ayas NT, Stradling J, Fleetham J. Cost-effectiveness of oral appliances in the treatment of obstructive sleep apnoea-hypopnoea. Sleep Breath. 2009;13(3):241–52.
Tan KB, Toh ST, Guilleminault C, Holty JE. A cost-effectiveness analysis of surgery for middle-aged men with severe obstructive sleep apnea intolerant of CPAP. J Clin Sleep Med. 2015;11(5):525–35.
Trenaman L, Sadatsafavi M, Almeida F, Ayas N, Lynd L, Marra C, et al. Exploring the potential cost-effectiveness of patient decision aids for use in adults with obstructive sleep apnea: a case study. Med Decis Making. 2015;35(5):671–82.
Zupancic JA, Richardson DK, O’Brien BJ, Eichenwald EC, Weinstein MC. Cost-effectiveness analysis of predischarge monitoring for apnea of prematurity. Pediatrics. 2003;111(1):146–52.
Corral J, Sánchez-Quiroga M, Carmona-Bernal C, Sánchez-Armengol Á, de la Torre AS, Durán-Cantolla J, et al. Conventional polysomnography is not necessary for the management of most patients with suspected obstructive sleep apnea: noninferiority, randomized controlled trial. Am J Respir Crit Care Med. 2017;196(9):1181–90.
Tarraubella N, Sánchez-de-la-Torre M, Nadal N, De Batlle J, Benítez I, Cortijo A, et al. Management of obstructive sleep apnoea in a primary care vs sleep unit setting: a randomised controlled trial. Thorax. 2018;73(12):1152–60.
Antic NA, Buchan C, Esterman A, Hensley M, Naughton MT, Rowland S, et al. A randomized controlled trial of nurse-led care for symptomatic moderate-severe obstructive sleep apnea. Am J Respir Crit Care Med. 2009;179(6):501–8.
Pelletier-Fleury N, Meslier N, Gagnadoux F, Person C, Rakotonanahary D, Ouksel H, et al. Economic arguments for the immediate management of moderate-to-severe obstructive sleep apnoea syndrome. Eur Respir J. 2004;23(1):53–60.
Boulos MI, Kamra M, Colelli DR, Kirolos N, Gladstone DJ, Boyle K, et al. SLEAP SMART (Sleep Apnea Screening Using Mobile Ambulatory Recorders After TIA/Stroke): a randomized controlled trial. Stroke. 2022;53(3):710–8.
Rosen CL, Auckley D, Benca R, Foldvary-Schaefer N, Iber C, Kapur V, et al. A multisite randomized trial of portable sleep studies and positive airway pressure autotitration versus laboratory-based polysomnography for the diagnosis and treatment of obstructive sleep apnea: the HomePAP study. Sleep. 2012;35(6):757–67.
Turino C, Benítez ID, Rafael-Palou X, Mayoral A, Lopera A, Pascual L, et al. Management and treatment of patients with obstructive sleep apnea using an intelligent monitoring system based on machine learning aiming to improve continuous positive airway pressure treatment compliance: randomized controlled trial. J Med Internet Res. 2021;23(10): e24072.
Andreu AL, Chiner E, Sancho-Chust JN, Pastor E, Llombart M, Gomez-Merino E, et al. Effect of an ambulatory diagnostic and treatment programme in patients with sleep apnoea. Eur Respir J. 2012;39(2):305–12.
Kim RD, Kapur VK, Redline-Bruch J, Rueschman M, Auckley DH, Benca RM, et al. An economic evaluation of home versus laboratory-based diagnosis of obstructive sleep apnea. Sleep. 2015;38(7):1027–37.
Hui DS, Ng SS, To KW, Ko FW, Ngai J, Chan KK, et al. A randomized controlled trial of an ambulatory approach versus the hospital-based approach in managing suspected obstructive sleep apnea syndrome. Sci Rep. 2017;4(8):45901.
Watanabe N, Furukawa TA, Shimodera S, Katsuki F, Fujita H, Sasaki M, et al. Cost-effectiveness of cognitive behavioral therapy for insomnia comorbid with depression: analysis of a randomized controlled trial. Psychiatry Clin Neurosci. 2015;69(6):335–43.
Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M. Psychological treatment for insomnia in the regulation of long-term hypnotic drug use. Health Technol Assess. 2004;8(8):1–68.
Snedecor SJ, Botteman MF, Bojke C, Schaefer K, Barry N, Pickard AS. Cost-effectiveness of eszopiclone for the treatment of adults with primary chronic insomnia. Sleep. 2009;32(6):817–24.
De Bruin EJ, van Steensel FJA, Meijer AM. Cost-effectiveness of group and internet cognitive behavioral therapy for insomnia in adolescents: results from a randomized controlled trial. Sleep. 2016;39(8):1571–81.
Thiart H, Ebert DD, Lehr D, Nobis S, Buntrock C, Berking M, et al. Internet-based cognitive behavioral therapy for insomnia: a health economic evaluation. Sleep. 2016;39(10):1769–78.
Tsiachristas A, Waite F, Freeman D, Luengo-Fernandez R. Cost-effectiveness of cognitive-behavioural therapy for sleep disorder added to usual care in patients with schizophrenia: the BEST study. BJPsych Open. 2018;4(3):126–35.
Darden M, Espie CA, Carl JR, Henry AL, Kanady JC, Krystal AD, et al. Cost-effectiveness of digital cognitive behavioral therapy (Sleepio) for insomnia: a Markov simulation model in the United States. Sleep. 2021;44(4):zsaa223.
Baka A, van der Zweerde T, Lancee J, Bosmans JE, van Straten A. Cost-effectiveness of guided internet-delivered cognitive behavioral therapy in comparison with care-as-usual for patients with insomnia in general practice. Behav Sleep Med. 2021;28:1–16.
Yeung K, Zhu W, McCurry SM, Von Korff M, Wellman R, Morin CM, et al. Cost-effectiveness of telephone cognitive behavioral therapy for osteoarthritis-related insomnia. J Am Geriatr Soc. 2021;11:11.
Savard J, Ivers H, Morin CM, Lacroix G. Video cognitive-behavioral therapy for insomnia in cancer patients: a cost-effective alternative. Psychooncology. 2021;30(1):44–51.
Buntrock C, Lehr D, Smit F, Horvath H, Berking M, Spiegelhalder K, et al. Guided internet-based cognitive behavioral therapy for insomnia: health-economic evaluation from the societal and public health care perspective alongside a randomized controlled trial. J Med Internet Res. 2021;23(5): e25609.
Lee JE, Jung IC, Lee SY, Lim JH, Kim BK, Cho E. The cost-effectiveness analysis of Gamiguibi-Tang versus Hwangryunhaedok-Tang for patients with insomnia disorder based on a randomized controlled trial. Healthcare (Basel). 2022;10(11):2157.
Ikeda S, Azuma MK, Fujimoto K, Shibahara H, Inoue S, Moline M, et al. Cost-effectiveness analysis of lemborexant for treating insomnia in Japan: a model-based projection, incorporating the risk of falls, motor vehicle collisions, and workplace accidents. Psychol Med. 2022;52(13):2822–34.
Nishimura S, Nakao M. Cost-effectiveness analysis of suvorexant for the treatment of Japanese elderly patients with chronic insomnia in a virtual cohort. J Med Econ. 2018;21(7):698–703.
Tannenbaum C, Diaby V, Singh D, Perreault S, Luc M, Vasiliadis HM. Sedative-hypnotic medicines and falls in community-dwelling older adults: a cost-effectiveness (decision-tree) analysis from a US Medicare perspective. Drugs Aging. 2015;32(4):305–14.
Scott GW, Scott HM, O’Keeffe KM, Gander PH. Insomnia: treatment pathways, costs and quality of life. Cost Eff Resour Alloc. 2011;21(9):10.
Botteman MF, Ozminkowski RJ, Wang S, Pashos CL, Schaefer K, Foley DJ. Cost effectiveness of long-term treatment with eszopiclone for primary insomnia in adults: a decision analytical model. CNS Drugs. 2007;21(4):319–34.
AIHW (Australian Institute of Health and Welfare). The problem of osteoporotic hip fracture in Australia. Canberra (ACT): AIHW (Australian Institute of Health and Welfare). 2010.
Snedecor SJ, Botteman MF, Schaefer K, Sarocco P, Barry N, Pickard AS. Economic outcomes of eszopiclone treatment in insomnia and comorbid major depressive disorder. J Ment Health Policy Econ. 2010;13(1):27–35.
Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ. 2004;13(9):873–84.
Shiroiwa T, Fukuda T, Ikeda S, Igarashi A, Noto S, Saito S, et al. Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual Life Res. 2016;25(3):707–19.
Brazier JE, Roberts J. The estimation of a preference-based measure of health from the SF-12. Med Care. 2004;42(9):851–9.
Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med. 2001;33(5):328–36.
Banerjee D. The Epworth sleepiness scale. Occup Med. 2007;57(3):232.
Campbell AJ, Neill AM, Scott DAR. Clinical reproducibility of the Epworth Sleepiness Scale for patients with suspected sleep apnea. J Clin Sleep Med. 2018;14(5):791–5.
Kapur VK, Baldwin CM, Resnick HE, Gottlieb DJ, Nieto FJ. Sleepiness in patients with moderate to severe sleep-disordered breathing. Sleep. 2005;28(4):472–7.
Berkley AS, Carter PA, Yoder LH, Acton G, Holahan CK. The effects of insomnia on older adults’ quality of life and daily functioning: a mixed-methods study. Geriatr Nurs. 2020;41(6):832–8.
Shahid A, Wilkinson K, Marcu S, Shapiro CM, editors. STOP, THAT and one hundred other sleep scales. New York: Springer; 2012.
Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307.
Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–8.
Gu NY, Botteman MF, Ji X, Bell CF, Carter JA, van Hout B. Mapping of the Insomnia Severity Index and other sleep measures to EuroQol EQ-5D health state utilities. Health Qual Life Outcomes. 2011;9(1):119.
Billings ME, Rosen CL, Auckley D, Benca R, Foldvary-Schaefer N, Iber C, et al. Psychometric performance and responsiveness of the functional outcomes of sleep questionnaire and sleep apnea quality of life instrument in a randomized trial: the HomePAP study. Sleep. 2014;37(12):2017–24.
Chasens ER, Ratcliffe SJ, Weaver TE. Development of the FOSQ-10: a short version of the Functional Outcomes of Sleep Questionnaire. Sleep. 2009;32(7):915–9.
Alessi CA, Fung CH, Dzierzewski JM, Fiorentino L, Stepnowsky C, Rodriguez Tapia JC, et al. Randomized controlled trial of an integrated approach to treating insomnia and improving the use of positive airway pressure therapy in veterans with comorbid insomnia disorder and obstructive sleep apnea. Sleep. 2021;44(4):zsaa235.
Weaver TE, Drake CL, Benes H, Stern T, Maynard J, Thein SG, et al. Effects of solriamfetol on quality-of-life measures from a 12-week phase 3 randomized controlled trial. Ann Am Thorac Soc. 2020;17(8):998–1007.
Weaver TE, Menno DM, Bron M, Crosby RD, Morris S, Mathias SD. Determination of thresholds for minimally important difference and clinically important response on the functional outcomes of sleep questionnaire short version in adults with narcolepsy or obstructive sleep apnea. Sleep Breath. 2021. https://doi.org/10.1007/s11325-020-02270-3.
Coman AC, Borzan C, Vesa CS, Todea DA. Obstructive sleep apnea syndrome and the quality of life. Clujul Med. 2016;89(3):390–5.
Knufinke M, Nieuwenhuys A, Geurts SAE, Coenen AML, Kompier MAJ. Self-reported sleep quantity, quality and sleep hygiene in elite athletes. J Sleep Res. 2018;27(1):78–85.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40.
Barber-Westin SD, Noyes FR. Chapter 43: rating of athletic and daily functional activities: knee-specific scales and global outcome instruments. In: Noyes FR, Barber-Westin SD, editors. Noyes’ knee disorders: surgery, rehabilitation, clinical outcomes. 2nd ed. Elsevier; 2017. p. 1211–21.
Williams JB, Kobak KA, Bech P, Engelhardt N, Evans K, Lipsitz J, et al. The GRID-HAMD: standardization of the Hamilton Depression Rating Scale. Int Clin Psychopharmacol. 2008;23(3):120–9.
Reimer MA, Flemons WW. Quality of life in sleep disorders. Sleep Med Rev. 2003;7(4):335–49.
Chen TH, Li L, Kochen MM. A systematic review: how to choose appropriate health-related quality of life (HRQOL) measures in routine general practice? J Zhejiang Univ Sci B. 2005;6(9):936–40.
National Institute for Health Care Excellence. NICE Process and Methods Guides. The social care guidance manual. London: National Institute for Health and Care Excellence (NICE). 2016: 92.
Nikl A, Janssen MF, Brodszky V, Rencz F. A head-to-head comparison of the EQ-5D-5L and 15D descriptive systems and index values in a general population sample. Health Qual Life Outcomes. 2023;21(1):17.
Koivunen K, Sintonen H, Lukkarinen H. Properties of the 15D and the Nottingham Health Profile questionnaires in patients with lower limb atherosclerotic disease. Int J Technol Assess Health Care. 2007;23(3):385–91.
Stavem K, Frøland SS, Hellum KB. Comparison of preference-based utilities of the 15D, EQ-5D and SF-6D in patients with HIV/AIDS. Qual Life Res. 2005;14(4):971–80.
Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res. 2013;22(7):1717–27.
Christiansen ASJ, Møller MLS, Kronborg C, Haugan KJ, Køber L, Højberg S, et al. Comparison of the three-level and the five-level versions of the EQ-5D. Eur J Health Econ. 2021;22(4):621–8.
Huber FL, Furian M, Kohler M, Latshang TD, Nussbaumer-Ochsner Y, Turk A, et al. Health preference measures in patients with obstructive sleep apnea syndrome undergoing continuous positive airway pressure therapy: data from a randomized trial. Respiration. 2021;100(4):328–38.
Finch AP, Brazier JE, Mukuria C. What is the evidence for the performance of generic preference-based measures? A systematic overview of reviews. Eur J Health Econ. 2018;19(4):557–70.
Boulos MI, Kamra M, Colelli DR, Kirolos N, Gladstone DJ, Boyle K, et al. SLEAP SMART (Sleep Apnea Screening Using Mobile Ambulatory Recorders After TIA/Stroke): a randomized controlled trial. Stroke. 2021:STROKEAHA120033753.
Gill TM, Feinstein AR. A critical appraisal of the quality of quality-of-life measurements. JAMA. 1994;272(8):619–26.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. No funding was received for the preparation of this article.
Author information
Authors and Affiliations
Contributions
Concept and design: BK. Acquisition of data: AN, T-JW, NB, CM-K. Analysis and interpretation of data: BK, T-JW, AN, NB, CM-K. Drafting of the manuscript: BK, T-JW, AN, NB, CM-K, AS, AR, KAL, DE. Critical revision of the paper for important intellectual content: KAL, PC, DE. Supervision: BK.
Corresponding author
Ethics declarations
Conflict of Interest
Alexander Sweetman has backing from the National Health and Medical Research Council (NHMRC), Flinders University, Flinders Foundation, ResMed Foundation, Philips Respironics, Hospital Research Foundation and Big Health, along with consultancies for Australian Doctor Group, Cerebra and Sleep Review Mag. Peter G. Catcheside declares grants from the NHMRC, Defence Science and Technology Group, Flinders University, Compumedics Pty Ltd, REDARC and Invicta Medical, patent-related payments from Philips, and in-kind support from Philips and Compumedics, unrelated to this article. Amy C. Reynolds reports paid workshops for the Sleep Health Foundation and presentations for Teva Pharmaceuticals. Robert Adams has received grants from various foundations unrelated to this study. Danny J. Eckert holds an NHMRC Leadership Fellowship (1196261) and received research grants from Bayer, Takeda, Invicta Medical, Apnimed and Withings. He has also served on advisory boards or as a consultant for Apnimed, Invicta, Mosanna, Takeda and Bayer, delivered a lecture sponsored by Philips and has a pending patent application for sleep apnoea. Billingsley Kaambwa, Taylor-Jade Woods, Andrea Natsky, Norma Bulamu, Christine Mpundu-Kaambwa, and Kelly A. Loffler have no conflicts of interest that are directly relevant to the content of this article.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kaambwa, B., Woods, TJ., Natsky, A. et al. Content Comparison of Quality-of-Life Instruments Used in Economic Evaluations of Sleep Disorder Interventions: A Systematic Review. PharmacoEconomics 42, 507–526 (2024). https://doi.org/10.1007/s40273-023-01349-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-023-01349-5