Abstract
Aims
The aim of this study was to explore the experiences, values and preferences of people living with relapsing multiple sclerosis (PLwRMS) focusing on their treatments and what drives their treatment preferences.
Methods
In-depth, semi-structured, qualitative telephone interviews were conducted using a purposive sampling approach with 72 PLwRMS and 12 health care professionals (HCPs, MS specialist neurologists and nurses) from the United Kingdom, United States, Australia and Canada. Concept elicitation questioning was used to elicit PLwRMS’ attitudes, beliefs and preferences towards features of disease-modifying treatments. Interviews with HCPs were conducted to inform on HCPs’ experiences of treating PLwRMS. Responses were audio recorded and transcribed verbatim and then subjected to thematic analysis.
Results
Participants discussed numerous concepts that were important to them when making treatment decisions. Levels of importance participants placed on each concept, as well as reasons underpinning importance, varied substantially. The concepts with the greatest variability in terms of how much PLwRMS found them to be important in their decision-making process were mode of administration, speed of treatment effect, impact on reproduction and parenthood, impact on work and social life, patient engagement in decision making, and cost of treatment to the participant. Findings also demonstrated high variability in what participants described as their ideal treatment and the most important features a treatment should have. HCP findings provided clinical context for the treatment decision-making process and supported patient findings.
Conclusions
Building upon previous stated preference research, this study highlighted the importance of qualitative research in understanding what drives patient preferences. Characterized by the heterogeneity of the RMS patient experience, findings indicate the nature of treatment decisions in RMS to be highly individualized, and the subjective relative importance placed on different treatment factors by PLwRMS to vary. Such qualitative patient preference evidence could offer valuable and supplementary insights, alongside quantitative data, to inform decision making related to RMS treatment.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
The importance of understanding how people living with relapsing multiple sclerosis (PLwRMS) make benefit–risk trade-offs in treatment decisions is recognized in MS treatment guidelines and guidance from regulatory and HTA bodies in the US and Europe. However, reasons why certain features of disease-modifying therapies (DMTs) are considered to be more important than others have not been qualitatively explored from the patient perspective. |
Feedback from PLwRMS highlighted that a number of factors related to the treatment itself, its anticipated impact on their lives and the context of the decision-making process are considered when making treatment decisions. However, significant variability and individual differences were observed between PLwRMS in the level of importance they place on each of these factors, what they consider to be an ideal treatment and their reasons why. |
Findings from this study emphasize the importance of incorporating patient preferences alongside clinical evidence to support individual treatment decisions and personalized treatment pathways for PLwRMS. |
1 Introduction
Relapsing multiple sclerosis (RMS) is an extremely heterogeneous condition, presenting different symptom profiles with varying severities including sensory disturbances, followed by weakness and visual disturbances [1]. RMS is characterized by acute episodes of disease activity, followed by periods of symptom remission [2] and there is the potential for some patients to transition to secondary progressive MS [3]. Subsequently, people living with RMS (PLwRMS) report an inherent uncertainty regarding disease progression and management, and how this will impact their health-related quality of life (HRQoL) [4,5,6,7]. Additionally, the heterogeneity of the disease manifestation may result in notable individual differences among PLwRMS with respect to treatment preferences and priorities.
PLwRMS are typically offered disease-modifying treatments (DMTs), which aim to control the disease evolution and to slow progression and accumulated disability [8]. The DMTs available have varying features to consider, including mode of administration (oral, intravenous and subcutaneously injectable), frequency of administration (e.g. daily, weekly, monthly, every 6 months, yearly), levels of efficacy and risk of various side effects [9,10,11,12,13]. The variety of DMTs available can make treatment selection complex for PLwRMS and their healthcare professional (HCP). The unpredictable course of RMS, uncertainty around treatment response and variation in PLwRMS’ attitudes to risk further complicates treatment choices; some people may even opt for no treatment. For HCPs, the uncertainty surrounding clinical incompatibility with treatment and funding factors further adds to the complications surrounding choosing an appropriate treatment [14]. National treatment guidelines for MS from multiple countries [15,16,17,18,19,20] highlight the importance of shared decision-making between PLwRMS and their HCPs when making treatment choices. Through this shared framework, it is hoped that PLwRMS feel informed, engaged and satisfied with their chosen treatment pathway, thus improving adherence and potential health outcomes [21,22,23]. Nonetheless, information on how such discussions should take place and what specific treatment factors should be discussed are limited [15,16,17,18,19,20, 24].
The National Health Service treatment algorithm for MS DMTs in the United Kingdom (UK) [25] highlights treatment-specific features such as administration, efficacy and side effects as important to consider and discuss with PLwRMS [4, 21, 26, 27]. However, the guidance does not consider broader, non-treatment-specific factors which may also influence decision making, such as the impact of treatment on a patients’ lifestyle (e.g. work, daily activities including mobility, family) and psychological factors. Subsequently, clinician decisions to recommend DMTs are more driven by the perceived toxicity and efficacy of DMTs rather than the additional psychosocial factors that will also likely inform how sustainable the DMT will be in their patient’s everyday life [28].
Stated-preference studies, specifically discrete choice experiments (DCEs), have explored the relative importance of DMT attributes to PLwRMS [4, 26, 27], however they have been subject to methodological criticism. A systematic review of recent stated-preference studies indicated that robust approaches towards the identification, selection and subsequent validation of attributes and levels with qualitative patient input was lacking in many published studies [24]. Since then, a number of qualitative studies have been conducted which have outlined how important communication with HCPs is at the initial stage of starting treatment and how patient preferences for treatment can change during the course of the condition [14, 29]. While the literature provides an indication of certain attributes that are considered by patients in their decision-making process, the reason why PLwRMS may place more importance on certain attributes over others appears to be lacking, particularly from the patient perspective.
The United States (US) Food and Drug Administration (FDA) has acknowledged the importance of patients’ benefit–risk perspectives when evaluating medical devices for regulatory approval [22, 23, 30]. Examples of both quantitative (DCE in obesity) and qualitative (identifying caregiver treatment preferences in Duchenne muscular dystrophy) assessments of patient preference data have been disseminated by the FDA. Health technology assessment (HTA) bodies such as the National Institute for Health and Care Excellence (NICE) [31], and the Scottish Medicines Consortium [32], have also acknowledged that patient experience data can offer supplementary insights regarding factors not captured in quality-adjusted life-years within technology assessments; notably highlighting the value of understanding patient trade-offs within heterogenous patient populations [32, 33]. However, it remains unclear how patient preference data is to be incorporated into regulatory and reimbursement decisions [34].
The importance of understanding how PLwRMS make benefit–risk trade-offs in treatment decisions is recognized in MS treatment guidelines across multiple countries, as well as regulatory and HTA bodies in the US and Europe [15,16,17,18,19,20, 31, 32]. While current patient preference research in RMS has highlighted treatment-specific and broader non-treatment-specific features that are important to PLwRMS, the reasons why certain features of a treatment are considered to be more important than others has not been qualitatively explored from the patient perspective. Given the heterogeneity of the RMS patient experience, it is crucial to understand how and why PLwRMS and their HCPs approach treatment decisions to fully explore what factors drive and inform their decisions. To address this unmet need [24], in-depth qualitative interviews were conducted with PLwRMS and HCPs who manage/treat PLwRMS across the UK, Canada, US and Australia to explore the experiences, values and preferences across different healthcare systems.
2 Methodology
2.1 Study Design
This was a qualitative study composed of 60-min, in-depth, semi-structured telephone interviews with 72 adult PLwRMS and 12 HCPs across the UK, US, Australia and Canada (Fig. 1).
A meeting was held with members from NICE and CADTH (Canadian Agency for Drugs and Technologies in Health) in December 2019, to obtain guidance and feedback from MS experts, patient experts and reimbursement bodies on the proposed methodology. The study was informed by the agencies, however neither agency reviewed nor approved the final study design.
2.2 Study Sample
2.2.1 Patient Sample
Using sampling quotas (Online Resource 1, see electronic supplementary material [ESM]), a purposive sampling approach was used to ensure patients with a range of demographic, educational and clinical characteristics were recruited. In total, 72 PLwRMS from the UK (n = 18), US (n = 18), Australia (n = 18) and Canada (n = 18) participated in the study. Eligible participants were ≥18 years, had a clinician-confirmed diagnosis of RMS, and had made at least one treatment decision for their MS since diagnosis (including deciding not to start/take a treatment and/or to stop a treatment). Participants had to be verbally fluent and literate in English and have the cognitive and linguistic capabilities to participate in a 60-minute telephone interview (according to their clinician). Participants were excluded from the study if they had any comorbidities which affected their ability to clearly attribute their symptoms and experiences to RMS, or if they had any other physical or mental illness, that in their clinician’s opinion, might influence their responses.
2.2.2 Health Care Provider (HCP) Sample
A purposive sampling approach was used to ensure at least one MS specialist neurologist and one MS specialist nurse was recruited from each of the four countries. In total, 12 HCPs from the UK (n = 3), US (n = 3), Australia (n = 3) and Canada (n = 3) participated in the study. Eligible HCPs were either MS specialist neurologists with at least 3 years’ experience in practice, treating at least 15 MS patients a month and spending more than 60% of their time in clinical practice or MS specialist nurses who held an MS Nursing Certification with 2 years’ experience working in the four domains of MS nursing (clinical practice, advocacy, education and research).
2.3 Recruitment
Third-party recruitment agencies shared details about the study with referring clinicians to recruit PLwRMS and HCPs. PLwRMS eligible for participation and who expressed interest in the study were then referred by their treating clinicians to the recruitment agency to take part in the study. Recruitment agencies provided all referred participants with an Information and Consent Form (ICF) providing details of the study and gave patients the opportunity to ask any questions prior to providing written informed consent to participate. Following receipt of consent, recruitment agencies collected demographic (via a self-report form) and clinical information (via a clinician-completed case report form) for PLwRMS, which facilitated the monitoring of achievement of sampling quotas throughout the recruitment process (Online Resource 1, see ESM). All participants were remunerated via cash in their local currency or in the form of an Amazon voucher for participating ($160 AUS/$135 CAN/£80 UK/$100 USA).
2.4 Qualitative Interviews
2.4.1 Patient Interviews
Semi-structured, 60-min telephone interviews were conducted in English by experienced qualitative interviewers (AB, WN, CF and an additional Australian-based interviewer) who had been briefed on the study objectives and interview guide (Online Resource 2, see ESM) prior to conducting interviews. The interview guide was informed by a targeted literature review of previous patient preference research (Online Resource 3, see ESM), as recommended by NICE and CADTH. The targeted literature review supported identification of concepts reported to be important to PLwRMS and informed the development of concept elicitation (CE) questioning in the interview guide. CE questioning was deemed the most appropriate approach given it provides an in-depth understanding of the patient experience [35]. Questions were designed to elicit spontaneous responses from participants regarding their attitudes, beliefs and preferences towards features of DMTs, in an open-ended and unbiased manner. Any key concepts identified in the literature review that were not spontaneously discussed by participants during the interview were probed by the interviewer where time permitted. Additional questions relating to current and past treatment experiences, the most important factors considered when making treatment decisions and participants’ ideal treatment were also explored. To evaluate the suitability of the interview guide, six pilot interviews were first conducted with PLwRMS in the UK (n = 3) and US (n = 3). External expert qualitative input was sought via a key opinion leader and medical leads in the field of RMS during the development of the interview guide and after the conduct of pilot interviews, to refine the guide.
2.4.2 HCP Interviews
Semi-structured, 60-minute telephone interviews were conducted in English by trained qualitative interviewers (AB, WN, CF and an additional Australian-based interviewer), to contextualize the patient decision-making process from the HCP perspective. Similar to the patient interview guide (Online Resource 2, see ESM), the HCP interview guide (Online Resource 4, see ESM) utilized open-ended and probed CE questioning. While both interview guides aimed to elicit the factors which drive patient decisions and the reasons why, the HCP interview guide was tailored to obtain this information from a clinical perspective and based on the HCP’s experience. The HCP interview guide additionally aimed to explore HCPs’ experiences of treating PLwRMS (including those opting for no treatment) and HCPs’ experiences on the factors that drive RMS treatment preferences, such as level of engagement and the types of information patients consider/rely upon.
2.5 Ethics
The study was conducted in accordance with local guidelines. Ethical approval, participant remuneration and oversight of the study was provided by a centralized ethics review committee (Western Independent Review Board® [WIRB]; approval reference number: 20202348). The study protocol was approved by WIRB and study procedures ensured that all participants provided consent, via signing the ICF, prior to the collection of any data.
2.6 Qualitative Analysis
Interviews were audio recorded and transcribed verbatim, with identifiable information redacted to anonymize participants. Instead, participants were assigned a unique identification number. For patients, this denoted the order of site recruitment, sex, age and the country from which they were recruited. For HCPs, this denoted the order of site recruitment, ‘HCP’ to differentiate from patients, type of HCP (neuro = neurologist, nurse = MS specialist nurse) and the country they were recruited from. Verbatim transcripts were coded by experienced qualitative researchers (AB, WN and CF) who had been briefed on the study interview guides and study objectives. Transcripts were subject to thematic analysis using Atlas.Ti software (Online Resource 1, see ESM). Thematic analysis is a foundational, theory-free, qualitative analysis method, providing a rich, detailed and complex synthesis of qualitative data that meets a very specific and applied aim [36, 37]. An abductive approach was taken to coding whereby concepts were identified directly from the data and by applying prior knowledge [38]. This approach enabled the analysis to remain grounded in the data, allowing participants to identify areas of importance to them, but also taking into consideration prior knowledge when applying codes. Research team discussions were held to gain consensus on codes used and interpretations during the data analysis process to help reduce bias. Sub-group analysis was also conducted to explore trends within the data and highlight any cross-country differences. Following analysis, concept frequency was determined by counting the number of participants who mentioned a concept, defined as a feature of treatment which was discussed at least once, during the interview. Data saturation analysis, commonly defined as the point at which no new relevant concepts (for this specific study—features of treatment) can be identified, was conducted at both the country level and across the whole sample to ensure the data collection process was rigorous and exhaustive, as well as to confirm if the sample size was sufficient [39,40,41].
3 Results
3.1 Participant Sample
3.1.1 Patient Sample Characteristics
Seventy-two adult PLwRMS, from four countries, participated. The sample represented a wide range of demographic and clinical characteristics (Table 1, further detail provided in Online Resource 5, see ESM). At the time of interview, 83.3% (n = 60/72) participants were receiving a DMT, 65.3% (n = 47/72) participants had previously received a DMT and 7.0% (n = 5/72) participants had refused a treatment.
3.1.2 HCP Sample Characteristics
Of the 12 HCPs who participated in the study, 75.0% were MS specialist neurologists (n = 9/12) and 25.0% (n = 3/12) were MS specialist nurses.
3.2 Overview of Findings
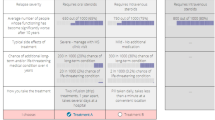
Figure 2 provides an overview of all 39 concepts described to be important to PLwRMS, either spontaneously (elicited by the participant without being prompted by the interviewer) or probed (reported by the participant only when questioned by the interviewer). The number of participants who did not find a concept relevant to their treatment decision making and the number of participants who did not discuss a concept is also provided. The concepts most commonly reported to inform treatment preferences were input from HCP, patient engagement in decision making and mode of administration. Findings from the patient interviews are discussed in comparison with findings from the HCP interviews, to help contextualize findings.
Data saturation was achieved across the total sample and within each country with the exception of impact on sex life, which was not discussed spontaneously in any interviews. This could reflect participants’ reluctance to disclose such information within an interview, or low relevance.
3.3 Findings: Differences in Preferences for Treatment and the Decision-Making Process
Findings highlighted key differences between respondents in the features of treatment reported to be important to PLwRMS when making a treatment decision, and critically why those features were important. There were generally no meaningful cross-country differences with regards to the frequency that concepts were mentioned unless specified. Differences in preferences for treatment were assessed by comparing the percentages of participants who discussed a concept to be important (as measured by whether that concept was mentioned spontaneously or probed) compared with the percentage of participants who discussed a concept as not important. Six concepts were identified from the analysis where differences in preferences for treatment were most prominent (i.e. the proportion of participants who discussed the concept as being important was similar to that of those who discussed the concept as not being important): patient engagement, mode of administration, speed of effect, reproduction and parenthood, impact on work/social life and cost of treatment. The variation in preferences for each of these six concepts are discussed in greater detail in the following sections.
Due to the study being conducted during the COVID-19 pandemic, some participants spontaneously mentioned how their treatment preferences had changed due to there being limited options available to access treatment (n = 5/72, 6.9%). Most of those participants explained how they would have preferred to have taken treatment in hospital; however, they were advised against this due to their increased risk of catching COVID-19 by travelling to and staying in hospital (n = 3/5, 60.0%).
3.4 Others’ Input in the Decision-Making Process—Patient Engagement
Most participants discussed how engaged they felt in their decision making (n = 68/72, 94.4%), and reported this to be an important part of the decision-making process (n = 63/68, 92.6%). However, the level of engagement and autonomy demonstrated by participants varied, from relying solely on their doctor’s advice, consulting family/friends/other patients to conducting independent research (Online Resource 4, see ESM). HCP interviews mirrored this finding, with some noting that younger PLwRMS were often more engaged and more likely to conduct their own research than older PLwRMS.
“I think we did it in sort of, you know, collaboration… that's the important thing about having a good relationship with your neurologist is that you can have these types of conversations, right.” (41-M-27-CAN)
“I think they do a lot of sort of internet reading as well because you know everyone wants to be autonomous and … not just listen to a doctor but find out information for themselves, I think to various degrees of kind of success.” (02-HCP-NEURO-UK)
3.5 Administration of Disease-Modifying Therapy (DMT)—Mode of Administration
Participants (n = 55/67, 78.9%) described mode of administration as an important consideration when making treatment decisions, with preference largely informed by previous experience. Both patient and HCP findings highlighted convenience and ease of use of oral treatments to be a key perception informing preference. HCPs further reported these features were particularly important to younger PLwRMS, as treatments would have less impact on their daily life. For participants who preferred injections and infusions, frequency of administration, efficacy and perceived convenience were considered key features.
“…right away I knew I didn’t want to get an injection, so that was an easy no and then the symptoms of the other medication, um, I didn’t like them, um, as much—like they were more of a put-off for me, so just through going through those three options, um, I made the decision by the process of elimination of things that I was looking for.” (41-M-27-CAN)
“I think administration is important for the patient, there’s no doubt about it, it kind of links into kind of lifestyle. There are some who are just very keen to have an oral tablet and not something more, you know not something more kind of severe.” (05-HCP-NEURO-UK)
Participants’ previous experiences with needles (n = 52/72, 72.2%) were described to influence the importance of mode of administration when making a treatment decision. Participants with positive needle experiences (n = 32/52, 61.5%) did not view the use of needles in administration to be an important consideration. Those with negative experiences stated that administering treatment via needles would stop them from taking such a treatment (n = 20/52, 38.2%) due to the thought of having to self-administer the treatment (n = 8/20, 40.0%) or fear of the invasiveness of an injection whether that be subcutaneous or intravenous (n = 8/20, 40.0%).
3.6 Efficacy of DMT—Speed of Effect
When exploring preferences regarding DMT efficacy, the speed of treatment effect was a differentiating factor amongst participants. Participants who described speed of effect to be an important consideration in treatment selection (n = 25/37, 67.6%), reported a desire to see their treatment working (i.e. by seeing or feeling an improvement in their symptoms) within 2 months of starting it, whereas participants who felt speed of effect was less important (n = 12/37, 32.4%) were less concerned, provided the treatment worked eventually. This finding was consistent with reports from HCPs. Most patients reporting speed of effect to be important were from Australia (n = 12/25, 48.0%).
“You don’t want to have to be… on it for years before you see an effect because especially with MS, it's… degenerative so you really want it to start working as soon as possible” (36-F-32-USA)
3.7 Side Effects—Reproduction and Parenthood
Side effects of treatments related to reproduction and parenthood led to most variability amongst participants (n = 56/72, 77.7%). For participants who already had children, or who weren’t planning to reproduce, this specific side effect was often not considered (n = 31/56, 55.4%). Most of those who reported potential impact on reproduction as an important consideration (n = 25/56, 44.6%), explained that they would like to have children in the future and would not want a treatment to impact that. Of these, 88.0% (n = 22/25) were females and the majority were either from the US (n = 9/25, 36.0%) or UK (n = 8/25, 32.0%). This finding was consistent with reports from HCPs.
“I did not take… treatment until after I had my… child… I didn’t want that in my system if I was going to be having babies” (32-F-50-USA)
3.8 HRQoL Impact—Impact on Work/Social Life
Participants were also asked to consider the broader impact a treatment may have on their HRQoL, with impact on work and social lives having most variability in responses (n = 57/72, 79.2%). Working participants commonly discussed having to take time off work (n = 33/57, 57.9%), to either receive treatment or as a result of side effects of treatment. Most participants discussing this as important were from the UK (n = 15/33, 45.5%). Those who were either not working or had not taken time off work due to treatment (n = 24/57, 42.1%) considered this less important. Previous experience of treatments negatively impacting social lives, such as having to miss social commitments (including hobbies, events with family/friends) or not wanting to be around others (n = 24/57, 42.1%), due to treatment administration or treatment side effects, informed preferences. HCPs echoed these findings and highlighted that frequency of treatment could also influence PLwRMS’ HRQoL.
“I couldn’t do it when it was going to interfere with work because I was quite concerned… about number of sick days and things” (10-F-36-UK)
“The betaferon would stop me going out so much or doing stuff because of the aches and pains in the muscles that I was always experiencing and the joints.” (57-M-44-AUS)
“Whether it’s a daily treatment, a weekly treatment, a monthly treatment an annual treatment, um, that might interfere with their work schedule, life schedule.” (07-HCP-NURSE-CAN)
3.9 Financial Impact—Cost of Treatment
Treatment cost was an important consideration for half of participants asked (n = 34/68, 50.0%). For those living in the US (n = 14/34, 41.2%), Canada (n = 9/34, 26.4%) and Australia (n = 7/34, 20.6%), treatment cost was described in relation to insurance coverage, work status and income. HCPs reported consistent findings. Despite not having to pay for treatment in the UK, four participants described the importance of cost from a societal perspective, in terms of the cost to the NHS, or the financial implications of missed workdays due to treatment (n = 4/34, 11.8%). Participants who did not consider treatment cost to be an important consideration were those who had treatment covered by their insurance provider (n = 22/34, 64.7%) or healthcare provider (n = 12/34, 35.3%; all UK).
“I was never planning on paying out-of-pocket for a treatment. I know I cannot do that… The worry for me is what the insurance would pay for.” (33-F-46-USA)
“They do not want to bankrupt their family financially and leave that as what they would always remember.” (02-HCP-NURSE-US)
3.10 Patient Descriptions of Ideal Treatment
During the interview, participants were asked to describe their ideal treatment in terms of mode and frequency of administration (Online Resource 4, see ESM). Preference for mode of administration was largely informed by current or previous treatment experiences and oral treatments were most frequently preferred. However, all participants reported that reduced frequency of administration was also a key feature to consider, as it determined the level of impact a treatment had on participants’ daily lives. Preferred frequency of administration ranged from once only (n = 6/58, 10.3%), daily (n = 20/58, 34.5%), weekly (n = 5/58, 8.6%), monthly (n = 13/58,22.4%), between 2–4 times a year (n = 8/58, 13.8%), to once a year (n = 6/58, 10.3%), thus highlighting the subjective and individual nature of treatment-related preferences in MS.
Participants were also asked to report the three most important features of a treatment when making treatment decisions, however some participants reported less than three (Fig. 3). Side effects (n = 48/72, 66.7%), efficacy (n = 38/72, 52.8%) and mode of administration (n = 13/72, 18.1%) were the most frequently reported features of treatment. These findings were largely consistent with HCP reports, although HCPs considered impact on daily life (n = 8/12, 66.7%) to be more important to participants than mode of administration (n = 6/12, 50.0%). These findings reiterate the variability in which features are deemed important to PLwRMS.
4 Discussion
Previous patient preference research has aimed to evaluate the relative importance of different features of DMT treatments [4, 21, 24, 26,27,28], including the importance of communication and patient engagement in decision-making specifically from the patient perspective [14, 29]. However, the reasons why PLwRMS may have preferences for certain features over others had yet to be explored, in particular from the patient perspective. The current study aimed to address this and better understand what drives RMS treatment preferences from the patient perspective [24]. In addition, in recognition that decisions regarding RMS treatment are agreed between patients and HCPs, insights were also obtained from 12 HCPs who treat/manage PLwRMS help to contextualize the patient interview findings.
A diverse sample of 72 PLwRMS was recruited, as demonstrated by the core demographic (age; gender) and clinical characteristics (experience of DMTs) [42]. Evidence of data saturation provides confidence that those concepts most relevant and important to participants had been identified and discussed. Consistent with previous patient preference studies [4, 14, 21, 24, 29], the concepts most frequently reported by participants (≥75% of the sample) as considerations when making a treatment decision were HCP input, patient engagement in decision making, mode of administration and efficacy. Previous research frequently reports efficacy to be the leading preference factor for PLwRMS [43], however the current study adds additional support that patient perceptions of efficacy can also be subjective in nature [28] and highlights the importance of employing a multi-faceted approach and perspective when exploring patient preferences [44].
Understandably, previous experiences of treatment largely informed preferences for mode and frequency of administration, and the severity and duration of side effects a participant was willing to endure. Participants’ personal circumstances, such as their current work status, social life, family commitments or desire to start a family, also played a key role. RMS occurs most commonly among women of child-bearing age and findings from this study reinforce the importance of such considerations on treatment decisions among this population [28, 29, 45]. However, the reasons provided for why participants placed more importance on some factors than others in their decision-making process was varied and this variability demonstrates the individualized nature of treatment decisions and the subjective relative importance placed on different factors by PLwRMS.
Some of the variation observed in participant perspectives may be explained by geographical differences. For example, cross-country differences were found with regards to the impact of treatment costs or insurance coverage on treatment decisions. Nearly half of all patients discussing the importance of the impact of treatment on work were from the UK. Given that patients in the UK did not have to pay for their treatment, it suggests that there is variability in the types of impacts on work that patients consider to be important, other than the expected financial repercussions. No major cross-country differences were identified for patient preferences regarding patient engagement and mode of administration. This may be due to the countries included being of the Western world and of arguably similar economic stability. The literature has indicated that patients from cultures where there is emphasis on family obligation and solidarity are likely to prefer to involve their families in their medical decision-making, compared with those from cultures where there is emphasis on independence and patient autonomy [46]. Similarly, it has been found that patients from less developed countries place greater influence on the mode of administration, and in particular injections, in their treatment decisions as these are perceived to be more efficacious than other modes [47]. Nonetheless, it is also acknowledged that these perspectives are also individualized in their nature and can vary within similar cultures [46]. The study findings therefore demonstrate that while certain similarities may exist in Western populations, particularly for those with similar healthcare systems, there is no one treatment deemed ‘ideal’ by most PLwRMS.
Current national treatment guidelines [15,16,17,18,19,20] acknowledge the importance of the treatment-specific factors outlined above when considering and discussing treatment choices with PLwRMS. However, the broader, holistic approach of considering a patient’s individual circumstances and experiences is limited [25]. There are decision aids available to help inform these decisions; however, there does not appear to be clear guidance on how and where these can be accessed and how they differ by country [14]. Acknowledging the inability to predict the course of the disease, as well as the inherent variability of patient preferences towards treatment, will ensure that the most appropriate treatment pathway is chosen for each person with MS. HCPs echoed this point in the current study, highlighting the link between personalized treatment pathways and higher adherence to treatment. Previous research has indicated how important patient engagement is to establish a personalized treatment pathway at the initial stage of starting treatment and during the decision to switch [14, 28, 48]. Potential revisions to treatment guidelines should be considered to reflect the shift towards evidence-based medicine, that is, the incorporation of patient preferences alongside clinical evidence [31]. To encourage these discussions in clinical practice, guidelines could also include information on how to discuss such topics with PLwRMS, ultimately leading to more personalized treatment pathways.
The reports by HCPs that younger PLwRMS play a more active role in the decision-making process, as they are more likely to conduct independent research, builds on the previous evidence by demonstrating that there is also variability in patient preferences regarding who patients are engaged with, and how, in making these decisions. Considering the global average age of an MS diagnosis is in the early 30s [49], the majority of patients in this study could be regarded as older patients. This may explain why a higher proportion of patients preferred to discuss their treatment options with their doctor as opposed to conducting their own research and why less than half the sample reported considering the impact of reproduction as an important consideration in their decisions.
A limitation of the study was the use of an able-bodied patient sample only. Further research may be needed to explore the experiences of PLwRMS with higher levels of disability and with disease forms with worse outcomes, such as progressive MS, as they have a much more limited range of DMT choice [50] and their experiences and treatment preferences may differ substantially to able-bodied patients. Additionally, the research was conducted in westernized cultures, leading to potential cultural bias of the findings. Although the current findings highlighted the personalized nature of treatment preferences, it is anticipated that cultural identity and levels of access to MS specialist centers may also play a role when considering treatment decisions, particularly in those who decide not to take or stop taking a treatment. Future research could explore preferences within countries of varying cultural identities and should note the geographical location of participants and the levels of access participants have to MS specialist centers. Some concepts were not always discussed during the interviews due to time limitations. However, data saturation was achieved and the nature of RMS meant that interviews longer than 60 minutes may have exacerbated participants’ fatigue, which can be worsened by sustained cognitive effort [51] and tends to peak in the late afternoon [52]. This study was conducted during the COVID-19 pandemic which may have influenced participants’ responses. To mitigate this risk, interviewers probed participants if they spontaneously reported that their treatment preferences had changed because of COVID-19. This was then accounted for during data analysis whereby any preferences which had changed because of COVID-19 were coded and reported as separate concepts.
5 Conclusion
Concurrent with best practice guidelines [15,16,17,18,19,20], the study highlights the importance of qualitative work as an integral component of patient preference studies to gain a deeper understanding of what drives patient preferences. Qualitative patient preference evidence could offer valuable and supplementary insights, alongside quantitative data, to inform reimbursement and regulatory approval decisions made by HTA bodies and regulators, particularly when a treatment is indicated for a heterogenous population such as RMS.
References
Olek MJ, Narayan RN, Frohman EM, Frohman TC (2018) Clinical features of multiple sclerosis in adults. UpToDate. UpToDate, Waltham, MA. Accessed 2 Apr 2018.
Stadelmann C, Wegner C, Brück W. Inflammation, demyelination, and degeneration—recent insights from MS pathology. Biochim Biophys Acta (BBA) Mol Basis Dis. 2011;1812(2):275–82.
Confavreux C, Vukusic S, Moreau T, Adeleine P. Relapses and progression of disability in multiple sclerosis. N Engl J Med. 2000;343(20):1430–8.
Bottomley C, Lloyd A, Bennett G, Adlard N. A discrete choice experiment to determine UK patient preference for attributes of disease modifying treatments in multiple sclerosis. J Med Econ. 2017;20(8):863–70.
Desborough J, Brunoro C, Parkinson A, et al. ‘It struck at the heart of who I thought I was’: a meta-synthesis of the qualitative literature examining the experiences of people with multiple sclerosis. Health Expect. 2020;23(5):1007–27.
Moriya R, Suzuki S. A qualitative study relating to the experiences of people with MS: differences by disease severity. Br J Neurosci Nurs. 2011;7(4):593–600.
Ploughman M, Austin MW, Murdoch M, Kearney A, Godwin M, Stefanelli M. The path to self-management: a qualitative study involving older people with multiple sclerosis. Physiother Can. 2012;64(1):6–17.
Pardo G, Jones DE. The sequence of disease-modifying therapies in relapsing multiple sclerosis: safety and immunologic considerations. J Neurol. 2017;264(12):2351–74.
McKay KA, Tremlett H, Patten SB, et al. Determinants of non-adherence to disease-modifying therapies in multiple sclerosis: a cross-Canada prospective study. Mult Scler J. 2017;23(4):588–96.
Ibrahim F, Deleu D. Assessment of non-adherence of multiple sclerosis patients to medication and follow up clinic. Health Sci J. 2018;12(2):1–5.
Nicholas JA, Edwards NC, Edwards RA, Dellarole A, Grosso M, Phillips AL. Real-world adherence to, and persistence with, once-and twice-daily oral disease-modifying drugs in patients with multiple sclerosis: a systematic review and meta-analysis. BMC Neurol. 2020;20(1):1–15.
Li P, Ladage VP, Berger J, et al. Disease-modifying therapy adherence and associated factors in a national sample of Medicare patients with multiple sclerosis. Value Health. 2020;23(3):328–34.
Kołtuniuk A, Rosińczuk J. Adherence to disease-modifying therapies in patients with multiple sclerosis. Patient Prefer Adherence. 2018;12:1557.
Manzano A, Eskytė I, Ford HL, Bekker HL, Potrata B, Chataway J, Pavitt SH. Impact of communication on first treatment decisions in people with relapsing-remitting multiple sclerosis. Patient Educ Couns. 2020;103(12):2540–7.
NICE. Multiple Sclerosis Treatment Summary. https://bnf.nice.org.uk/treatment-summary/multiple-sclerosis.html. Accessed.
NICE. Multiple Sclerosis Pathway. https://pathways.nice.org.uk/pathways/multiple-sclerosis#path=view%3A/pathways/multiple-sclerosis/managing-multiple-sclerosis.xml&content=view-index. Accessed.
Broadley SA, Barnett MH, Boggild M, et al. Therapeutic approaches to disease modifying therapy for multiple sclerosis in adults: an Australian and New Zealand perspective Part 3 Treatment practicalities and recommendations. J Clin Neurosci. 2014;21(11):1857–65.
Tsang BK, Macdonell R. Multiple sclerosis: diagnosis, management and prognosis. Aust Fam Physician. 2011;40(12):948–55.
Freedman MS, Devonshire V, Duquette P, et al. Treatment optimization in multiple sclerosis: Canadian MS Working Group recommendations. Can J Neurol Sci. 2020;47(4):437–55.
Rae-Grant A, Day GS, Marrie RA, et al. Practice guideline recommendations summary: disease-modifying therapies for adults with multiple sclerosis: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology. Neurology. 2018;90(17):777–88.
van Eijndhoven E, Brauer M, Kee R, et al. Modeling the impact of patient treatment preference on health outcomes in relapsing-remitting multiple sclerosis. J Med Econ. 2020;23(5):474–83.
FDA. Patient preference information—voluntary submission, review in premarket approval applications, humanitarian device exemption applications, and de novo requests, and inclusion in decision summaries and device labeling. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-preference-information-voluntary-submission-review-premarket-approval-applications. Accessed 2016.
FDA. Developing and submitting proposed draft guidance relating to patient experience data draft guidance. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/developing-and-submitting-proposed-draft-guidance-relating-patient-experience-data. Accessed 2018.
Webb EJ, Meads D, Eskyte I, et al. A systematic review of discrete-choice experiments and conjoint analysis studies in people with multiple sclerosis. Patient-Patient-Centered Outcomes Res. 2018;11(4):391–402.
England N. Treatment algorithm for multiple sclerosis disease-modifying therapies. https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2019/03/Treatment-Algorithm-for-Multiple-Sclerosis-Disease-Modifying-Therapies-08-03-2019-1.pdf. Published 2018. Accessed.
Wilson L, Loucks A, Bui C, et al. Patient centered decision making: Use of conjoint analysis to determine risk–benefit trade-offs for preference sensitive treatment choices. J Neurol Sci. 2014;344(1–2):80–7.
Bayas A, Mäurer M. Teriflunomide for the treatment of relapsing–remitting multiple sclerosis: patient preference and adherence. Patient Prefer Adherence. 2015;9:265.
Eskyte I, Manzano A, Pepper G, Pavitt S, Ford H, Bekker H, Potrata B. Understanding treatment decisions from the perspective of people with relapsing remitting multiple sclerosis: a critical interpretive synthesis. Mult Scler Relat Disord. 2019;27:370–7.
Manzano A, Eskyté I, Ford HL, Pavitt SH, Potrata B, Schmierer K, Bekker HL. Patient perspective on decisions to switch disease-modifying treatments in relapsing-remitting multiple sclerosis. Mult Scler Relat Disord. 2020;46:102–507.
Bouvy JC, Cowie L, Lovett R, Morrison D, Livingstone H, Crabb N. Use of patient preference studies in HTA decision making: a NICE perspective. Patient-Patient-Centered Outcomes Res. 2020;13(2):145–9.
Marsh K, van Til JA, Molsen-David E, Juhnke C, Hawken N, Oehrlein EM, Muehlbacher A. Health preference research in Europe: a review of its use in marketing authorization, reimbursement, and pricing decisions—report of the ISPOR Stated Preference Research Special Interest Group. Value Health. 2020;23(7):831–41.
SMC. Patient and clinician engagement (PACE) meetings overview. https://www.scottishmedicines.org.uk/media/5423/pace-overview-document-v32.pdf. Accessed.
Cowie L, Bouvy J. Measuring patient preferences: an exploratory study to determine how patient preferences data could be used in health technology assessment (HTa). Myeloma UK, 2019. https://www.myeloma.org.uk/wp-content/uploads/2019/07/NICE-Patient-Preferences-Report.pdf. Accessed June 2019.
Van Overbeeke E, Forrester V, Simoens S, Hays I. Use of patient preferences in health technology assessment: perspectives of canadian, belgian, and german HTA representatives. Patient Patient-Cent Outcomes Res. 2021;14:119–28.
Humphrey L, Willgoss T, Trigg A, et al. A comparison of three methods to generate a conceptual understanding of a disease based on the patients’ perspective. J Patient Rep Outcomes. 2017;1(1):9. https://doi.org/10.1186/s41687-017-0013-6.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Kerr C, Nixon A, Wild D. Assessing and demonstrating data saturation in qualitative inquiry supporting patient-reported outcomes research. Expert Rev Pharmacoecon Outcomes Res. 2010;10(3):269–81.
Thompson J. A guide to abductive thematic analysis. Qual Rep. 2022;27(5):1410–21. https://doi.org/10.46743/2160-3715/2022.53405340.
Francis JJ, Johnston M, Robertson C, et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health. 2010;25(10):1229–45.
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82.
Lamoureux R, Shields A, Stokes J, Yaworsky A, Galipeau N. How many subjects are enough for symptom-focused concept elicitation studies? A retrospective analysis of saturation across twenty-six studies. Value Health. 2015;18(3):A33.
Ascherio A, Munger KL. Epidemiology of multiple sclerosis: from risk factors to prevention—an update. Semin Neurol. 2016;36(2):103–14.
Brown H, Gabriele S, White J. Physician and patient treatment decision-making in relapsing-remitting multiple sclerosis in Europe and the USA. Neurodegener Disease Manag. 2018;8(6):371–6.
Miller DM, Moss B, Rose S, Li H, Schindler D, Weber M, Planchon SM, Alberts J, Boissy A, Bermel R. Obtaining patient priorities in a multiple sclerosis comprehensive care center: beyond patient-reported outcomes. J Patient Exp. 2020;7(4):541–8.
Webb EJD, Meads D, Eskytė I, Ford HL, Bekker HL, Chataway J, Pepper G, Marti J, Okan Y, Pavitt SH, Schmierer K, Manzano A. The impact of reproductive issues on preferences of women with relapsing multiple sclerosis for disease-modifying treatments. Patient. 2020;13(5):583–97. https://doi.org/10.1007/s40271-020-00429-4.
Alden DL, Friend J, Lee PY, Lee YK, Trevena L, Ng CJ, Limpongsanurak S. Who decides: me or we? Family involvement in medical decision making in eastern and western countries. Med Decis Mak. 2018;38(1):14–25.
Reeler AV. Anthropological perspectives on injections: a review. Bull World Health Org. 2000;78(1):135–43.
Rieckmann P, Boyko A, Centonze D, Elovaara I, Giovannoni G, Havrdová E, Hommes O, Kesselring J, Kobelt G, Langdon D, LeLorier J. Achieving patient engagement in multiple sclerosis: a perspective from the multiple sclerosis in the 21st Century Steering Group. Mult Scler Relat Disord. 2015;4(3):202–18.
The Multiple Sclerosis International Federation, Atlas of MS, 3rd edition (September 2020).
Feinstein A, Freeman J, Lo AC. Treatment of progressive multiple sclerosis: what works, what does not, and what is needed. Lancet Neurol. 2015;14(2):194–207.
Berard JA, Smith AM, Walker LA. A longitudinal evaluation of cognitive fatigue on a task of sustained attention in early relapsing-remitting multiple sclerosis. Int J MS Care. 2018;20(2):55–61.
Powell DJ, Liossi C, Schlotz W, Moss-Morris R. Tracking daily fatigue fluctuations in multiple sclerosis: ecological momentary assessment provides unique insights. J Behav Med. 2017;40(5):772–83.
Acknowledgements
The authors would like to acknowledge and thank Danny Nuttall and Adam Gater (Adelphi Values) for their valuable input and contributions to the study. They would also like to express thanks to the patients and healthcare professionals for taking part in the study. No medical writing or editorial assistance was used or provided.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest/competing interests
The research was conducted by Adelphi Values Patient-Centered Outcomes who received funding from Novartis Pharma AG to complete this work. Some of the authors are salaried employees of Novartis Pharma AG.
Funding
The research was conducted by Adelphi Values Patient-Centered Outcomes who received funding from Novartis Pharma AG to complete this work.
Ethics approval
The study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by Western Independent Review Board® (WIRB).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Participants signed informed consent regarding publishing their anonymized data.
Availability of data and material
All data generated or analyzed during this study are included in this published article (and its supplementary information files). The data that support the findings of this study are available from Novartis, but restrictions apply to the availability of these data, which were used under licence for the current study and so are not publicly available.The data are, however, available from the authors upon reasonable request and with the permission of Novartis.
Code availability
Not applicable.
Author contributions
Adelphi Values authors (AB, ST, KS, WN and CF) contributed to the study design, data collection, interpretation of data, and preparation of the manuscript for publication. All other authors (CL, RB, NA and TB) contributed to defining the scope of the research, including study design; and interpretation of study results in the manuscript. All authors reviewed and approved this manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tatlock, S., Sully, K., Batish, A. et al. Individual Differences in the Patient Experience of Relapsing Multiple Sclerosis (RMS): A Multi-Country Qualitative Exploration of Drivers of Treatment Preferences Among People Living with RMS. Patient 16, 345–357 (2023). https://doi.org/10.1007/s40271-023-00617-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-023-00617-y