Abstract
Background
Ponesimod is a potent selective sphingosine-1-phosphate receptor 1 (S1P1) modulator, which leads to a reduction in circulating lymphocytes, reflecting their sequestration within lymphoid organs. Modulation of the S1P1 receptor has been previously described to be an effective treatment of autoimmune diseases (e.g., multiple sclerosis).
Objectives
The aim of this study was to compare the relative bioavailability of two polymorphic forms of ponesimod in capsules (Form A versus Form C; Study 1) and the relative bioavailability of a capsule formulation and a tablet formulation (both polymorphic Form C; Study 2).
Methods
Two open-label, randomized, two-way crossover studies in healthy subjects were performed. In Study 1, 12 male subjects received a single dose of 20 mg of polymorphic Form A or Form C of ponesimod in a capsule. In Study 2, 14 male and female subjects (ratio 1:1) received a single dose of 40 mg of polymorphic Form C of ponesimod in either a capsule or a tablet formulation. Pharmacokinetic and safety variables (clinical laboratory test results, vital signs, and an electrocardiogram) were assessed.
Results
Comparison of the exposure to ponesimod following administration of the formulations in Study 1 showed that the 90 % confidence intervals of the geometric mean ratios for the area under the curve from time zero to infinity (AUC0–inf), the area under the curve from time zero to the time of the last measurable concentration (AUC0–t), the terminal half-life (t ½), and the maximum plasma concentration (C max) were all within the 0.80–1.25 bioequivalence interval. In Study 2, more rapid absorption of ponesimod was observed from the tablet formulation than from the capsule formulation. There were no relevant differences in the safety and tolerability profiles between the different formulations.
Conclusion
The two polymorphic forms of ponesimod and tablet versus capsule formulations were similar in terms of pharmacokinetics, safety, and tolerability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The pharmacokinetics of a single oral dose of two polymorphic forms (Form A versus Form C) of ponesimod in capsules and a tablet formulation (Form C) were compared. |
Comparison between the two polymorphic forms and comparison between the capsule and tablet formulations did not reveal relevant differences in pharmacokinetic and safety properties. |
Capsules can be substituted with tablets, from which ponesimod is absorbed slightly more rapidly. |
1 Introduction
Sphingosine-1-phosphate (S1P) is a phospholipid displaying a wide range of physiological roles [1–3]. S1P effects are mediated by the activation of five G-protein-coupled receptors, S1P1 to S1P5. Among them, the S1P1 receptors, which are expressed in many cell types (e.g., lymphocytes, cardiomyocytes, and endothelial cells), induce G αi protein-mediated signaling and play a role in the immune and cardiovascular systems [4]. Recent studies have revealed that functional antagonism of the S1P1 receptor leads to inhibition of the egress of lymphocytes from secondary lymphoid organs and a low lymphocyte count in peripheral blood [5].
Ponesimod (ACT-128800) is a potent, orally active, selective, reversible S1P1 receptor modulator [6] currently in clinical development for the treatment of autoimmune diseases and has successfully reached its study end points in recent phase II trials in patients with chronic plaque psoriasis [7] or relapsing–remitting multiple sclerosis [8]. Single- and multiple-dose administration of ponesimod results in a dose-dependent decrease in circulating lymphocytes in healthy subjects and is associated with heart rate reduction, a delay in atrioventricular conduction, and pulmonary effects [9–13].
The maximum plasma concentration (C max) is achieved approximately 2–4 h after dosing (t max), and the terminal half-life (t ½) is approximately 32 h. Steady-state conditions are attained within 4–5 days when ponesimod is administered once daily at any given dose. Increases in C max are dose proportional, while increases in the area under the curve (AUC) are slightly greater than dose proportional [9–11]. A previous study [9] revealed low variability in pharmacokinetic parameters (inter-subject variability <36 %). Previous clinical trials were performed with polymorph Form A (a hydrated crystalline form) of ponesimod capsules. During the development of the drug, solid-state investigations revealed the existence of distinct polymorphic forms of ponesimod. Form C (an anhydrous polymorphic form)—the thermodynamically most stable form at room temperature so far known—was identified. Moreover, a tablet formulation of Form C with a smaller size, compared with the capsules, was developed.
The aim of this study was to compare the two polymorphic forms (Form A and Form C in capsules), as well as the capsule and tablet formulations of Form C of ponesimod, in terms of their pharmacokinetics, safety, and tolerability, in order to bridge the results obtained in early clinical studies using capsules of Form A with those of later studies.
2 Methods
2.1 Subjects
Healthy male and female subjects aged between 18 and 65 years were included in this study. The health of the subjects was assessed at the screening visit, which included recording of the medical history, medications taken during the 3 months preceding the screening visit, a physical examination, measurement of body weight and height, clinical laboratory tests, recording of vital signs, and a standard electrocardiogram (ECG). Because of the teratogenic potential of ponesimod, women of childbearing potential were required to use two reliable and protocol-approved methods of contraception from screening until 2 months after the last study drug intake. At screening, subjects had to have a PR interval of <200 ms, a heart rate of >55 beats per minute (bpm), and a total lymphocyte count of >1000 lymphocytes/µL. Written informed consent was obtained from each individual participating in the study prior to any study procedure and after adequate explanation of the aims, methods, objectives, and potential hazards of the studies. These studies were conducted at different centers and at different times. The Comité de Protection des Personnes (Paris, France) approved the protocol of Study 1, and the Aspire Institutional Review Board (La Mesa, CA, USA) approved the protocol of Study 2. These studies were performed according to good clinical practice and in accordance with the principles of the Declaration of Helsinki.
2.2 Study Design
This work was performed at two centers, one in France for the comparison of polymorphic Form A and Form C in capsules (Study 1) and one in the USA for the comparison between capsules and tablets of Form C (Study 2). Each study was a single-center, randomized, open-label, two-period, two-treatment, crossover, biocomparison study. A total of 26 subjects (12 healthy male subjects in Study 1: age 31.3 [±12.8] years, body weight 75.4 [±11.3] kg; 14 healthy male and female subjects [ratio 1:1] in Study 2: age 31.1 [±14.9] years, body weight 69.0 [±14.5] kg) were enrolled, and all subjects received active treatment. A power of 80 % was estimated with a sample size of 12 subjects (in Study 1) and 14 subjects (in Study 2), based on an intra-subject coefficient of variation of the tablet formulation of ~12 % observed in previous clinical trials of ponesimod. The treatment consisted of two treatment periods of a single dose of ponesimod 20 mg as one Form A or Form C capsule (in Study 1) or two treatment periods of a single dose of ponesimod 40 mg either as one capsule or one tablet (in Study 2). These doses have been used in phase II trials [7, 8]. All treatments were administered in the morning with approximately 240 mL of water, and the two treatment periods were separated by a wash-out period of 8–15 days in Study 1 and 14–15 days in Study 2. The subjects remained fasted from at least 10 h prior to drug intake until 4 h afterward. The subjects remained in the clinic from day −1 (i.e., the day prior to study drug administration) until day 2, 24 h after study drug administration, and they could then be discharged if this was allowed on the basis of their medical condition at the end of each treatment period. An end-of-study visit comprising the same examinations as those performed at the screening visit was conducted 6 days or 22 (+2) days after the last study drug administration in Study 1 and Study 2, respectively.
2.3 Safety and Tolerability Assessments
Safety and tolerability were evaluated by monitoring of adverse events and vital signs (supine blood pressure and heart rate), a cardiodynamic assessment (a 12-lead ECG recording), pulmonary function tests, clinical laboratory tests, and physical and neurological examinations.
Vital signs were recorded from subjects in the supine position after they had rested for at least a 5-min period pre-dose and 1, 2.5, 4, 10, 24, 48, and 144 h after study drug administration in both Study 1 and Study 2. In Study 1, vital signs were, in addition, recorded 0.5, 1.5, 6, 36, 72, 96, and 120 h after study drug administration. A standard 12-lead ECG was recorded at rest in the supine position pre-dose and 1, 2.5, 4, 10, 24, 48, and 144 h after study drug administration in both studies. Clinical laboratory tests and a physical examination were done prior to study drug administration and during the end-of-study visit.
2.4 Pharmacodynamic Assessments
A lymphocyte count was only performed pre-dose and 144 h after ponesimod administration in Study 2. Two additional assessments (24 and 48 h after study drug administration) were performed in Study 1.
2.5 Pharmacokinetic Assessments and Analysis
Blood samples of about 3 mL were collected in ethylenediaminetetraacetic acid (EDTA) tubes just before study drug administration and 0.5, 1, 1.5, 2.5, 4, 6, 10, 16, 24, 36, 48, 72, 96, 120, and 144 h after study drug administration in both Study 1 and Study 2. After centrifugation, plasma was transferred into a labeled polypropylene tube and stored at −21 °C (±5 °C) pending analysis. Plasma concentrations of ponesimod were determined using a validated liquid chromatography–tandem mass spectrometry (LC–MS/MS) assay with a lower limit of quantification of 1 ng/mL [9]. Analysis of quality-control samples of all runs showed that the inter-day coefficients of variation were <12.2 %, whereas the average intra-day inaccuracy was in the range of −6.0 to 3.3 %. Noncompartmental pharmacokinetic analyses were performed using Professional WinNonlin 6.1 software (Pharsight Corp., Mountain View, CA, USA). The variables C max and t max were directly read from the plasma concentration–time profiles, AUC from time zero to the time of the last measurable concentration (AUC0–t) was calculated using the trapezoidal method [14], and t ½ was calculated as ln 2/λz, where λz is the terminal elimination rate constant estimated by log-linear regression analysis. Pharmacokinetic variables were analyzed descriptively, providing geometric means and 95 % confidence intervals (CIs) for C max, AUC from time zero to infinity (AUC0–inf), AUC0–t (i.e., AUC from time zero to 144 h [AUC0–144h]), and t ½. For t max, the median with minimum and maximum values were calculated and reported.
2.6 Statistical Analysis
Safety and tolerability data were analyzed descriptively. Bioequivalence was explored, and the geometric mean ratios of AUC and C max of Form C/Form A and tablet/capsule, as well as their 90 % CIs, were derived from mixed-effect models with treatment, sequence, and period as fixed effects and subjects as random effects, and by a linear model with treatment and subjects as fixed effects. Differences in t max were explored using the nonparametric Wilcoxon signed-rank test.
SAS® software versions 8.2 and 9.1 (SAS Institute, Cary, NC, USA) were used for the statistical analysis and the reporting of safety and tolerability data. For the pharmacokinetics, the statistical package R (R Foundation for Statistical Computing Version 2.6.1, lme function) was used. Cardiodynamic and pharmacodynamic data are expressed as mean ± standard deviation (SD). The Student’s t test was used to analyze the effects of ponesimod on the heart rate and blood pressure. Differences were considered to be statistically significant at p < 0.05.
3 Results
3.1 Pharmacokinetics
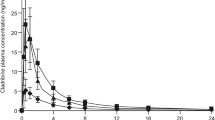
In Study 1, the plasma concentration–time profiles of ponesimod were characterized by a median t max of 4 h for both polymorphic forms in capsules (Fig. 1a; Table 1). Table 1 reveals that following ponesimod 20 mg, the observed total exposure, C max, and t ½ were similar with Form A and Form C. When bioequivalence was explored by mixed-effect and linear models, the geometric mean ratios (and 90 % CIs) of C max and AUC for Form C versus Form A capsules were all within the 0.80–1.25 bioequivalence interval (Fig. 2; Table 1).
Arithmetic mean (with standard deviation) plasma concentration–time profiles of ponesimod (left graphs from 0 to 144 h [with linear scales and semi-logarithmic scales shown as insets]; right graphs from 0 to 8 h) in healthy subjects after a single dose of a 20 mg as a Form A or Form C capsule (n = 12) or b 40 mg as a Form C capsule or tablet (n = 14)
Geometric mean ratios (with 90 % confidence intervals) derived from mixed-effect models of the area under the curve from time zero to the time of the last measurable concentration (AUC0–t), the area under the curve from time zero to infinity (AUC0–inf), and the maximum plasma concentration (C max) in Study 1 (comparison of the two polymorphic Forms C and A; n = 12) and in Study 2 (comparison of the tablet and capsule formulations; n = 14). The dotted lines represent the lower and upper bounds of the bioequivalence interval (0.80–1.25)
In Study 2, subjects received ponesimod 40 mg as either a tablet or a capsule of Form C. When both formulations were compared, total exposure and t ½ were similar (Table 1). C max was slightly higher and reached earlier with the tablet than with the capsule (Fig. 1b; Table 1), indicating more rapid absorption of ponesimod when administered in the tablet formulation. The 90 % CIs of the estimated geometric mean ratios of AUC0–t (AUC0–144h) and AUC0–inf were contained within the 0.80–1.25 bioequivalence interval. The estimated geometric mean ratio for C max was 27 % higher (i.e., ratio 1.27) with the tablet than with the capsule formulation (90 % CI 1.15–1.40), and t ½ tended to be slightly shorter with the tablet formulation (ratio 0.90, 90 % CI 0.77–1.05) (Fig. 2).
In Study 2, both male and female subjects (ratio 1:1) were enrolled. The observed C max was greater in female subjects (geometric means [95 % CIs] 251.4 [176.6–357.8] ng/mL and 326.8 [272.7–391.7] ng/mL for capsules and tablets, respectively) than in male subjects (160.1 [127.2–201.7] ng/mL and 199.4 [165.4–240.0] ng/mL for capsules and tablets, respectively). Moreover, exposure to ponesimod (AUC0–inf) was greater in female subjects (9841 [7292–13,280] ng·h/mL and 10,864 [8826–13,372] ng·h/mL for capsules and tablets, respectively) than in male subjects (6361 [4896–8264] ng·h/mL and 6543 [4947–8654] ng·h/mL for capsules and tablets, respectively), and t ½ was slightly longer in female subjects (37.1 [27.8–49.5] h and 31.2 [24.6–39.5] h for capsules and tablets, respectively) than in male subjects (26.3 [23.2–29.7] h and 25.2 [23.3–27.3] h for capsules and tablets, respectively).
3.2 Safety and Tolerability
No serious or severe adverse events occurred during these two studies. There was no marked difference in the nature, severity, and incidence of adverse events reported for the different formulations in Study 1 (Form A and Form C capsules) and Study 2 (Form C capsule and tablet) (Table 2). All reported adverse events were of mild to moderate intensity, were considered by the investigators to be related to the study drug, and were reported as being resolved by the end of the studies. In both studies, the most frequently observed adverse events were headache, dizziness, nausea, and sinus bradycardia (defined as a heart rate below 40 bpm), and three subjects (one in Study 1 and two in Study 2) displayed an event of first-degree atrioventricular block (defined as a PR interval above 200 ms). When comparing Study 1 and Study 2 (Table 2), the incidence of adverse events (i.e., the number of subjects with at least one adverse event) was higher following administration of ponesimod 40 mg (85.7 %) than following ponesimod 20 mg (33.3 %).
In Study 1, maximum heart rate changes of (mean ± SD) −20.2 ± 6.0 bpm (t = 9.2, p < 0.001) and −18.8 ± 5.6 bpm (t = 10.7, p < 0.001) 2.5 h after administration of Form A and Form C, respectively, were observed (Fig. 3a). There was no relevant difference between the two polymorphic forms of ponesimod (t = 0.6, p = 0.6).
Arithmetic mean (with standard deviation) heart rates from 0 to 144 h after administration of ponesimod at a dose of a 20 mg (Study 1; n = 12) or b 40 mg (Study 2; n = 14) in healthy subjects. The insets show the arithmetic mean heart rates (with standard deviations) from 0 to 10 h. bpm beats per minute
In Study 2, the maximum heart rate changes were (mean ± SD) −15.6 ± 10.6 bpm (t = 4.9, p < 0.0001) and −16.2 ± 6.4 bpm (t = 5.0, p < 0.0001) 2.5 h after administration of the capsule and tablet formulations, respectively (Fig. 3b). There was no relevant difference between the capsule and tablet formulations of Form C (t = 0.2, p = 0.9) (Fig. 3b).
A reduction in blood pressure, compared with baseline, following administration of both polymorphic forms of ponesimod (20 mg) was observed. However, no relevant differences were observed in the decrease in systolic and diastolic blood pressure between Form A (systolic: −7 ± 11 mmHg; diastolic: −10 ± 7 mmHg) and Form C (systolic: −6 ± 14 mmHg, t = 0.2, p = 0.8; diastolic: −8 ± 5 mmHg, t = 0.8, p = 0.4). In Study 2, both the capsule (systolic: −7 ± 9 mmHg; diastolic: −9 ± 8 mmHg) and the tablet (systolic: −6 ± 6 mmHg, t = 0.4, p = 0.7; diastolic: −7 ± 11 mmHg, t = 0.7, p = 0.5) formulations triggered similar decreases in blood pressure. The maximum decrease in blood pressure was observed 2.5 h after ponesimod administration in both Study 1 and Study 2.
In both studies, administration of ponesimod 20 or 40 mg did not alter other safety parameters, such as ECG variables (including the QTcB and QTcF intervals) and body weight. There were no marked differences regarding the number of ECG abnormalities in Study 1 (three ECG abnormalities were observed with each polymorphic form) or Study 2 (16 and 20 abnormalities were observed with the capsule and tablet, respectively). Thus, the frequency of abnormalities was higher following administration of ponesimod 40 mg than following ponesimod 20 mg.
As expected, a single administration of ponesimod 20 mg (mean ± SD decreases in the number of lymphocytes: −1.05 ± 0.50 × 109 cells/L and −0.95 ± 0.47 × 109 cells/L for Form A and Form C, respectively) or 40 mg (−0.30 ± 0.51 × 109 cells/L and −0.23 ± 0.27 × 109 cells/L for the capsule and tablet, respectively) led to a reduction in the lymphocyte count (not shown). This effect was not considered to be an adverse event, as it is an anticipated pharmacodynamic effect of the drug.
4 Discussion
The aim of the present study was to compare two polymorphic capsule forms, as well as comparing tablet and capsule formulations (of the same polymorphic form) of ponesimod, a potent S1P1 modulator.
The capsule and tablet formulations of ponesimod have similar concentration–time profiles and exposure, as well as t ½ values, though absorption of ponesimod from the tablet formulation was slightly more rapid, with a higher C max than that seen with the capsule formulation. The observed safety profile was comparable between the different formulations. Previous clinical studies were performed with ponesimod polymorphic Form A. This form is a crystalline solid obtained by rapid precipitation, whereas another formulation obtained by slow crystallization has been developed. This Form C is thermodynamically more stable than Form A. In addition, the slow crystallization of Form C in the final step of the synthesis is easier to control and more reproducible, especially on a large manufacturing scale, than the rapid precipitation that yields Form A. In addition, a tablet formulation has been developed, which is preferred to the capsule formulation, since the tablets are smaller and easier to swallow, which may improve patient compliance. It is worth noting that difficulties in swallowing are relatively frequent in patients with multiple sclerosis [15]. More importantly, tablets are generally more stable than capsules. In the present work, we have shown bioequivalence between the two polymorphic forms of ponesimod, and we observed slightly more rapid absorption of ponesimod when it was administered as tablet formulation. Therefore, ponesimod capsules can be substituted with tablets without any dose adjustment.
Between Study 1 and Study 2, the increases in C max were dose proportional and the increases in AUC were slightly greater than dose proportional, which is in line with the findings of previous clinical studies performed with ponesimod [8–11]. Whereas similar exposure in male and female subjects has been seen previously [10], the findings of a recent study [11] are in good agreement with the greater exposure in female subjects that was observed in the present work. This finding could be related to differences in body weight, requiring dose adjustment [16, 17].
In terms of safety and tolerability, a similar incidence and nature of adverse events was observed in Study 1 and Study 2. No new findings were observed, in comparison with previous studies [7–13]. The incidence of adverse events and the percentage of subjects displaying adverse events were dose dependent. In current phase II studies, an up-titration scheme (a first dose of 10 mg) is applied in patients to improve the safety and tolerability of ponesimod treatment [7, 8]. The lymphocyte nadir (maximum observed decrease) was higher following administration of ponesimod 20 mg than following 40 mg. This might have been related to the timing of the assessments. Indeed, in Study 2, the lymphocyte count was assessed pre-dose and 144 h after ponesimod administration. In Study 1, additional assessments were performed daily.
In good agreement with previous studies, we observed transient significant reductions in the heart rate and blood pressure following administration of ponesimod, which were induced by the activation of S1P1 [18]. The maximum decrease was observed 2.5 h after ponesimod administration, and the heart rate returned to baseline within 10 h, as previously observed [9–11]. When comparing Study 1 and Study 2, no clear dose-dependent effect was observed. This was also the case in a previous study, in which the decrease in the heart rate was similar in the 20 and 50 mg dose groups [9]. While comparison across studies has limitations, we may assume that the effect on the heart rate reaches a plateau with ponesimod 20 mg. This reduction in the heart rate following ponesimod administration is explained by the internalization of the S1P1 receptors and their desensitization. This effect has been well characterized for S1P modulators [18–20].
5 Conclusion
The two polymorphic forms of ponesimod and the tablet and capsule formulations were similar in terms of their pharmacokinetics, except for more rapid absorption of the tablet formulation than the capsule formulation. At the same dose, the strength, safety, and tolerability were similar. Therefore, Form A can be substituted with Form C, and capsules can be substituted with tablets.
References
Rivera J, Proia RL, Olivera A. The alliance of sphingosine-1-phosphate and its receptors in immunity. Nat Rev Immunol. 2008;8(10):753–63.
Spiegel S, Milstien S. Sphingosine-1-phosphate: an enigmatic signalling lipid. Nat Rev Mol Cell Biol. 2003;4(5):397–407.
Takuwa Y, Okamoto Y, Yoshioka K, Takuwa N. Sphingosine-1-phosphate signaling and biological activities in the cardiovascular system. Biochim Biophys Acta. 2008;1781(9):483–8.
Bigaud M, Guerini D, Billich A, Bassilana F, Brinkmann V. Second generation S1P pathway modulators: research strategies and clinical developments. Biochim Biophys Acta. 2014;1841(5):745–58.
Thangada S, Khanna KM, Blaho VA, Oo ML, Im DS, Guo C, et al. Cell-surface residence of sphingosine 1-phosphate receptor 1 on lymphocytes determines lymphocyte egress kinetics. J Exp Med. 2010;207(7):1475–83.
Bolli MH, Abele S, Binkert C, Bravo R, Buchmann S, Bur D, et al. 2-Imino-thiazolidin-4-one derivatives as potent, orally active S1P1 receptor agonists. J Med Chem. 2010;53(10):4198–211.
Vaclavkova A, Chimenti S, Arenberger P, Hollo P, Sator PG, Burcklen M, et al. Oral ponesimod in patients with chronic plaque psoriasis: a randomised, double-blind, placebo-controlled phase 2 trial. Lancet. 2014;384(9959):2036–45.
Olsson T, Boster A, Fernandez O, Freedman MS, Pozzilli C, Bach D, et al. Oral ponesimod in relapsing-remitting multiple sclerosis: a randomised phase II trial. J Neurol Neurosurg Psychiatry. 2014;85(11):1198–208.
Brossard P, Derendorf H, Xu J, Maatouk H, Halabi A, Dingemanse J. Pharmacokinetics and pharmacodynamics of ponesimod, a selective S1P1 receptor modulator, in the first-in-human study. Br J Clin Pharmacol. 2013;76(6):888–96.
Brossard P, Scherz M, Halabi A, Maatouk H, Krause A, Dingemanse J. Multiple-dose tolerability, pharmacokinetics, and pharmacodynamics of ponesimod, an S1P receptor modulator: favorable impact of dose up-titration. J Clin Pharmacol. 2014;54(2):179–88.
Hoch M, D’Ambrosio D, Wilbraham D, Brossard P, Dingemanse J. Clinical pharmacology of ponesimod, a selective S1P1 receptor modulator, after uptitration to supratherapeutic doses in healthy subjects. Eur J Pharm Sci. 2014;63C:147–53.
Reyes M, Brossard P, Chassard D, Hoch M, Dingemanse J. Effects of ponesimod, a selective S1P1 receptor modulator, on the pharmacokinetics of a hormonal combination contraceptive. Eur J Clin Pharmacol. 2014;70(3):287–93.
Reyes M, Hoch M, Brossard P, Wagner-Redeker W, Miraval T, Dingemanse J. Mass balance, pharmacokinetics and metabolism of the selective S1P receptor modulator ponesimod in humans. Xenobiotica. 2015;45(2):139–49.
Gibaldi M, Perrier D. Pharmacokinetics. New York: Marcel Dekker; 1982.
Poorjavad M, Derakhshandeh F, Etemadifar M, Soleymani B, Minagar A, Maghzi AH. Oropharyngeal dysphagia in multiple sclerosis. Mult Scler. 2010;16(3):362–5.
Schwartz JB. The influence of sex on pharmacokinetics. Clin Pharmacokinet. 2003;42(2):107–21.
Krause A, Brossard P, D’Ambrosio D, Dingemanse J. Population pharmacokinetics and pharmacodynamics of ponesimod, a selective S1P1 receptor modulator. J Pharmacokinet Pharmacodyn. 2014;41(3):261–78.
Schmouder R, Hariry S, David OJ. Placebo-controlled study of the effects of fingolimod on cardiac rate and rhythm and pulmonary function in healthy volunteers. Eur J Clin Pharmacol. 2012;68(4):355–62.
Kappos L, Radue EW, O’Connor P, Polman C, Hohlfeld R, Calabresi P, et al. A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis. N Engl J Med. 2010;362(5):387–401.
Cohen JA, Barkhof F, Comi G, Hartung HP, Khatri BO, Montalban X, et al. Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis. N Engl J Med. 2010;362(5):402–15.
Acknowledgments
The authors wish to express their thanks to Dr. Andrea Vaclavkova for her contribution to this work.
Conflicts of interest
Actelion Pharmaceuticals Ltd provided funding for these clinical trials. At the time of the study conduct and reporting, Pierre-Eric Juif, Matthias Hoch, Daniele D’Ambrosio, and Jasper Dingemanse were full‐time employees of Actelion Pharmaceuticals Ltd. SGS Aster SAS and the Hawaii Clinical Research Center received financial compensation for the clinical conduct of Study 1 and Study 2, respectively. The study investigators were M. Guillaume (at SGS Aster SAS) and J. Ruckle (at Hawaii Clinical Research Center).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Juif, PE., Hoch, M., D’Ambrosio, D. et al. Biocomparison of Three Formulations of the S1P1 Receptor Modulator Ponesimod in Healthy Subjects. Drugs R D 15, 203–210 (2015). https://doi.org/10.1007/s40268-015-0095-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-015-0095-7