Abstract
The effect of fabrics on common atopic dermatitis (AD) is significant, but studies are sparse. Current evidence suggests ubiquitous cotton and silk do not exacerbate AD; like superfine wool, they may improve it. Coarse and/or occlusive fabrics like wool, nylon, acetate and most polyesters are not recommended. Newer manufactured options like lyocell and antimicrobial silver-impregnated textiles are promising. All these fabrics need further study in AD.
Similar content being viewed by others
References
Ricci G, Dondi A, Patrizi A. Useful tools for the management of atopic dermatitis. Am J Clin Dermatol. 2009;10(5):287–300.
Forston EA, Feldman SR, Strowd LC. Managment of atopic dermatitis: methods and challenges. Cham: Springer International Publishing AG; 2017.
Jaros J, Wilson C, Shi VY. Fabric selection in atopic dermatitis: an evidence-based review. Am J Clin Dermatol. 2020;21(4):467–82.
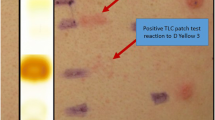
Mobolaji-Lawal M, Nedorost S. The role of textiles in dermatitis: an update. Curr Allergy Asthma Rep. 2015. https://doi.org/10.1007/s11882-015-0518-0.
Dawn A, Papoiu AD, Chan YH, et al. Itch characteristics in atopic dermatitis: results of a web-based questionnaire. Br J Dermatol. 2009;160(3):642–4.
Hendricks AJ, Vaughn AR, Clark AK, et al. Sweat mechanisms and dysfunctions in atopic dermatitis. J Dermatol Sci. 2018;89(2):105–11.
Daeschlein G, Assadian O, Arnold A, et al. Bacterial burden of worn therapeutic silver textiles for neurodermitis patients and evaluation of efficacy of washing. Skin Pharmacol Physiol. 2010;23(2):86–90.
Mason R. Fabrics for atopic dermatitis. J Fam Health Care. 2008;18(2):63–5.
Ricci G, Patrizi A, Mandrioli P, et al. Evaluation of the antibacterial activity of a special silk textile in the treatment of atopic dermatitis. Dermatology. 2006;213(3):224–7.
Yao L, Tokura H, Li Y, et al. Effect of wearing cotton or polyester pajamas on stratum corneum water content under mildly cold conditions. J Am Acad Dermatol. 2006;55(5):910–2.
Stinco G, Piccirillo F, Valent F. A randomized double-blind study to investigate the clinical efficacy of adding a non-migrating antimicrobial to a special silk fabric in the treatment of atopic dermatitis. Dermatology. 2008;217(3):191–5.
Goddard AL, Lio PA. Alternative, complementary, and forgotten remedies for atropic dermatitis. Evid Based Complement Altern Med. 2015;2015:676897.
Gauger A, Mempel M, Schekatz A, et al. Silver-coated textiles reduce Staphylococcus aureus colonization in patients with atopic eczema. Dermatology. 2003;207(1):15–21.
Fowler JF, Fowler LM, Lorenz D. Effects of merino wool on atopic dermatitis using clinical, quality of life, and physiological outcome measures. Dermatitis. 2019;30(3):198–206.
Su JC, Dailey R, Zallmann M, et al. Determining effects of superfine sheep wool in INfantile Eczema (DESSINE): a randomized paediatric crossover study. Br J Dermatol. 2017;177(1):125–33.
Makvandi P, Jamaledin R, Jabbari M, et al. Antibacterial quaternary ammonium compounds in dental materials: a systematic review. Dent Mater. 2018;34(6):851–67.
Fontanini C, Berti I, Monasta L, et al. DermaSilk in long-term control of infantile atopic dermatitis: a double blind randomized controlled trial. G Ital Dermatol Venereol. 2013;148(3):293–7.
Thomas KS, Bradshaw LE, Sach TH, et al. Randomised controlled trial of silk therapeutic garments for the management of atopic eczema in children: the CLOTHES trial. Health Technol Assess. 2017;21(16):1–260.
Love WE, Nedorost ST. Fabric preferences of atopic dermatitis patients. Dermatitis. 2009;20(1):29–33.
Holm L, Öhman S, Bengtsson Å, et al. Effectiveness of occlusive bedding in the treatment of atopic dermatitis: a placebo-controlled trial of 12 months’ duration. Allergy. 2001;56(2):152–8.
Araujo CP, Gomes J, Vieira AP, et al. A proposal for the use of new silver-seaweed-cotton fibers in the treatment of atopic dermatitis. Cutan Ocul Toxicol. 2013;32(4):268–74.
Srour J, Wollenberg A. Evaluation of antimicrobial textiles for atopic dermatitis. J Eur Acad Dermatol Venereol. 2019;33(2):384–90.
Pluut OA, Bianco C, Jakasa I, et al. Percutaneous penetration of silver from a silver containing garment in healthy volunteers and patients with atopic dermatitis. Toxicol Lett. 2015;235(2):116–22.
Hipler UC, Elsner P, Fluhr JW. A new silver-loaded cellulosic fiber with antifungal and antibacterial properties. Curr Probl Dermatol. 2006;33:165–78.
Fluhr JW, Breternitz M, Kowatzki D, et al. Silver-loaded seaweed-based cellulosic fiber improves epidermal skin physiology in atopic dermatitis: safety assessment, mode of action and controlled, randomized single-blinded exploratory in vivo study. Exp Dermatol. 2010;19(8):e9-15.
Gauger A, Fischer S, Mempel M, et al. Efficacy and functionality of silver-coated textiles in patients with atopic eczema. J Eur Acad Dermatol Venereol. 2006;20(5):534–41.
Wiegand C, Hipler UC, Boldt S, et al. Skin-protective effects of a zinc oxide-functionalized textile and its relevance for atopic dermatitis. Clin Cosmet Investig Dermatol. 2013;6:115–21.
Kanehara S, Ohtani T, Uede K, et al. Clinical effects of undershirts coated with borage oil on children with atopic dermatitis: a double-blind, placebo-controlled clinical trial. J Dermatol. 2007;34(12):811–5.
Lopes C, Soares J, Tavaria F, et al. Chitosan coated textiles may improve atopic dermatitis severity by modulating skin staphylococcal profile: a randomized controlled trial. PLoS ONE. 2015;10(11):e0142844.
Jagadish R, Fabien S, Stéphane G, et al. Chitosan-based sustainable textile technology: process, mechanism, innovation, and safety. Rijeka: InTechOpen; 2017.
Jaeger T, Rothmaier M, Zander H, et al. Acid-coated textiles (pH 5.5–6.5)—a new therapeutic strategy for atopic eczema? Acta Derm Venereol. 2015;95(6):659–63.
Kim SH, Hwang SH, Hong SK, et al. The clinical efficacy, safety and functionality of anion textile in the treatment of atopic dermatitis. Ann Dermatol. 2012;24(4):438–43.
Yip J. Advanced textiles for intimate apparel. In: Yu W, editor. Advances in women’s intimate apparel technology. Cambridge: Woodhead Publishing; 2016. p. 3–23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflict of interest
C. Fenton is a contracted employee of Adis International Ltd/Springer Nature and declares no relevant conflicts of interest. Z.T. Al-Salama is a salaried employee of Adis International/ Springer Nature, is an editor of Drugs & Therapy Perspectives, was not involved in any publishing decision for the manuscript, and declares no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent for publication, Availability of data and material, Code availability
Not applicable.
Rights and permissions
About this article
Cite this article
Fenton, C., Al-Salama, Z.T. Fabrics can greatly improve or exacerbate atopic dermatitis. Drugs Ther Perspect 37, 157–161 (2021). https://doi.org/10.1007/s40267-021-00822-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-021-00822-5