Abstract
Background and Objectives
Secondary prevention of peripheral arterial disease includes administration of statins regardless of the patient’s serum cholesterol level. Our study aimed to identify patient-associated risk factors for statin non-persistence and comparison of the explanatory power of models based on clusters of patient-associated characteristics.
Methods
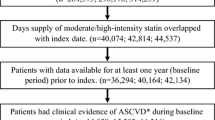
Our study cohort (n = 8330) was assembled from the database of the largest health insurance provider in the Slovak Republic. Statin users aged ≥ 65 years in whom peripheral arterial disease was diagnosed during 2012 were included. Patients were followed for 5 years; those with a treatment gap period of at least 6 months without statin prescription were classified as “non-persistent”. The risk factors for non-persistence were identified within six models (sociodemographic, cardiovascular events, comorbid conditions, statin-related characteristics, cardiovascular co-medication and full model) using Cox regression. The explanatory power of models was assessed using Harrell’s C-index.
Results
At the end of the follow-up, 35.7% of patients were found to be non-persistent. The full model had the highest explanatory power (C = 0.632). Female sex, atorvastatin and rosuvastatin as initially administered statins, being a new statin user and an increasing co-payment were associated with an increased risk for non-persistence. Increasing age, history of ischaemic stroke, diabetes mellitus, general practitioner as index prescriber, increasing overall number of medications and co-administration of certain cardiovascular co-medications were associated with a lower likelihood for non-persistence.
Conclusions
Patients identified as high risk for non-persistence require special attention aimed at the improvement of their persistence with statin treatment.


Similar content being viewed by others
References
Coppola G, Novo S. Statins and peripheral arterial disease: effects on claudication, disease progression, and prevention of cardiovascular events. Arch Med Res. 2007;38(5):479–88.
Kalbaugh CA, Kucharska-Newton A, Wruck L, et al. Peripheral artery disease prevalence and incidence estimated from both outpatient and inpatient settings among Medicare fee-for-service beneficiaries in the Atherosclerosis Risk in Communities (ARIC) Study. J Am Heart Assoc. 2017;6(5):1–9.
Kannel WB, McGee DL. Update on some epidemiologic features of intermittent claudication: the Framingham Study. J Am Geriatr Soc. 1985;33(1):13–8.
Tendera M, Aboyans V, Bartelink ML, et al. ESC guidelines on the diagnosis and treatment of peripheral artery diseases: document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries. The Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2011;32(22):2851–906.
Markel A. Statins and peripheral arterial disease. Int Angiol. 2015;34(5):416–27.
Bonaca MP, Creager MA. Pharmacological treatment and current management of peripheral artery disease. Circ Res. 2015;116(9):1579–98.
Endres M. Statins and stroke. J Cereb Blood Flow Metab. 2005;25(9):1093–110.
Burton JK, Papworth R, Haig C, et al. Statin use is not associated with future long-term care admission: extended follow-up of two randomised controlled trials. Drugs Aging. 2018;35(7):657–63.
Thompson W, Pottegård A, Nielsen JB, Haastrup P, Jarbøl DE. How common is statin use in the oldest old? Drugs Aging. 2018;35(8):679–86.
Westin GG, Armstrong EJ, Bang H, et al. Association between statin medications and mortality, major adverse cardiovascular event, and amputation-free survival in patients with critical limb ischemia. J Am Coll Cardiol. 2014;63(7):682–90.
Yandrapalli S, Gupta S, Andries G, Cooper HA, Aronow WS. Drug therapy of dyslipidemia in the elderly. Drugs Aging. 2019;36(4):321–40.
De Geest S, Zullig LL, Dunbar-Jacob J, et al. ESPACOMP medication adherence reporting guideline (EMERGE). Ann Intern Med. 2018;169(1):30–5.
Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705.
Ofori-Asenso R, Jakhu A, Zomer E, Curtis AJ, Korhonen MJ, Nelson M, et al. Adherence and persistence among statin users aged 65 years and over: a systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci. 2018;73(6):813–9.
Ofori-Asenso R, Jakhu A, Curtis AJ, et al. A systematic review and meta-analysis of the factors associated with nonadherence and discontinuation of statins among people aged ≥ 65 years. J Gerontol A Biol Sci Med Sci. 2018;73(6):798–805.
Booth JN 3rd, Colantonio LD, Chen L, et al. Statin discontinuation, reinitiation, and persistence patterns among Medicare beneficiaries after myocardial infarction: a cohort study. Circ Cardiovasc Qual Outcomes. 2017;10(10):1–9.
Daskalopoulou SS, Delaney JA, Filion KB, Brophy JM, Mayo NE, Suissa S. Discontinuation of statin therapy following an acute myocardial infarction: a population-based study. Eur Heart J. 2008;29(17):2083–91.
Muntner P, Yun H, Sharma P, et al. Ability of low antihypertensive medication adherence to predict statin discontinuation and low statin adherence in patients initiating treatment after a coronary event. Am J Cardiol. 2014;114(6):826–31.
Wawruch M, Zatko D, Wimmer G Jr, et al. Patient-related characteristics associated with non-persistence with statin therapy in elderly patients following an ischemic stroke. Pharmacoepidemiol Drug Saf. 2017;26(2):201–7.
Wawruch M, Zatko D, Wimmer G Jr, et al. Age-related differences in non-persistence with statin treatment in patients after a transient ischaemic attack. Clin Drug Investig. 2017;37(11):1047–54.
Romppainen T, Rikala M, Aarnio E, Korhonen MJ, Saastamoinen LK, Huupponen R. Measurement of statin exposure in the absence of information on prescribed doses. Eur J Clin Pharmacol. 2014;70(10):1275–6.
International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Geneva: WHO; 1992. p. 191.
Stone NJ, Robinson JG, Lichtenstein AH, et al. ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl. 2):S1–45.
Guidelines for ATC classification and DDD assignment 2018. Oslo: WHO Collaborating Centre for Drug Statistics Methodology; 2018. p. 283.
Newman SC. Biostatistical methods in epidemiology. Chichester: Wiley; 2001. p. 382.
Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15(4):361–87.
Uno H, Cai T, Pencina MJ, D’Agostino RB, Wei LJ. On the C-statistics for evaluating overall adequacy of risk prediction procedures with censored survival data. Stat Med. 2011;30(10):1105–17.
Baroletti S, Dell’Orfano H. Medication adherence in cardiovascular disease. Circulation. 2010;121(12):1455–8.
Wei MY, Ito MK, Cohen JD, Brinton EA, Jacobson TA. Predictors of statin adherence, switching, and discontinuation in the USAGE survey: understanding the use of statins in America and gaps in patient education. J Clin Lipidol. 2013;7(5):472–83.
Alfian SD, Worawutputtapong P, Schuiling-Veninga CCM, et al. Pharmacy-based predictors of non-persistence with and non-adherence to statin treatment among patients on oral diabetes medication in the Netherlands. Curr Med Res Opin. 2018;34(6):1013–9.
Goldstein KM, Zullig LL, Bastian LA, Bosworth HB. Statin adherence: does gender matter? Curr Atheroscler Rep. 2016;18(11):63.
Miller P. Women and cardiovascular disease: what can health care providers do to reduce the risks? N C Med J. 2016;77(6):406–9.
National Clinical Guideline Centre (UK). MI: secondary prevention. Secondary prevention in primary and secondary care for patients following a myocardial infarction: partial update of NICE CG48. London: Royal College of Physicians (UK); 2013. Available from: http://www.ncbi.nlm.nih.gov/books/NBK247688/. Accessed 1 Mar 2019.
Arnan MK, Burke GL, Bushnell C. Secondary prevention of stroke in the elderly: focus on drug therapy. Drugs Aging. 2014;31(10):721–30.
Ofori-Asenso R, Ilomaki J, Tacey M, Zomer E, Curtis AJ, Si S, et al. Switching, discontinuation, and reinitiation of statins among older adults. J Am Coll Cardiol. 2018;72(21):2675–7.
O’Shea MP, Teeling M, Bennett K. Regional variation in medication-taking behaviour of new users of oral anti-hyperglycaemic therapy in Ireland. Ir J Med Sci. 2015;184(2):403–10.
Helin-Salmivaara A, Lavikainen P, Ruokoniemi P, Korhonen M, Huupponen R. Persistence with statin therapy in diabetic and non-diabetic persons: a nation-wide register study in 1995–2005 in Finland. Diabetes Res Clin Pract. 2009;84(1):e9–11.
Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288(4):455–61.
Ofori-Asenso R, Ilomaki J, Tacey M, Curtis AJ, Zomer E, Bell JS, Zoungas S, Liew D. Prevalence and incidence of statin use and 3-year adherence and discontinuation rates among older adults with dementia. Am J Alzheimers Dis Other Demen. 2018;33(8):527–34.
Ofori-Asenso R, Ilomäki J, Tacey M, et al. Predictors of first-year nonadherence and discontinuation of statins among older adults: a retrospective cohort study. Br J Clin Pharmacol. 2019;85(1):227–35.
Ponikowski P, Voors AA, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18(8):891–975.
Ofori-Asenso R, Ilomäki J, Tacey M, et al. Patterns of statin use and long-term adherence and persistence among older adults with diabetes. J Diabetes. 2018;10(9):699–707.
Citarella A, Kieler H, Sundström A, et al. Family history of cardiovascular disease and influence on statin therapy persistence. Eur J Clin Pharmacol. 2014;70(6):701–7.
Watanabe JH, Kazerooni R, Bounthavong M. Association of copayment with likelihood and level of adherence in new users of statins: a retrospective cohort study. J Manag Care Pharm. 2014;20(1):43–50.
Aarnio EJ, Martikainen JA, Helin-Salmivaara A, et al. Register-based predictors of adherence among new statin users in Finland. J Clin Lipidol. 2014;8(1):117–25.
Morotti K, Lopez J, Vaupel V, Swislocki A, Siegel D. Adherence to and persistence with statin therapy in a veteran population. Ann Pharmacother. 2019;53(1):43–9.
Grant RW, O’Leary KM, Weilburg JB, Singer DE, Meigs JB. Impact of concurrent medication use on statin adherence and refill persistence. Arch Intern Med. 2004;164(21):2343–8.
Ofori-Asenso R, Zoungas S, Liew D. Reinitiation of statin therapy after discontinuation: a meta-analysis. Mayo Clin Proc. 2018;93(5):666–8.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study was supported by a grant from the Scientific Grant Agency of the Ministry of Education, Science, Research and Sport of the Slovak Republic VEGA 1/0112/17. Emma Aarnio has received funding from the Finnish Cultural Foundation. The providers of these grants played no role in the study design, methodology, data collection, analysis and interpretation of the data, preparation of the paper, or in the decision to submit the manuscript.
Conflict of interest
Martin Wawruch, Gejza Wimmer Jr, Jan Murin, Martina Paduchova, Tomas Tesar, Lubica Hlinkova, Peter Slavkovsky, Lubomira Fabryova and Emma Aarnio have no conflicts of interest that are directly relevant to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wawruch, M., Wimmer, G., Murin, J. et al. Patient-Associated Characteristics Influencing the Risk for Non-Persistence with Statins in Older Patients with Peripheral Arterial Disease. Drugs Aging 36, 863–873 (2019). https://doi.org/10.1007/s40266-019-00689-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00689-2