Abstract
Background
A decade ago, statin persistence was < 50% after 1 year, and recent short-term analyses have revealed very little progress in improving statin persistence, even in patients with a prior cardiovascular (CV) event. Data on longer-term statin persistence are lacking. We measured long-term statin persistence in patients with high CV risk.
Methods
This retrospective administrative claims analysis of the Optum Research Database included patients aged ≥ 45 years with diabetes and/or atherosclerotic CV disease (ASCVD) who had a statin prescription filled in 2010. It included an elevated triglycerides (TG) cohort of patients with index date in 2010 and TG ≥ 150 mg/dL (n = 23,181) and a propensity-matched comparator cohort with TG < 150 mg/dL and high-density lipoprotein cholesterol > 40 mg/dL (n = 23,181). Both cohorts were followed for ≥ 6 months up to March 2016.
Results
The probability of remaining on a prescription fill for index statin therapy was 47% after 1 year and 19% after 5 years in both cohorts. Statin persistence was worse among women than men, and among younger versus older patients (P < 0.001 for all comparisons). After 5 years, the probability of remaining on a prescription fill for index statin was < 25% across all subgroups assessed including patients with and without baseline revascularization, heart failure, peripheral artery disease and renal disease. Similar results were observed in a subcohort analysis of patients with TG 200–499 mg/dL.
Conclusions
Long-term statin persistence after 5 years is alarmingly low (< 25%) and is a public health concern.
Similar content being viewed by others
Introduction
Statin therapy forms the cornerstone of both primary and secondary prevention and treatment of atherosclerotic cardiovascular disease (ASCVD) [1]. However, adherence and persistence to statin therapy are low, and this has been shown to negatively impact clinical outcomes and residual cardiovascular (CV) risk [2, 3]. Nearly a decade ago, statin persistence was reported to be less than 50% after 1 year [4]. A more recent study found that the proportion of days covered with a statin after a median follow-up of 2.2 years was 76%, with 40.5% of patients having poor adherence after 2 years [5]. Furthermore, adherence and persistence have been found to be low even in patients at high risk of CV events. In a recent study in which Medicare patients and patients with commercial and Medicare supplemental insurance were followed retrospectively for statin persistence, only 63.8% who started a statin following a myocardial infarction and < 40% of those with diabetes mellitus and a history of coronary heart disease and those without a history of coronary heart disease or diabetes mellitus took the medication with a high degree of adherence [6]. Another recent study in a Veterans Affairs population found an overall high adherence rate among patients taking a stable statin dose for secondary prevention of ASCVD of 87.7%; importantly, this study demonstrated a relationship between adherence and all-cause mortality [7].
Interpretation of results from these studies, however, has been complicated by the wide variability in estimates of statin persistence, as demonstrated in a recent systematic review [8]. This review found that statin persistence in primary prevention in the general population ranged from 7 to 84%, while persistence in secondary prevention for patients with a history of CV events ranged from 11.6 to 76.1%. Data on persistence with long-term statin use are lacking. Indeed, all but two of the studies in the systematic review were less than 3 years in duration; the longest study had a median follow-up of 4.1 years. Persistence in one of these studies was as low as 36.8% in secondary prevention and 23.3% in primary prevention [9]. Statin use among patients with diabetes is also low. In a recent study in patients with diabetes prescribed a statin, the mean proportion of days covered decreased from 0.69 at 6 months to 0.56 at 9 years, with the proportion considered adherent (proportion of days covered ≥ 0.80) decreasing from 54% at 6 months to 30.7% at 9 years [10].
Patients with elevated and high triglycerides (TG) and elevated low-density lipoprotein cholesterol (LDL-C) are at increased risk of CV events, and some residual CV risk remains even in those controlled on a statin [11, 12]. Statin adherence and persistence is therefore of particular interest in this high-risk group. The purpose of this study was to analyze long-term, real-world data on statin persistence in patients with elevated (≥ 150 mg/dL) and high (200–499 mg/dL) TG and high risk of CV disease, including those with diabetes and/or a history of ASCVD.
Methods
Study design
This was an observational retrospective administrative analysis of the Optum Research Database as previously described [13, 14]. The Optum Research Database is a claims database of > 160 million individuals with electronic health records for > 80 million individuals. The follow-up period, which was > 6 months, began on the index date and ended on the earliest of any of the following: the date of disenrollment from the plan, the date of death, or the end of the study on March 31, 2016. No patient identities or medical records were disclosed for the purposes of this study, and it was fully compliant with the Health Insurance Portability and Accountability Act. Measurement of index statin persistence was a secondary objective of the study.
The primary endpoint (frequency of major CV events in the follow-up period), and secondary endpoints (direct health care costs and resource utilization in the follow-up period) have been reported elsewhere [13, 14]. Other secondary prespecified analyses included statin persistence, as reported here.
Study populations
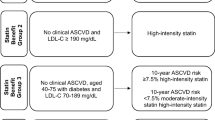
Key inclusion criteria included: men and women aged ≥ 45 years on the index date; at least one prescription claim for statin therapy between January 1, 2010 and December 31, 2010, and ≥ 6 months of baseline data prior to the index date (date of first statin claim); ≥ 1 medical claim with diagnosis code representing diabetes and/or ASCVD (ASCVD included acute coronary syndrome, myocardial infarction, angina, coronary or other arterial revascularization, stroke, transient ischemic attack, or peripheral artery disease [PAD]); and continuous enrollment with medical and pharmacy benefits during the baseline period and ≥ 6 months starting on the index date, or death within 6 months of the index date. Key exclusion criteria included: niacin on the index date from a recent prescription fill, and ICD-9 codes indicating the presence of pregnancy, severe liver disease, acute or chronic pancreatitis, malabsorption syndrome, bypass surgery, HIV/AIDs, end-stage renal disease, hemodialysis, peritoneal dialysis, myositis, polymyositis, rhabdomyolysis, or drug or alcohol abuse.
Patients in an elevated-TG analysis cohort were required to have TG ≥ 150 mg/dL, while those in the comparator cohort were required to have TG < 150 mg/dL and high-density lipoprotein cholesterol (HDL-C) > 40 mg/dL [14]. In addition, a high-TG analysis subcohort (and corresponding comparator cohort) was investigated in patients with TG 200–499 mg/dL [13]. Concomitant use of ezetimibe, fibrates, and prescription omega-3 products was permitted. Data on fish oil dietary supplements were not captured in the claims database as they are not prescription products that generate claims.
Statistical analysis
Persistence with index statin therapy as a class was measured as months to therapy discontinuation, inclusive of prescription fills on the index date. Patients who switched to a different type of statin were captured as persisting on statin therapy by this variable definition and were not captured as discontinuing. Persistence calculations were corrected for inpatient events under the assumption that medication would be supplied by the facility during the stay. Statin therapy was characterized as low, moderate, or high intensity. Ezetimibe was summarized together with statins, either as a low-intensity monotherapy or in combination with atorvastatin or simvastatin. Discontinuation from the index statin was defined as a gap in therapy of 30 days from the run-out date of days’ supply. Discontinuation was calculated within the first 6 months of the follow-up period, as well as for the duration of the follow-up period.
Persistence was calculated using descriptive statistics and with Kaplan-Meier probabilities. Persistence in different risk groups within the elevated- and high-TG and comparator cohorts was also calculated. These risk groups included gender, age, diabetes at baseline, ASCVD at baseline, and other CV diagnoses at baseline, including heart failure, PAD, renal disease, and a history of revascularization. Between-group comparisons were calculated as clustered P values using Cox proportional hazard models with cohort as an independent variable. A P value < 0.05 was considered statistically significant.
A propensity score analysis was used to create a matched comparator study cohort similar to the analysis cohort, but without elevated or high TG, by controlling for confounding relationships. A propensity score is a method of balancing cohorts and assumes that the distribution of observed baseline covariates is similar between the elevated-TG cohort and the comparator cohort. The estimated propensity score is the predicted probability of treatment derived from a fitted logistic regression model in which the cohort indicator is regressed on predetermined baseline characteristics. The method results in matched sets of patients from the two cohorts.
Propensity score matching was performed using a greedy match algorithm [15]. The procedure used attempts to match each case to a single control based on the first 8 digits of the propensity score, which was estimated using logistic regression, then 7 digits, etc., until a match was found. The closest available match, known as the nearest neighbor, was used. Ties were resolved randomly. A maximum allowed propensity score difference (ie, a caliper) of 0.01 between the matched case-control pairs was imposed a priori. Once a match was found, it was not reconsidered and the control was removed from the available pool for matches. The final sample of cases that were successfully matched to the controls was retained for analysis. The final list of variables included in the propensity score model was determined following review of the pre-matching descriptive analyses of patient characteristics and other pre-index measures and included age; gender; insurance type; region; baseline medical cost; LDL-C level relative to the median, if available; baseline use of statins, fibrates, or omega-3 fatty acids; and the following diagnoses: ASCVD, diabetes, stroke, hypertension, renal disease, and peripheral artery disease. Patients in the elevated-TG cohort were matched in a 1:1 ratio to the comparator cohort. Those who were not matched were not included in the descriptive analyses.
Results
Patients
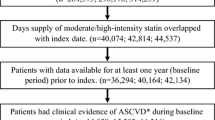
Approximately 1.6 million patients with ≥ 1 prescription claim for a statin were identified from the Optum Research Database. A total of 23,181 propensity score–matched patients were included in the elevated-TG cohort (TG ≥ 150 mg/dL) with 23,181 corresponding patients in the comparator cohort (TG < 150 mg/dL and HDL-C > 40 mg/dL). As previously described, there were few clinically important differences between the elevated-TG and comparator cohorts, except for statistically significant differences in baseline lipids per the inclusion criteria due to the propensity score design (Table 1) [14]. The mean (SD) age was 62.2 (9.6) years and 62.6 (9.9) years in the elevated-TG and comparator cohorts, respectively; approximately 50% were women in both cohorts. Mean duration of follow-up was 41.4 and 42.5 months in the elevated-TG and comparator cohorts, respectively.
Most baseline comorbidities were similar in the elevated-TG and comparator cohorts [14]. Consistent with the study entry criteria requiring a diagnosis of diabetes or ASCVD, 84% of patients in both cohorts had diabetes and 30 and 29% had ASCVD in the elevated-TG cohort and comparator cohort, respectively; in addition, 79% had hypertension in both cohorts. With the exception of PAD (14–15%) and renal disease (12%), all other comorbid diagnoses (myocardial infarction, stroke, angina, coronary revascularization, heart failure, atrial fibrillation, and transient ischemic attack) were present in < 10% of patients in both cohorts.
In addition to statins, during the first 6 months, 7% of patients in both the elevated-TG cohort and comparator cohort were prescribed fibrates, 8% were prescribed ezetimibe, and 2% received prescriptions for omega-3 fatty acids.
A parallel analysis in a subcohort of patients with high TG (200–499 mg/dL; n = 10,990) and a propensity-matched comparator group (TG < 150 mg/dL and HDL-C > 40 mg/dL; n = 10,990) was also conducted with similar demographic and baseline characteristic results [13].
Statin persistence
The proportion of days covered (ie, the proportion of days on which patients had index statin available) is shown in Table 2. For those patients who discontinued index statin therapy, the mean (SD) time to discontinuation was approximately 10.4 months and 10.3 months in the elevated-TG and comparator cohorts, respectively (Table 2). Among patients who discontinued index statin therapy, 55.6% in the elevated-TG cohort and 56.7% in the comparator cohort did so within the first 6 months (P = 0.036 for comparison). Kaplan-Meier estimates of the time to discontinuation are shown in Fig. 1. After 1 year, the probability of remaining on a prescription fill for index statin was 47% in both the elevated-TG cohort and its comparator cohort. At 5 years, the probability of these patients remaining on a prescription fill for index statin therapy fell to 19%, with no significant difference between the two cohorts (clustered P value for elevated-TG cohort vs comparator cohort, 0.511).
In the parallel analysis of the subcohort of patients with high TG (TG > 200–499 mg/dL) versus a propensity-matched comparator group (TG < 150 mg/dL and HDL-C > 40 mg/dL), similar results were observed overall and in all subgroups tested below. These results are summarized in Tables 3, 4, 5, 6, 7, 8, 9, 10 and 11.
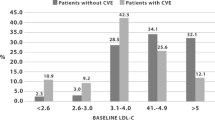
Subgroup analyses of statin persistence
Across all subgroups, using Kaplan-Meier analysis, the probability of remaining on a prescription fill for index statin was < 54% at 1 year and < 25% at 5 years. Statin persistence was worse in women than in men (P < 0.001; Fig. 2 and Table 4). In the elevated-TG cohort, the probability of remaining on a prescription fill for index statin therapy after 5 years was 21.3% for men and 16.3% for women, compared with 21.7 and 16.9% in the comparator cohort, respectively. Statin persistence was worse in younger than in older patients (P < 0.001; Table 5). In the elevated-TG and comparator cohorts, respectively, the probability of remaining on a prescription fill for index statin therapy after 5 years was 14 and 13% for patients aged 45–54 years, 18 and 20% for patients aged 55–64 years, and 23% in both cohorts for patients aged ≥ 65 years.
Persistence to Index Statin Therapy by Patients With High CV Risk According to TG Level, Gender, and Age. Kaplan-Meier analysis. Clustered P values were calculated using cohort and gender. See Tables 4 and 5 for P values. P < 0.001 for comparisons between men vs women and younger vs older patients. *TG ≥150 mg/dL. †TG < 150 mg/dL and HDL-C > 40 mg/dL; propensity score matched to elevated-TG cohort. CV, cardiovascular; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides
By contrast, in patients with baseline ASCVD, the probability of remaining on a prescription fill for index statin therapy after 5 years was slightly higher than in those without baseline ASCVD, although persistence was still poor (P = 0.001 and P = 0.002 for the elevated-TG cohort and the comparator cohort, respectively: Fig. 3; Table 6). In the elevated-TG cohort, the probability of remaining on a prescription fill for index statin therapy after 5 years was 20.3% for patients with baseline ASCVD, compared with 18.2% for those without baseline ASCVD; these probabilities were 20.2 and 19.0% for those with and without baseline ASCVD in the comparator cohort, respectively (Table 6).
Persistence With Index Statin in High CV Risk Patients by TG Level and Baseline ASCVD. Clustered P values were calculated using cohort and baseline ASCVD. See Table 6 for P values. P < 0.01 for comparisons between patients with and without baseline ASCVD. *TG ≥150 mg/dL. †TG < 150 mg/dL and HDL-C > 40 mg/dL; propensity score matched to elevated-TG cohort. ASCVD, atherosclerotic cardiovascular disease; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides
Patients without diabetes at baseline had a higher probability of remaining on a prescription fill for index statin over the course of the study than those with diabetes (P = 0.029 and P = 0.002 for the elevated-TG cohort and comparator cohort, respectively) but again, persistence was low (Table 7). In the elevated-TG cohort, the probability of remaining on a prescription fill for index statin therapy after 5 years was 20.8% for patients without baseline diabetes and 18.4% for those with baseline diabetes; similarly, the probability of remaining on a prescription fill for index statin therapy was 19.0 and 21.0% for those with and without baseline diabetes, respectively, in the comparator cohort (Table 5). There were no significant differences in persistence among patients with or without diabetes between the elevated-TG and comparator cohorts.
Similar trends of poor persistence were seen in other subgroups, with patients with a history of peripheral arterial revascularization, heart failure, PAD, and renal disease at baseline all having greater probability of persistence (although still poor) than those with no history (comparisons did not reach statistical significance; Tables 8, 9, 10 and 11). There was also no difference in statin persistence between those with elevated TG and propensity-matched comparators in these subgroups.
Discussion
Results from this 5-year retrospective administrative claims analysis indicate that persistence with index statin therapy is poor in patients with elevated TG (≥ 150 mg/dL) or high TG (200–499 mg/dL), diabetes, and/or ASCVD. This result is consistent with a number of previous studies over the past two decades, and confirms that poor long-term statin persistence remains an issue of concern for patients with high CV disease risk, including those with elevated TG who may be at increased risk of CV events and patients with diabetes [4,5,6, 8, 10, 16, 17]. This highlights the fact that very little, if anything, has changed in the last two decades with regard to improving statin persistence, which remains abysmal in all groups probed in our study, all of whom are at high risk of CV events. This low persistence has a significant effect on risk for CV events, including death. A systematic review found that statin discontinuation was associated with an increased risk of death or CV events [17]. In a Danish population study of nearly 675,000 individuals, early statin discontinuation increased with negative reports about statins in the news media and was associated with increased risk of myocardial infarction and death from CV disease, whereas early statin discontinuation decreased with positive news media reports about statin [18]. In a population study from the United Kingdom, statin discontinuation after acute myocardial infarction was associated with higher total mortality than any other pattern of statin prescription [19]. A recent analysis in a Veterans Affairs population found that poor statin adherence, particularly high-intensity statins, was associated with a higher incidence of all-cause mortality [7]. Another study estimated that improving adherence from 50 to 75% could double the number of deaths prevented [20].
Given the consistently low adherence to statin therapy in all of these studies, it is important to consider what steps could be taken to remedy this issue. A number of modifiable factors associated with patient out-of-pocket costs, including use of generic versus brand-name statins, low or no copayments, and coupons, have been identified [21]. Statin intolerance due to adverse effects may be another important reason for discontinuing therapy [22]; in an internet survey of statin users, the primary reason for stopping statin therapy was side effects (primarily muscle-related side effects) in 62% [23]. Poor statin adherence due to intolerance has been associated with an increased risk of recurrent myocardial infarction and coronary heart disease events [24]. Providing support for and careful assessment of patients who report side effects that are potentially related to statins may help improve adherence and persistence [25]. Physicians should address any side-effect–related concerns that patients have, and, if necessary, titrate the dose or switch to another statin [26]. Alternate-day dosing of statins is another option for patients with statin intolerance [27]. Cholesterol management guidelines recommend proactively screening for muscle issues prior to initiating and during statin therapy, including measuring creatine kinase levels in those at greatest risk, in order to proactively manage this side effect and distinguish from unrelated muscle issues to ensure continued persistence [1].
Another possible reason for the low persistence in the population described here is the burden of polypharmacy [28]. Approximately 85% of patients in this study had diabetes, 79% had hypertension, and 29% had a history of ASCVD, in addition to other comorbidities. Most patients were therefore likely taking several medications multiple times a day, leading to reduced persistence [28, 29]. One retrospective study in a Veterans Health Administration population suggested that statin adherence actually correlated with the number of drugs that patients were taking at baseline [30]. Other factors that may affect adherence and persistence include illness; beliefs about the intervention in question and its perceived risks, benefits, and necessity; patient–practitioner relationship; physical and mental illness; and financial constraints [29, 31]. The high rate of diabetes, hypertension, and other comorbidities in this population, and the resulting polypharmacy, suggest that these persistence data are not generalizable to patients with simple hypertriglyceridemia.
Statin nonadherence and nonpersistence have been associated with younger patient age, female gender, lower income, and nonwhite race [31,32,33]. This is in agreement with the results of this study, which found that female gender and younger age were associated with significantly lower statin persistence over 5 years of follow-up. Of note, while previous studies have suggested that concomitant diabetes is predictive of better adherence and persistence, our study found slightly lower persistence in patients with diabetes [32]. This may reflect the study design, which required that all patients have diabetes or ASCVD. As a result, all patients without diabetes had ASCVD, which may be associated with a higher rate of statin persistence than diabetes. Persistence with medications for asymptomatic diseases, such as hypercholesterolemia, is also a challenge because of the lack of noticeable efficacy by the patient in everyday life; this may explain in part the low persistence with statin therapy observed here [31]. Regardless of the reasons patients are not continuing their index statin, this study emphasizes that statin persistence is alarmingly poor and is likely contributing to adverse health outcomes in these high-risk patients.
This study has a number of limitations. Data used in the study were collected for administration of health claims, not for research. The included population was limited to patients in a managed care health plan in the United States and may not be generalizable to other populations. In addition, medication usage claims do not indicate whether the medication was consumed or whether it was taken as prescribed. The data may also contain inaccurate recording of health events, missing data, and uncertainty about internal validity [34, 35]. Laboratory test results, including lipid measures during the follow-up period, were only available for a subset of patients, but the extent of missing data may not be distinguishable from the lack of an administered test. The analysis measured only persistence with statin index therapy as a class and did not measure whether patients who discontinued index statin resumed therapy with another lipid-lowering medication class. This analysis was designed to assess health status and burden over time in patients with elevated TG despite having generally controlled LDL-C, and was not designed to assess the potential effects of any treatment modality. Statistical analyses should be evaluated in the context of the large sample size; this may indicate statistical significance for some parameters even when differences are small and not clinically meaningful. This is potentially enhanced by the large number of statistical comparisons conducted across various subgroups which may have introduced type 1 errors. Despite these limitations, real-world data are pragmatic in that they examine patient populations in the context of clinical practice and may be more reflective of actual use in practice than evidence from clinical trials [34, 36].
Conclusions
This study highlights that persistence with statin therapy is very poor. Although most patients at increased CV risk—including those with ASCVD, elevated or high TG, heart failure, PAD, renal disease, and a history of revascularization—had slightly better probability of persistence than those who did not, persistence remained low after 5 years. These findings underscore the need to develop public health programs and nationwide patient education initiatives about the well-defined benefits of statin therapy, particularly in the high-risk setting. The crucial need to ensure long-term statin persistence in high-risk patients should also be reinforced at all patient follow-up visits. Helping patients understand that statin discontinuation correlates with increased risk for acute CV events and death is a matter that cannot be overemphasized. Institution of programs to enhance persistence and adherence to statin therapy, especially in women and younger patients, is also required.
Availability of data and materials
Data are proprietary to Optum and cannot be shared.
Abbreviations
- ASCVD:
-
Atherosclerotic cardiovascular disease
- CV:
-
Cardiovascular
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- PAD:
-
Peripheral artery disease
- TG:
-
Triglycerides
References
Stone NJ, Robinson J, Lichtenstein AH, Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;129(25(suppl 2)):S1-S45.
Toth PP, Banach M. Statins: then and now. Methodist Debakey Cardiovasc J. 2019;15(1):23–31.
Banach M, Stulc T, Dent R, Toth PP. Statin non-adherence and residual cardiovascular risk: there is need for substantial improvement. Int J Cardiol. 2016;225:184–96.
Dorais M, Chirovsky D, Ambegaonkar B, Sazonov V, Davies G, Grant S, et al. Utilization patterns of extended-release niacin in Canada: analysis of an administrative claims database. Can J Cardiol. 2010;26(7):e229–35.
Virani SS, Akeroyd JM, Nambi V, Heidenreich PA, Morris PB, Nasir K, et al. Estimation of eligibility for PCSK9 inhibitors and associated costs based on the FOURIER trial: insights from the Department of Veterans Affairs. Circulation. 2017;135(25):2572–4.
Colantonio LD, Rosenson RS, Deng L, Monda KL, Dai Y, Farkouh ME, et al. Adherence to statin therapy among US adults between 2007 and 2014. J Am Heart Assoc. 2019;8(1):e010376.
Rodriguez F, Maron DJ, Knowles JW, Virani SS, Lin S, Heidenreich PA. Association of statin adherence with mortality in patients with atherosclerotic cardiovascular disease. JAMA Cardiol. 2019;4(3):206.
Deshpande S, Quek RG, Forbes CA, de Kock S, Kleijnen J, Gandra SR, et al. A systematic review to assess adherence and persistence with statins. Curr Med Res Opin. 2017;33(4):769–78.
Chodick G, Shalev V, Gerber Y, Heymann AD, Silber H, Simah V, et al. Long-term persistence with statin treatment in a not-for-profit health maintenance organization: a population-based retrospective cohort study in Israel. Clin Ther. 2008;30(11):2167–79.
Ofori-Asenso R, Ilomaki J, Tacey M, Zomer E, Curtis AJ, Bell JS, et al. Patterns of statin use and long-term adherence and persistence among older adults with diabetes. J Diabetes. 2018;6(4):E134.
Kasai T, Miyauchi K, Yanagisawa N, Kajimoto K, Kubota N, Ogita M, et al. Mortality risk of triglyceride levels in patients with coronary artery disease. Heart. 2013;99(1):22–9.
Sarwar N, Danesh J, Eiriksdottir G, Sigurdsson G, Wareham N, Bingham S, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2007;115(4):450–8.
Toth PP, Granowitz C, Hull M, Liassou D, Anderson A, Philip S. High triglycerides are associated with increased cardiovascular events, medical costs, and resource utilization: a real-world administrative claims analysis of statin-treated patients with high residual cardiovascular risk. J Am Heart Assoc. 2018;7(15):e008740.
Toth PP, Philip S, Hull M, Granowitz C. Elevated triglycerides are associated with increased cardiovascular risk and direct costs in statin-treated patients. Mayo Clin Proc. 2019; in press.
Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques [poster 214-26]. Proceedings of the 26th Annual SAS Users Group International Conference; 2001; Long Beach, CA.
Colantonio LD, Huang L, Monda KL, Bittner V, Serban MC, Taylor B, et al. Adherence to high-intensity statins following a myocardial infarction hospitalization among Medicare beneficiaries. JAMA Cardiol. 2017;2(8):890–5.
De Vera MA, Bhole V, Burns LC, Lacaille D. Impact of statin adherence on cardiovascular disease and mortality outcomes: a systematic review. Br J Clin Pharmacol. 2014;78(4):684–98.
Nielsen SF, Nordestgaard BG. Negative statin-related news stories decrease statin persistence and increase myocardial infarction and cardiovascular mortality: a nationwide prospective cohort study. Eur Heart J. 2016;37(11):908–16.
Daskalopoulou SS, Delaney JA, Filion KB, Brophy JM, Mayo NE, Suissa S. Discontinuation of statin therapy following an acute myocardial infarction: a population-based study. Eur Heart J. 2008;29(17):2083–91.
Shroufi A, Powles JW. Adherence and chemoprevention in major cardiovascular disease: a simulation study of the benefits of additional use of statins. J Epidemiol Community Health. 2010;64(2):109–13.
Birtcher K. When compliance is an issue-how to enhance statin adherence and address adverse effects. Curr Atheroscler Rep. 2015;17(1):471.
Banach M, Rizzo M, Toth PP, Farnier M, Davidson MH, Al-Rasadi K, et al. Statin intolerance - an attempt at a unified definition. Position paper from an international lipid expert panel. Arch Med Sci 2015;11(1):1–23.
Cohen JD, Brinton EA, Ito MK, Jacobson TA. Understanding statin use in America and gaps in patient education (USAGE): an internet-based survey of 10,138 current and former statin users. J Clin Lipidol. 2012;6(3):208–15.
Serban MC, Colantonio LD, Manthripragada AD, Monda KL, Bittner VA, Banach M, et al. Statin intolerance and risk of coronary heart events and all-cause mortality following myocardial infarction. J Am Coll Cardiol. 2017;69(11):1386–95.
Toth PP, Patti AM, Giglio RV, Nikolic D, Castellino G, Rizzo M, et al. Management of statin intolerance in 2018: still more questions than answers. Am J Cardiovasc Drugs. 2018;18(3):157–73.
Rosenson RS, Baker S, Banach M, Borow KM, Braun LT, Bruckert E, et al. Optimizing cholesterol treatment in patients with muscle complaints. J Am Coll Cardiol. 2017;70(10):1290–301.
Awad K, Mikhailidis DP, Toth PP, Jones SR, Moriarty P, Lip GYH, et al. Efficacy and safety of altern8 ate-day versus daily dosing of statins: a systematic review and meta-analysis. Cardiovasc Drugs Ther. 2017;31(4):419–31.
Tiktin M, Celik S, Berard L. Understanding adherence to medications in type 2 diabetes care and clinical trials to overcome barriers: a narrative review. Curr Med Res Opin. 2016;32(2):277–87.
Mukhtar O, Weinman J, Jackson SH. Intentional non-adherence to medications by older adults. Drugs Aging. 2014;31(3):149–57.
Watanabe JH, Bounthavong M, Chen T, Ney JP. Association of polypharmacy and statin new-user adherence in a Veterans Health Administration population: a retrospective cohort study. Ann Pharmacother. 2013;47(10):1253–9.
Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119(23):3028–35.
Mann DM, Woodward M, Muntner P, Falzon L, Kronish I. Predictors of nonadherence to statins: a systematic review and meta-analysis. Ann Pharmacother. 2010;44(9):1410–21.
Ma J, Sehgal NL, Ayanian JZ, Stafford RS. National trends in statin use by coronary heart disease risk category. PLoS Med. 2005;2(5):e123.
Sherman RE, Anderson SA, Dal Pan GJ, Gray GW, Gross T, Hunter NL, et al. Real-world evidence - what is it and what can it tell us? N Engl J Med. 2016;375(23):2293–7.
Berger ML, Sox H, Willke RJ, Brixner DL, Eichler HG, Goettsch W, et al. Good practices for real-world data studies of treatment and/or comparative effectiveness: recommendations from the joint ISPOR-ISPE special task force on real-world evidence in health care decision making. Value Health. 2017;20(8):1003–8.
Jarow JP, LaVange L, Woodcock J. Multidimensional evidence generation and FDA regulatory decision making: defining and using “real-world” data. JAMA. 2017;318(8):703–4.
Acknowledgements
Medical writing assistance was provided by Peloton Advantage, LLC, an OPEN Health company, Parsippany, NJ, and funded by Amarin Pharma Inc, Bedminster, NJ.
Funding
This study was funded by Amarin Pharma Inc, Bedminster, NJ.
Author information
Authors and Affiliations
Contributions
Study design: PPT, CG, MH, SP. Data analysis/interpretation: All authors. Critical revision and review of the manuscript: All authors. Project/data management: All authors. Statistical analyses: SP, CG, MH. Approval of final draft for submission: All authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
PPT is a consultant and/or speaker for Amarin Pharma Inc, Amgen, Kowa, Novo-Nordisk, Regeneron, and Sanofi. SP and CG are employees and stock shareholders of Amarin Pharma Inc. MH and AA are employees of Optum.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Toth, P.P., Granowitz, C., Hull, M. et al. Long-term statin persistence is poor among high-risk patients with dyslipidemia: a real-world administrative claims analysis. Lipids Health Dis 18, 175 (2019). https://doi.org/10.1186/s12944-019-1099-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-019-1099-z