Abstract
Background
Chronic kidney disease (CKD) afflicts many older adults and increases the risk for medication-related adverse events.
Objective
The aim of this study was to assess the prevalence and associated morbidity and mortality of polypharmacy (use of several medications concurrently), and potentially inappropriate medication (PIM) use in older adults, looking for differences by CKD status.
Methods
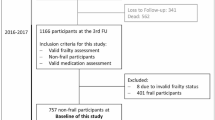
We quantified medication and PIM use (from Beers criteria, the Screening Tool of Older People’s Prescriptions, and Micromedex®) by level of estimated glomerular filtration rate (eGFR) for participants aged 65 years or older attending a baseline study visit in the Atherosclerosis Risk in Communities study (n =6392). We used zero-inflated negative binomial and Cox proportional hazards regressions to assess the relationship between baseline polypharmacy, PIM use, and subsequent hospitalization and death.
Results
Mean age at baseline was 76 (± 5) years, 59% were female, and 29% had CKD (eGFR < 60 ml/min/1.73 m2). Overall, participants reported 6.1 (± 3.5) medications and 2.3 (± 2.2) vitamins/supplements; 16% reported ≥ 10 medications; 31% reported a PIM based on their age. On average, participants with CKD reported more medications. A PIM based on kidney function was used by 36% of those with eGFR < 30 ml/min/1.73 m2. Over a median of 2.6 years, more concurrent medications were associated with higher risk of hospitalization and death, but PIM use was not. While those with CKD had higher absolute risks, there was no difference in the relative risks associated with greater numbers of medications by CKD status.
Conclusion
Polypharmacy and PIM use were common, with greater numbers of medications associated with higher risk of hospitalization and death; relative risks were similar for those with and without CKD.



Similar content being viewed by others
References
He W, Goodkind D, Kowal P. An aging world: 2015, international population reports. Washington, DC: U.S. Government Publishing Office; 2016.
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298(17):2038–47.
Lassiter J, Bennett WM, Olyaei AJ. Drug dosing in elderly patients with chronic kidney disease. Clin Geriatr Med. 2013;29(3):657–705.
Masoudi FA, Baillie CA, Wang Y, Bradford WD, Steiner JF, Havranek EP, et al. The complexity and cost of drug regimens of older patients hospitalized with heart failure in the United States, 1998–2001. Arch Intern Med. 2005;165(18):2069–76.
Bushardt RL, Massey EB, Simpson TW, Ariail JC, Simpson KN. Polypharmacy: misleading, but manageable. Clin Interv Aging. 2008;3(2):383–9.
Slabaugh SL, Maio V, Templin M, Abouzaid S. Prevalence and risk of polypharmacy among the elderly in an outpatient setting: a retrospective cohort study in the Emilia-Romagna region, Italy. Drugs Aging. 2010;27(12):1019–28.
Banerjee A, Mbamalu D, Ebrahimi S, Khan AA, Chan TF. The prevalence of polypharmacy in elderly attenders to an emergency department—a problem with a need for an effective solution. Int J Emerg Med. 2011;4(1):22.
Rohrer JE, Garrison G, Oberhelman SA, Meunier MR. Epidemiology of polypharmacy among family medicine patients at hospital discharge. J Prim Care Commun Health. 2013;4(2):101–5.
Qato DM, Alexander GC, Conti RM, Johnson M, Schumm P, Lindau ST. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA. 2008;300(24):2867–78.
Sharma M, Loh KP, Nightingale G, Mohile SG, Holmes HM. Polypharmacy and potentially inappropriate medication use in geriatric oncology. J Geriatr Oncol. 2016;7(5):346–53.
Wooten JM. Pharmacotherapy considerations in elderly adults. South Med J. 2012;105(8):437–45.
Papaioannou A, Clarke JA, Campbell G, Bedard M. Assessment of adherence to renal dosing guidelines in long-term care facilities. J Am Geriatr Soc. 2000;48(11):1470–3.
Chang F, O’Hare AM, Miao Y, Steinman MA. Use of renally inappropriate medications in older veterans: a national study. J Am Geriatr Soc. 2015;63(11):2290–7.
Goldberg RM, Mabee J, Chan L, Wong S. Drug-drug and drug-disease interactions in the ED: analysis of a high-risk population. Am J Emerg Med. 1996;14(5):447–50.
Schottker B, Saum KU, Muhlack DC, Hoppe LK, Holleczek B, Brenner H. Polypharmacy and mortality: new insights from a large cohort of older adults by detection of effect modification by multi-morbidity and comprehensive correction of confounding by indication. Eur J Clin Pharmacol. 2017;73(8):1041–8.
Herr M, Robine JM, Pinot J, Arvieu JJ, Ankri J. Polypharmacy and frailty: prevalence, relationship, and impact on mortality in a French sample of 2350 old people. Pharmacoepidemiol Drug Saf. 2015;24(6):637–46.
Flaherty JH, Perry HM, Lynchard GS, Morley JE. Polypharmacy and hospitalization among older home care patients. J Gerontol A Biol Sci Med Sci. 2000;55(10):554.
Onder G, Pedone C, Landi F, Cesari M, Della Vedova C, Bernabei R, et al. Adverse drug reactions as cause of hospital admissions: results from the Italian Group of Pharmacoepidemiology in the Elderly (GIFA). J Am Geriatr Soc. 2002;50(12):1962–8.
Hellden A, Bergman U, von Euler M, Hentschke M, Odar-Cederlof I, Ohlen G. Adverse drug reactions and impaired renal function in elderly patients admitted to the emergency department: a retrospective study. Drugs Aging. 2009;26(7):595–606.
Leendertse AJ, van Dijk EA, De Smet PA, Egberts TC, van den Bemt PM. Contribution of renal impairment to potentially preventable medication-related hospital admissions. Ann Pharmacother. 2012;46(5):625–33.
Espino DV, Bazaldua OV, Palmer RF, Mouton CP, Parchman ML, Miles TP, et al. Suboptimal medication use and mortality in an older adult community-based cohort: results from the Hispanic EPESE Study. J Gerontol A Biol Sci Med Sci. 2006;61(2):170–5.
Gurwitz JH, Field TS, Harrold LR, Rothschild J, Debellis K, Seger AC, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289(9):1107–16.
Rich MW. Pharmacotherapy of heart failure in the elderly: adverse events. Heart Fail Rev. 2012;17(4–5):589–95.
Muhlack DC, Hoppe LK, Weberpals J, Brenner H, Schottker B. The association of potentially inappropriate medication at older age with cardiovascular events and overall mortality: a systematic review and meta-analysis of cohort studies. J Am Med Dir Assoc. 2017;18(3):211–20.
Doogue MP, Polasek TM. Drug dosing in renal disease. Clin Biochem Rev. 2011;32(2):69–73.
Hassan Y, Al-Ramahi R, Abd Aziz N, Ghazali R. Drug use and dosing in chronic kidney disease. Ann Acad Med Singap. 2009;38(12):1095–103.
Verbeeck RK, Musuamba FT. Pharmacokinetics and dosage adjustment in patients with renal dysfunction. Eur J Clin Pharmacol. 2009;65(8):757–73.
Hartmann B, Czock D, Keller F. Drug therapy in patients with chronic renal failure. Dtsch Arztebl Int. 2010;107(37):6.
Via-Sosa MA, Lopes N, March M. Effectiveness of a drug dosing service provided by community pharmacists in polymedicated elderly patients with renal impairment–a comparative study. BMC Fam Pract. 2013;14:96.
Hanlon JT, Wang X, Handler SM, Weisbord S, Pugh MJ, Semla T, et al. Potentially inappropriate prescribing of primarily renally cleared medications for older veterans affairs nursing home patients. J Am Med Dir Assoc. 2011;12(5):377–83.
Nielsen AL, Henriksen DP, Marinakis C, Hellebek A, Birn H, Nybo M, et al. Drug dosing in patients with renal insufficiency in a hospital setting using electronic prescribing and automated reporting of estimated glomerular filtration rate. Basic Clin Pharmacol Toxicol. 2014;114(5):407–13.
Falconnier AD, Haefeli WE, Schoenenberger RA, Surber C, Martin-Facklam M. Drug dosage in patients with renal failure optimized by immediate concurrent feedback. J Gen Intern Med. 2001;16(6):369–75.
Chertow GM, Lee J, Kuperman GJ, Burdick E, Horsky J, Seger DL, et al. Guided medication dosing for inpatients with renal insufficiency. JAMA. 2001;286(22):2839–44.
van Dijk EA, Drabbe NR, Kruijtbosch M, De Smet PA. Drug dosage adjustments according to renal function at hospital discharge. Ann Pharmacother. 2006;40(7–8):1254–60.
Blix HS, Viktil KK, Moger TA, Reikvam A. Use of renal risk drugs in hospitalized patients with impaired renal function–an underestimated problem? Nephrol Dial Transplant. 2006;21(11):3164–71.
Parker K, Aasebo W, Stavem K. Potentially inappropriate medications in elderly haemodialysis patients using the STOPP criteria. Drugs Real World Outcomes. 2016;3(3):359–63.
Sheen SS, Choi JE, Park RW, Kim EY, Lee YH, Kang UG. Overdose rate of drugs requiring renal dose adjustment: data analysis of 4 years prescriptions at a tertiary teaching hospital. J Gen Intern Med. 2008;23(4):423–8.
Khanal A, Castelino RL, Peterson GM, Jose MD. Dose adjustment guidelines for medications in patients with renal impairment: how consistent are drug information sources? Intern Med J. 2014;44(1):77–85.
Hanlon JT, Aspinall SL, Semla TP, Weisbord SD, Fried LF, Good CB, et al. Consensus guidelines for oral dosing of primarily renally cleared medications in older adults. J Am Geriatr Soc. 2009;57(2):335–40.
Richardson MM, Nolin TD. A decade after the KDOQI CKD guidelines: impact on medication safety. Am J Kidney Dis. 2012;60(5):713–5.
Vidal L, Shavit M, Fraser A, Paul M, Leibovici L. Systematic comparison of four sources of drug information regarding adjustment of dose for renal function. BMJ. 2005;331(7511):263.
Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Inter Suppl. 2012;2:337–414.
Klarin I, Wimo A, Fastbom J. The association of inappropriate drug use with hospitalisation and mortality: a population-based study of the very old. Drugs Aging. 2005;22(1):69–82.
Lau DT, Kasper JD, Potter DE, Lyles A, Bennett RG. Hospitalization and death associated with potentially inappropriate medication prescriptions among elderly nursing home residents. Arch Intern Med. 2005;165(1):68–74.
Dedhiya SD, Hancock E, Craig BA, Doebbeling CC, Thomas J. Incident use and outcomes associated with potentially inappropriate medication use in older adults. Am J Geriatr Pharmacother. 2010;8(6):562–70.
Lu WH, Wen YW, Chen LK, Hsiao FY. Effect of polypharmacy, potentially inappropriate medications and anticholinergic burden on clinical outcomes: a retrospective cohort study. CMAJ. 2015;187(4):130.
Skoldunger A, Fastbom J, Wimo A, Fratiglioni L, Johnell K. Impact of inappropriate drug use on hospitalizations, mortality, and costs in older persons and persons with dementia: findings from the SNAC study. Drugs Aging. 2015;32(8):671–8.
Pozzi C, Lapi F, Mazzaglia G, Inzitari M, Boncinelli M, Geppetti P, et al. Is suboptimal prescribing a risk factor for poor health outcomes in community-dwelling elders? The ICARe Dicomano study. Pharmacoepidemiol Drug Saf. 2010;19(9):954–60.
Barnett K, McCowan C, Evans JM, Gillespie ND, Davey PG, Fahey T. Prevalence and outcomes of use of potentially inappropriate medicines in older people: cohort study stratified by residence in nursing home or in the community. BMJ Qual Saf. 2011;20(3):275–81.
Beer C, Hyde Z, Almeida OP, Norman P, Hankey GJ, Yeap BB, et al. Quality use of medicines and health outcomes among a cohort of community dwelling older men: an observational study. Br J Clin Pharmacol. 2011;71(4):592–9.
Lin HY, Liao CC, Cheng SH, Wang PC, Hsueh YS. Association of potentially inappropriate medication use with adverse outcomes in ambulatory elderly patients with chronic diseases: experience in a Taiwanese medical setting. Drugs Aging. 2008;25(1):49–59.
The Atherosclerosis Risk in Communities (ARIC). Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129(4):687–702.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Inter Suppl. 2013;3:1–150.
Ballew SH, Chen Y, Daya NR, Godino JG, Windham BG, McAdams-DeMarco M, et al. Frailty, Kidney Function, and Polypharmacy: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis. 2017;69(2):228–36.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
Fick DM, Semla TP, Beizer J, Brandt N, Dombrowski R, DuBeau CE, et al. American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227–46.
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–8.
Stevens LA, Nolin TD, Richardson MM, Feldman HI, Lewis JB, Rodby R, et al. Comparison of drug dosing recommendations based on measured GFR and kidney function estimating equations. Am J Kidney Dis. 2009;54(1):33–42.
Okparavero AA, Tighiouart H, Krishnasami Z, Wyatt CM, Graham H, Hellinger J, et al. Use of glomerular filtration rate estimating equations for drug dosing in HIV-positive patients. Antivir Ther. 2013;18(6):793–802.
Sharif-Askari FS, Syed Sulaiman SA, Saheb Sharif-Askari N, Hussain AAS. Development of an adverse drug reaction risk assessment score among hospitalized patients with chronic kidney disease. PLoS One. 2014;9(4):e95991.
Hug BL, Witkowski DJ, Sox CM, Keohane CA, Seger DL, Yoon C, et al. Occurrence of adverse, often preventable, events in community hospitals involving nephrotoxic drugs or those excreted by the kidney. Kidney Int. 2009;76(11):1192–8.
Page RL, O’Bryant CL, Cheng D, Dow TJ, Ky B, Stein CM, et al. Drugs that may cause or exacerbate heart failure: a scientific statement from the American Heart Association. Circulation. 2016;134(6):32.
Zhang L, Xu N, Xiao S, Arya V, Zhao P, Lesko LJ, et al. Regulatory perspectives on designing pharmacokinetic studies and optimizing labeling recommendations for patients with chronic kidney disease. J Clin Pharm. 2012;52(Suppl 1):90S.
Acknowledgements
Preliminary data from this study were presented in a spotlight poster session at the 33rd International Conference of Pharmacoepidemiology and Therapeutic Risk Management, Montreal, QC, Canada, 27–30 August 2017. The authors thank the staff and participants of the ARIC study for their important contributions
Author information
Authors and Affiliations
Contributions
Research idea and study design: AS, GCA, SHB, JC, MEG. Data analysis/interpretation: AS, GCA, SHB, JC, MEG. Statistical analysis: AS, MEG. Supervision or mentorship: GCA, JC, MEG. Each author contributed meaningfully to manuscript content during its preparation or revision, and accepts accountability for the overall work.
Corresponding author
Ethics declarations
Funding
Alex Secora, the principal author, is supported by grant T32 HL007024 from the NHLBI, National Institutes of Health; Morgan Grams is supported by grant K08DK092287 from the National Institute of Diabetes and Digestive and Kidney Diseases; and G. Caleb Alexander is supported by 1 U01 FD004977-02 from the US FDA. The ARIC study is performed as a collaborative investigation supported by contracts HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C from the NHLBI. The funding sources had no role in the design and conduct of the study, analysis or interpretation of the data, and preparation or final approval of the manuscript prior to publication.
Conflict of interest
Dr. G. Caleb Alexander is Chair of the FDA’s Peripheral and Central Nervous System Advisory Committee, has served as a paid advisor to IQVIA, serves on the advisory board of MesaRx Innovations, is a member of OptumRx’s National P&T Committee, and holds equity in Monument Analytics, a healthcare consultancy whose clients include the life sciences industry as well as plaintiffs in opioid litigation. This arrangement has been reviewed and approved by Johns Hopkins University in accordance with its conflict of interest policies. Alex Secora, G. Caleb Alexander, Shoshana H. Ballew, Josef Coresh and Morgan E. Grams declare that they have no conflicts of interest relevant to the content of this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Secora, A., Alexander, G.C., Ballew, S.H. et al. Kidney Function, Polypharmacy, and Potentially Inappropriate Medication Use in a Community-Based Cohort of Older Adults. Drugs Aging 35, 735–750 (2018). https://doi.org/10.1007/s40266-018-0563-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-018-0563-1