Abstract
Sacituzumab govitecan (sacituzumab govitecan-hziy; Trodelvy™) is a Trop-2-directed antibody conjugated to a topoisomerase I inhibitor (SN-38) that is being developed by Immunomedics for the treatment of solid tumours, including breast cancer. In April 2020, sacituzumab govitecan received accelerated approval in the USA for the treatment of adult patients with metastatic triple-negative breast cancer (mTNBC) who have received at least two prior therapies for metastatic disease. Sacituzumab govitecan is undergoing phase III development for breast cancer in the USA and EU, and phase II development for urothelial cancer. It is also being explored for brain metastases, glioblastoma, endometrial cancer and prostate cancer. This article summarizes the milestones in the development of sacituzumab govitecan leading to this first approval for mTNBC.
Similar content being viewed by others
An antibody-drug conjugate is being developed by Immunomedics for the treatment of solid tumours |
Received its first approval on 22 April 2020 in the USA |
Approved for use in adult patients with mTNBC who have received at least two prior therapies for metastatic disease |
1 Introduction
Sacituzumab govitecan (sacituzumab govitecan-hziy; Trodelvy™) is an antibody–drug conjugate developed by Immunomedics for the treatment of solid tumours, including breast and urothelial cancers [1]. Sacituzumab govitecan was developed by site-specific conjugation of the irinotecan active metabolite, SN-38 (govitecan), to a humanized monoclonal antibody (hRS7) against trophoblastic cell-surface antigen-2 (Trop-2); SN-38 is covalently linked to hRS7 via a hydrolysable CL2A linker [2,3,4,5]. Trop-2 is overexpressed in many solid tumours [3, 4] and has limited expression in normal tissues [6]. Trop-2 plays a role in oncogenesis and is associated with poor prognosis of several cancers, including breast cancer [7]. SN-38 is a moderately-toxic topoisomerase I inhibitor and therefore is conjugated to hRS7 at a high mean drug-to-antibody ratio (7.6) [3]. Use of a less toxic drug may improve therapeutic index of the formulation.

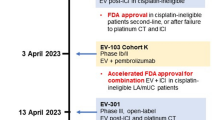
Key milestones in the development of sacituzumab govitecan, focusing on breast cancer. BLA Biologics License Application, mTNBC metastatic triple-negative breast cancer, Est estimated
Intravenous sacituzumab govitecan received accelerated approval in the USA on 22 April 2020 for the treatment of adult patients with metastatic triple-negative breast cancer (mTNBC) who have received at least two prior therapies for metastatic disease [8, 9]. The approval was based on results of a phase I/II trial (NCT01631552); continued approval will require demonstration of clinical benefit in a confirmatory phase III trial. The recommended dosage of sacituzumab govitecan is 10 mg/kg on days 1 and 8 of continuous 21-day treatment cycles until disease progression or unacceptable toxicity. The US prescribing information for sacituzumab govitecan carries a black box warning for neutropenia and diarrhoea [8].
The US FDA has granted sacituzumab govitecan breakthrough therapy designation for mTNBC [10], and fast track status for mTNBC [11], locally advanced or metastatic urothelial cancer [12], metastatic non-small cell lung cancer (NSCLC) [13] and small-cell lung cancer (SCLC) [11]. Sacituzumab govitecan has orphan drug designation for SCLC and pancreatic cancer in the USA [14] and pancreatic cancer in the EU [15]. Sacituzumab govitecan is being evaluated in phase III studies in breast cancer in the USA and EU, and in phase II studies in urothelial cancer. Additional investigator-initiated studies are exploring the activity of sacituzumab govitecan in endometrial cancer, prostate cancer, brain metastases and glioblastoma. In addition, clinical trials of sacituzumab govitecan in combination with PARP inhibitors and checkpoint inhibitors are underway.
1.1 Company Agreements
In April 2019, Immunomedics and Everest Medicines entered into an exclusive licensing agreement for the development and commercialisation of sacituzumab govitecan in South Korea, China, Hong Kong, Macao, Taiwan and Southeast Asia excluding Japan [16]. Immunomedics will receive upfront, milestone and royalty payments; Everest Medicines will be responsible for development and commercialisation costs [16].

Chemical structure of sacituzumab govitecan
In September 2018, Immunomedics signed a long-term manufacturing agreement with Samsung BioLogics, under which the latter will manufacture hRS7 [17]. In January 2018, Royalty Pharma acquired from Immunomedics royalty rights on global net sales of sacituzumab govitecan across all indications for $175 million [18].
In May 2017, Seattle Genetics agreed to terminate its license agreement with Immunomedics for sacituzumab govitecan and settle the associated litigation [19]. The agreement was signed in February 2017, under which Immunomedics was entitled to receive upfront, milestone and royalty payments; Seattle Genetics was responsible for initiating a phase III study in mTNBC and submission of the initial Biologics License Application, as well as for the development in other indications [20].
Immunomedics has collaboration agreements with:
-
Dana-Farber Cancer Institute to conduct two phase II studies of sacituzumab govitecan plus pembrolizumab in mTNBC and HR-positive/HER2-negative metastatic breast cancer (agreement signed in 2020) [21]
-
Roche for sacituzumab govitecan plus atezolizumab in TNBC (September 2019) [22]
-
GBG Forschungs GmbH for sacituzumab govitecan in high-risk post neoadjuvant patients with breast cancer (September 2019) [22]
-
Yale University School of Medicine for sacituzumab govitecan in endometrial cancer, as well as for preclinical studies of sacituzumab govitecan monotherapy and in combination with PARP inhibitors in gynaecological cancers (July 2018) [23]
-
Memorial Sloan Kettering Cancer Center for preclinical studies of sacituzumab govitecan monotherapy and in combination with EGFR and PI3K inhibitors and cisplatin (July 2018) [23]
-
Fred Hutchinson Cancer Research Center for preclinical studies of sacituzumab govitecan monotherapy and in combination with labetuzumab govitecan (July 2018) [23]
-
AstraZeneca for sacituzumab govitecan plus durvalumab in TNBC and urothelial cancer (July 2018) [24]
-
Clovis Oncology for sacituzumab govitecan plus rucaparib in mTNBC and urothelial cancer (June 2018) [25]
-
University of Wisconsin for sacituzumab govitecan in prostate cancer (January 2018) [26]
2 Scientific Summary
2.1 Pharmacodynamics
In vitro, sacituzumab govitecan has a mechanism of action similar to that of free SN-38; in addition, hRS7 may impart its own antibody-dependent cell-mediated cytotoxicity, although it has not been demonstrated clinically [3,4,5]. In vitro, sacituzumab govitecan delivers greater (up to 136-fold [3]) SN-38 than irinotecan [3, 27, 28]. A high level of SN-38 delivery may overcome Rad51-mediated homologous recombination repair of DNA breaks in Trop-2-expressing solid tumours, such as TNBC [28]. In addition to a greater delivery, sacituzumab govitecan delivers SN-38 in its most active nonglucuronidated form, which may partly explain the lower incidence of diarrhoea seen with sacituzumab govitecan than with irinotecan [3]. Sacituzumab govitecan has demonstrated potent in vitro and/or in vivo activity against TNBC [3, 4, 28] and a range of carcinomas, including cervical [29], endometrial [30], uterine and/or ovarian [31, 32], and NSCLC, squamous cell lung, colonic, pancreatic and prostatic [5] carcinomas. Pharmacodynamic exposure–response and temporal trends are unknown for sacituzumab govitecan [8].
Functional expression of ABCG2 is associated with resistance to sacituzumab govitecan in vitro; combining an ABCG2 inhibitor (YHO-13351) with sacituzumab govitecan was associated with improved survival versus no treatment in an ABCG2-positive, SN-38 resistant human gastric cancer xenograft model [33].
2.2 Pharmacokinetics
In patients with mTNBC, the mean distribution volume of sacituzumab govitecan after a single 10 mg/kg dose was 0.045 L/kg [8]. The mean half-life of sacituzumab govitecan and free SN-38 was 16 and 18 h, respectively; the clearance of sacituzumab govitecan was 0.002 L/h/kg [8]. Following the 10 mg/kg dosage, pharmacokinetics of sacituzumab govitecan and free SN-38 in patients with diverse metastatic cancers were broadly similar to those seen in patients with mTNBC [34].
There are no metabolism studies of sacituzumab govitecan [8]. SN-38 is metabolized by UGT1A1, with a glucuronide metabolite of SN-38 (SN-38G) detectable in patient serum. Patients who are homozygous for the UGT1A1*28 allele (which leads to reduced UGT1A1 enzyme activity) are at increased risk for neutropenia from sacituzumab govitecan. Sacituzumab govitecan exposure is similar between individuals with mild hepatic impairment and those with normal function; the effect of moderate or severe hepatic impairment is unknown, although these conditions may increase the exposure of SN-38 due to decreased UGT1A1 activity. There are no pharmacokinetic studies of sacituzumab govitecan in patients with renal impairment or end-stage renal disease, although renal elimination of SN-38 is known to be minimal. There are no formal drug interaction studies of sacituzumab govitecan or its components. UGT1A1 inhibitors or inducers are expected to increase or decrease SN-38 exposure, respectively; use of UGT1A1 inhibitors and inducers with sacituzumab govitecan should be avoided [8].
Features and properties of sacituzumab govitecan
Alternative names | hRS7-SN38 antibody drug conjugate; IMMU-132; Isactuzumab govitecan; Sacituzumab govitecan-hziy; TRODELVY; TROP-2-SN-38 |
Class | Antineoplastics; Camptothecins; Drug conjugates; Immunoconjugates; Immunotherapies; Indolizines; Monoclonal antibodies; Pyrans; Quinolines |
Mechanism of Action | Trop-2 directed antibody conjugated to a DNA topoisomerase I inhibitor |
Route of Administration | Intravenous |
Pharmacodynamics | Antibody–drug conjugate; delivers more SN-38 (irinotecan active metabolite) than irinotecan; delivers SN-38 in its most active nonglucuronidated form; potent in vitro and/or in vivo cytotoxicity against diverse solid tumours, including carcinomas |
Pharmacokinetics | Volume of distribution 0.045 L/kg, half-life 16 h and clearance 0.002 L/h/kg for whole product; half-life 18 h for free SN-38 |
Most frequent adverse events | Nausea, neutropenia, diarrhoea, fatigue, anaemia, vomiting, alopecia, constipation, rash, decreased appetite, and abdominal pain in patients with mTNBC |
ATC codes | |
WHO ATC code | L01 (Antineoplastic Agents) |
EphMRA ATC code | L1 (Antineoplastics) |
Chemical Name | (2R)-2-amino-3-[1-[[4-[[1-[2-[2-[2-[2-[2-[2-[2-[2-[2-[[2-[2-[[(2S)-6-amino-1-[4-[[(19S)-10,19-diethyl-7-hydroxy-14,18-dioxo-17-oxa-3,13-diazapentacyclo[11.8.0.02,11.04,9.015,20]henicosa-1(21),2,4(9),5,7,10,15(20)-heptaen-19-yl]oxycarbonyloxymethyl]anilino]-1-oxohexan-2-yl]amino]-2-oxoethoxy]acetyl]amino]ethoxy]ethoxy]ethoxy]ethoxy]ethoxy]ethoxy]ethoxy]ethoxy]ethyl]triazol-4-yl]methylcarbamoyl]cyclohexyl]methyl]-2,5-dioxopyrrolidin-3-yl]sulfanylpropanoic acid |
2.3 Therapeutic Trials
Sacituzumab govitecan showed encouraging antitumour activity in the first-in-human clinical trial in patients with metastatic solid tumours (NCT01631552; IMMU-132-01) [35]. In the phase I dose-escalation portion, sacituzumab govitecan was administered at 8, 10, 12 or 18 mg/kg on days 1 and 8 of a 3-week treatment cycle for up to 8 cycles, or until disease progression or unacceptable toxicity. Of 25 patients, two achieved partial responses (PRs), 16 had stable disease. Overall, three patients had a ≥ 30% reduction in their target lesions. The maximum tolerated dose was 12 mg/kg. The 8 and 10 mg/kg dosage levels were associated with acceptable tolerability in the first cycle, allowing repeated administrations. Consequently, the 8 and 10 mg/kg dosages were selected for phase II studies [35].
In the phase II dose-expansion portion of the IMMU-132–01 trial, 178 patients with advanced solid tumours were treated with sacituzumab govitecan 8 or 10 mg/kg [34]. Overall, the 10 mg/kg dosage was associated with numerically better objective response rate (ORR) and clinical benefit rate (CBR) than the 8 mg/kg dosage; therefore, the 10 mg/kg dosage was selected for further clinical studies in patients with solid tumours [34].
2.3.1 Breast Cancer
Sacituzumab govitecan was associated with an ORR of 33.3% (95% CI 24.6–43.1) [primary endpoint] in 108 heavily pretreated patients with mTNBC in the basket-design, open-label, single-group IMMU-132-01 trial [36]. The objective responses (assessed locally using RECIST version 1.1) included three complete responses (CR) and 33 PRs. The CBR (percent patients with CR, PR or stable disease for ≥ 6 months) was 45.4% (95% CI 35.8–55.2) and the median duration of response (DOR) was 7.7 months (95% CI 4.9–10.8). The median progression-free survival (PFS) was 5.5 months (95% CI 4.1–6.3) and the median overall survival (OS) was 13.0 months (95% CI 11.2–13.7). Sacituzumab govitecan was administered on days 1 and 8 of each 21-day cycle until disease progression or unacceptable toxic effects. The median duration of follow-up was 9.7 months (data cutoff December 2017) [36].
Consistent ORRs were seen with sacituzumab govitecan, regardless of oestrogen-receptor (ER) status in IMMU-132-01 [37]. In a pooled analysis of 162 patients with HER2-negative breast cancer (108 TNBC and 54 ER-positive), ORR was 33% (3 CRs, 50 PRs), median DOR was 8.3 months, PFS was 5.6 months and OS was 13.0 months. In the ER-positive subgroup, the ORR was 31% (17 PRs) and the median DOR was 7.4 months (median follow-up 10 months) [37].
In 69 patients who received a median of five prior therapies since diagnosis in IMMU-132-01, ORR was 30% (19 PRs, 2 CRs), CBR was 46% and the median DOR was 8.9 months [38]. Responses occurred early in the treatment course, with a median onset of 1.9 months. The median PFS and OS were 6.0 and 16.6 months, respectively [38].
The confirmatory multicentre, randomized, phase III ASCENT trial (NCT02574455) compared sacituzumab govitecan versus the physician’s choice of chemotherapy in patients with mTNBC who have failed ≥ 2 prior lines of therapy. This trial was stopped earlier than planned upon recommendation of an independent Data Safety Monitoring Committee because of compelling evidence of efficacy [39].
2.3.2 Urothelial Cancer
Sacituzumab govitecan showed clinical activity in patients with metastatic urothelial carcinoma in the IMMU-132-01 trial [40]. Patients had received at least one prior line of therapy. The ORR was 31% in the overall cohort (n = 45), 27% in those with visceral involvement (n = 33) and 23% in those previously treated with checkpoint inhibitors (n = 17). The CBR was 47% (n = 45). The median DOR was 12.9 months. The median PFS and OS were 7.3 and 16.3 months, respectively [40].
Sacituzumab govitecan was associated with an ORR of 29% (median follow-up 4.1 months; n = 35) in patients with platinum- or immunotherapy-resistant metastatic urothelial carcinoma (cohort 1) in an interim analysis of the open-label, multinational, phase II TROPHY-U-01 trial (NCT03547973) [41]. The ORR exceeded the prespecified Simon 2-stage rule of 5 or more responders among 35 patients at interim in cohort 1, permitting enrolment continuation. The objective responses included two confirmed CRs, six confirmed PRs and two unconfirmed PRs. In patients with liver involvement, the ORR was 25% (2 of 8). A reduction in the target lesion was seen in 74% (26 of 35) of patients [41].
2.3.3 Lung Cancer
In 36 patients with metastatic SCLC who received sacituzumab govitecan 10 mg/kg in the IMMU-132-01 trial, the ORR was 17%, CBR was 39% and the median DOR was 4.0 months; the median PFS and OS were 3.7 and 6.2 months, respectively [42]. In 54 patients with metastatic NSCLC who received sacituzumab govitecan 8 or 10 mg/kg, the ORR was 17% and the median DOR was 6 months; median PFS and OS were 5.2 and 9.5 months, respectively [43].
Key clinical trials of sacituzumab govitecan
Drug(s) | Indication | Phase | Status | Location(s) | Identifier | Sponsors |
|---|---|---|---|---|---|---|
Sacituzumab govitecan, chemotherapy | HR+/HER–mBC | III | Recruiting | Multinational | NCT03901339, EudraCT2018-004201-33, IMMU132-09, TROPICS-02 | Immunomedics |
Sacituzumab govitecan + immunotherapy | mTNBC | I/II | Recruiting | Multinational | NCT03424005, EudraCT2017-002038-21, CO40115, MORPHEUS-TNBC | Roche |
Sacituzumab govitecan + Talazoparib | mTNBC | I/II | Recruiting | USA | NCT04039230, 19-239 | Massachusetts General Hospital |
Sacituzumab govitecan, chemotherapy | mTNBC | III | Active, no longer recruiting | Multinational | NCT02574455, EudraCT2017-003019-21, IMMU132-05, ASCENT | Immunomedics |
Sacituzumab govitecan | Localised TNBC | II | Not yet recruiting | USA | NCT04230109, 19-578, NeoSTAR | Massachusetts General Hospital |
Sacituzumab govitecan | Endometrial cancer | II | Recruiting | USA | NCT04251416, 2000026850 | Yale |
Sacituzumab govitecan | Epithelial cancers | I/II | Active, no longer recruiting | USA | NCT01631552, VICCPHI1394, IM-T-IMMU132-01, IMMU-132-01 | Immunomedics |
Sacituzumab govitecan | Prostate cancer | II | Recruiting | USA | NCT03725761, SMPH-MEDICINE-HEM-ONC | University of Wisconsin |
Sacituzumab govitecan, rucaparib | Solid tumours | I/II | Recruiting | USA | NCT03992131, CO338-098, SEASTAR | Clovis Oncology |
Sacituzumab govitecan | Solid tumours | II | Halted due to COVID 19 | USA | NCT03964727, Immu132-11, TROPICS-03 | Immunomedics |
Sacituzumab govitecan ± pembrolizumab | Urothelial cancer | II | Recruiting | Multinational | NCT03547973, IMMU132-06, TROPHY U-01 | Immunomedics |
Sacituzumab govitecan | Brain metastases, glioblastoma | I | Recruiting | USA | NCT03995706, CTMS19-0069, HSC20190378H | The University of Texas Health Science Center at San Antonio |
2.4 Adverse Events
In the phase II dose-expansion portion of IMMU-132-01, in 89 patients with advanced epithelial cancers who received sacituzumab govitecan 10 mg/kg, the most common (incidence ≥ 5%) all-cause grade ≥ 3 adverse events (AEs) were neutrophil count decrease (36%), WBC decrease (12%), anaemia (12%), diarrhoea (10%), fatigue (9%) and febrile neutropenia (7%) [34]. Neutropenia was the most common dose-limiting toxicity and it was not correlated with serum govitecan levels or UGT1A1 genotype. The safety profile of sacituzumab govitecan was generally predictable and manageable [34].
Among 108 patients with mTNBC receiving sacituzumab govitecan in IMMU-132-01, grade 3 AEs occurred in 66% of patients; the most common (incidence ≥ 5%) were neutropenia (26%), anaemia (11%), hypophosphatemia (9%), WBC decrease (8%), diarrhoea (8%), nausea (6%) and vomiting (6%) [36]. Grade 4 AEs occurred in 19% of patients and included neutropenia (16%) and WBC decrease (3%) [36]. Serious adverse reactions occurred in 31% of patients and the most common (incidence > 1%) were febrile neutropenia (6%) vomiting (5%), nausea (3%), dyspnoea (3%), diarrhoea (4%), anaemia (2%), pleural effusion (2%), neutropenia (2%), pneumonia (2%) and dehydration (2%) [8]. Adverse reactions led to treatment interruption in 45% of patients, most commonly due to neutropenia (33%) [8]. Two patients discontinued treatment because of treatment-related AEs [36]. Patients had received a mean 9.6 cycles of sacituzumab govitecan over a median 5.1 months [36].
In 45 patients with metastatic urothelial carcinoma who received sacituzumab govitecan in the IMMU-132-01 trial, the most common (incidence ≥ 5%) grade ≥ 3 AEs included neutropenia/neutrophil count decreased (38%), anaemia (11%), hypophosphatemia (11%), diarrhoea (9%), fatigue (9%) and febrile neutropenia (7%) [40].
The tolerability profile of sacituzumab govitecan in patients with urothelial carcinoma in the TROPHY-U-01 trial was consistent with that of other studies. Grade ≥ 3 treatment-related AEs included neutropenia (23%), anaemia (17%), febrile neutropenia (11%) and diarrhoea (11%) [41].
In patients with lung cancer who received sacituzumab govitecan in the IMMU-132-01 trial, grade ≥ 3 AEs included neutropenia (28%), diarrhoea (7%), nausea (7%), fatigue (6%) and febrile neutropenia (4%) in those with metastatic NSCLC [43], and neutropenia (34%), fatigue (13%), diarrhoea (9%) and anaemia (6%) in those with metastatic SCLC [42].
As with all therapeutic proteins, sacituzumab govitecan has a potential for immunogenicity. Persistent anti-sacituzumab govitecan antibodies were detected in 2 of 106 (≈2%) of patients with mTNBC [8].
2.5 Ongoing Clinical Trials
The IMMU-132-01 trial is still ongoing. An open-label, randomized, phase III trial (NCT03901339; TROPiCS-02) is comparing sacituzumab govitecan with the physician’s choice of chemotherapy in patients with HR-positive/HER2-negative metastatic breast cancer [44]. A phase I/II trial (NCT04039230) is evaluating sacituzumab govitecan in combination with a PARP inhibitor (talazoparib) in patients with metastatic breast cancer. In addition, a phase I/II, open-label, multicentre, randomized umbrella study (NCT03424005; Morpheus-TNBC) is evaluating the efficacy and safety of multiple immunotherapy-based treatment combinations, including sacituzumab govitecan, in patients with mTNBC.
The TROPHY U-01 trial in urothelial carcinoma is ongoing [41]. Sacituzumab govitecan is also being evaluated in investigator-initiated phase II trials in endometrial carcinoma (NCT04251416) and prostate cancers (NCT03725761), as well as in an investigator-initiated early phase study (NCT03995706) in brain metastases or glioblastoma [45].
3 Current Status
Sacituzumab govitecan received its first approval on 22 April 2020 for mTNBC in the USA.
References
Immunomedics. Advanced antibody-based therapeutics [presentation]. 2017. https://www.immunomedics.com. Accessed 20 May 2020.
Goldenberg DM, Stein R, Sharkey RM. The emergence of trophoblast cell-surface antigen 2 (Trop-2) as a novel cancer target. Oncotarget. 2018;9(48):28989–9006.
Goldenberg DM, Cardillo TM, Govindan SV, et al. Trop-2 is a novel target for solid cancer therapy with sacituzumab govitecan (IMMU-132), an antibody-drug conjugate (ADC). Oncotarget. 2015;6(26):22496–512.
Cardillo TM, Govindan SV, Sharkey RM, et al. Sacituzumab govitecan (IMMU-132), an anti-Trop-2/SN-38 antibody-drug conjugate: characterization and efficacy in pancreatic, gastric, and other cancers. Bioconjugate Chem. 2015;26(5):919–31.
Cardillo TM, Govindan SV, Sharkey RM, et al. Humanized anti-Trop-2 IgG-SN-38 conjugate for effective treatment of diverse epithelial cancers: preclinical studies in human cancer-xenograft models and monkeys. Clin Cancer Res. 2011;2011:clincanres.2939.010.
Ponde N, Aftimos P, Piccart M. Antibody-drug conjugates in breast cancer: a comprehensive review. Curr Treat Options Oncol. 2019;20(5):37.
Ambrogi F, Fornili M, Boracchi P, et al. Trop-2 is a determinant of breast cancer survival. PLoS ONE. 2014;9(5):e96993.
Immunomedics. TRODELVYTM (sacituzumab govitecan-hziy) for injection, for intravenous use: US Prescribing Information. 2020. https://www.fda.gov. Accessed 20 May 2020.
US FDA. FDA grants accelerated approval to sacituzumab govitecan-hziy for metastatic triple negative breast cancer [media release]. 22 Apr 2020. https://www.fda.gov.
Immunomedics. U.S. Food and Drug Administration (FDA) grants breakthrough therapy designation to immunomedics for sacituzumab govitecan for the treatment of patients with triple-negative breast cancer [media release]. 5 Feb 2016. https://www.immunomedics.com.
Immunomedics. Immunomedics awarded fast track designation by FDA for sacituzumab govitecan (IMMU-132) for triple-negative breast cancer therapy [media release]. 5 Jan 2015. https://www.immunomedics.com.
Immunomedics. Correction - FDA grants fast track designation to sacituzumab govitecan for locally-advanced or metastatic urothelial cancer [media release]. 7 Apr 2020. https://www.immunomedics.com.
Immunomedics. Immunomedics awarded fast track designation by FDA for sacituzumab govitecan for non-small cell lung cancer therapy [media release]. 5 Jan 2015. https://www.immunomedics.com/.
Orphan drug product desgination [database on the Internet]. 2020. https://www.fda.gov/.
Immunomedics. Immunomedics announces European orphan drug designation for sacituzumab govitecan for pancreatic cancer treatment [media release]. 20 Oct 2014. https://www.immunomedics.com.
Everest Medicines, Immunomedics. Immunomedics and Everest Medicines announce exclusive license agreement for sacituzumab govitecan in East and Southeast Asia excluding Japan [media release]. 29 Apr 2019. https://www.everestmedicines.com.
Immunomedics. Immunomedics and Samsung BioLogics announce strategic manufacturing partnership [media release]. 12 Sep 2018. https://www.immunomedics.com.
Immunomedics. Immunomedics and Royalty Pharma announce royalty funding and stock purchase agreements totalling $250 million [media release]. 8 Jan 2018.
Seattle Genetics. Seattle Genetics terminates license agreement with Immunomedics for sacituzumab govitecan (IMMU-132) [media release]. 5 May 2017. https://www.seattlegenetics.com.
Seattle G. Seattle Genetics announces global license agreement with immunomedics for sacituzumab govitecan (IMMU-132), a promising late-stage ADC for solid tumors [media release]. 5 May 2017. https://www.seattlegenetics.com.
Immunomedics. Immunomedics reports first quarter 2020 results and provides corporate update [media release]. 6 May 2020.
Immunomedics. Immunomedics provides corporate update [media release]. 28 Sep 2019. https://www.immunomedics.com.
Immunomedics. Immunomedics announces multiple clinical and preclinical collaborations with prominent cancer research institutions [media release]. 30 Jul 2018. https://www.immunomedics.com.
Immunomedics. Immunomedics announces clinical collaboration with AstraZeneca in first-line triple-negative breast and urothelial cancers [media release]. 23 Jul 2018. https://www.immunomedics.com.
Clovis Oncology. Clovis Oncology and Immunomedics announce planned clinical collaboration to study combination therapies in metastatic triple-negative breast and urothelial cancers [media release]. 3 Jun 2018. https://www.clovisoncology.com.
Immunomedics. Immunomedics announces agreement with University of Wisconsin Carbone Cancer Center to expand sacituzumab govitecan (IMMU-132) into prostate cancer [media release]. 11 Jan 2018. https://www.immunomedics.com.
Sharkey RM, McBride WJ, Cardillo TM, et al. Enhanced delivery of SN-38 to human tumor xenografts with an anti-Trop-2-SN-38 antibody conjugate (sacituzumab govitecan). Clin Cancer Res. 2015;2015:clincanres.0670.2015.
Cardillo TM, Mostafa AA, Rossi DL, et al. Treatment of high Trop-2-expressing triple-negative breast cancer (TNBC) with sacituzumab govitecan (IMMU-132) overcomes homologous recombination repair (HRR) rescue mediated by Rad51 [abstract no. 3193]. Cancer Res. 2017;77(13 Suppl):1.
Zeybek B, Manzano A, Bianchi A, et al. Cervical carcinomas that overexpress human trophoblast cell-surface marker (Trop-2) are highly sensitive to the antibody-drug conjugate sacituzumab govitecan. Sci Rep. 2020;10(1):973.
Perrone E, Manara P, Lopez S, et al. Sacituzumab govitecan, an antibody-drug conjugate targeting trophoblast cell-surface antigen 2, shows cytotoxic activity against poorly differentiated endometrial adenocarcinomas in vitro and in vivo. Mol Oncol. 2020;14(3):645–56.
Lopez S, Perrone E, Bellone S, et al. Preclinical activity of sacituzumab govitecan (IMMU-132) in uterine and ovarian carcinosarcomas. Oncotarget. 2020;11(5):560–70.
Han C, Perrone E, Zeybek B, et al. In vitro and in vivo activity of sacituzumab govitecan, an antibody-drug conjugate targeting trophoblast cell-surface antigen 2 (Trop-2) in uterine serous carcinoma. Gynecol Oncol. 2020;156(2):430–8.
Chang CH, Wang Y, Zalath M, et al. Combining ABCG2 inhibitors with IMMU-132, an anti-Trop-2 antibody conjugate of SN-38, overcomes resistance to SN-38 in breast and gastric cancers. Mol Cancer Ther. 2016;15(8):1910–9.
Ocean AJ, Starodub AN, Bardia A, et al. Sacituzumab govitecan (IMMU-132), an anti-Trop-2-SN-38 antibody-drug conjugate for the treatment of diverse epithelial cancers: safety and pharmacokinetics. Cancer. 2017;123(19):3843–54.
Starodub AN, Ocean AJ, Shah MA, et al. First-in-human trial of a novel anti-Trop-2 antibody-SN-38 conjugate, sacituzumab govitecan, for the treatment of diverse metastatic solid tumors. Clin Cancer Res. 2015;21(17):3870–8.
Bardia A, Mayer IA, Vahdat LT, et al. Sacituzumab govitecan-hziy in refractory metastatic triple-negative breast cancer. N Engl J Med. 2019;380(8):741–51.
Kalinsky K, Isakoff SJ, Tolaney SM, et al. Safety and efficacy of sacituzumab govitecan (anti-Trop-2-SN-38 antibody-drug conjugate) as ≥3rd-line therapeutic option for treatment-refractory HER2-negative metastatic breast cancer (HER2Neg mBC) [abstract no. P2-11-01]. Cancer Res. 2018;79(4 Suppl):1.
Bardia A, Mayer IA, Diamond JR, et al. Efficacy and safety of anti-Trop-2 antibody drug conjugate sacituzumab govitecan (IMMU-132) in heavily pretreated patients with metastatic triple-negative breast cancer. J Clin Oncol. 2017;35(19):2141–8.
Immunomedics. Immunomedics announces ASCENT study to be stopped for compelling efficacy [media release]. 6 Apr 2020. https://www.immunomedics.com.
Tagawa ST, Faltas BM, Lam ET, et al. Sacituzumab govitecan (IMMU-132) in patients with previously treated metastatic urothelial cancer (mUC): results from a phase I/II study [abstract no. 354]. J Clin Oncol. 2019;37(7 Suppl):5.
Tagawa ST, Balar A, Petrylak DP, et al. Initial results from TROPHY-U-01: a phase II open-label study of sacituzumab govitecan in patients (Pts) with metastatic urothelial cancer (mUC) after failure of platinum-based regimens (PLT) or immunotherapy [abstract no. LBA55]. Ann Oncol. 2019;30(Suppl 5):v890–v1.
Gray JE, Heist RS, Starodub AN, et al. Therapy of small cell lung cancer (SCLC) with a topoisomerase-I-inhibiting antibody-drug conjugate (ADC) targeting Trop-2, sacituzumab govitecan. Clin Cancer Res. 2017;23(19):5711–9.
Heist RS, Guarino MJ, Masters G, et al. Therapy of advanced non-small-cell lung cancer with an SN-38-anti-Trop-2 drug conjugate, sacituzumab govitecan. J Clin Oncol. 2017;35(24):2790–7.
Rugo HS, Bardia A, Tolaney SM, et al. TROPiCS-02: a phase III study investigating sacituzumab govitecan in the treatment of HR+/HER2- metastatic breast cancer. Future Oncol. 2020;16(12):705–15.
Brenner AJ, Floyd J, Surapaneni P, et al. CNS penetration and preliminary efficacy of sacutizumab govitecan in breast brain metastasis and glioblastoma: a surgical study [abstract no. 437TiP]. Ann Oncol. 2019;30(Suppl 5):v158.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflict of interest
During the peer review process the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes resulting from any comments received were made by the authors on the basis of scientific completeness and accuracy. Yahiya Y. Syed is a salaried employee of Adis International Ltd/Springer Nature, is responsible for the article content and declares no relevant conflicts of interest.
Additional information
Enhanced material for this AdisInsight Report can be found at https://doi.org/10.6084/m9.figshare.12382289.
This profile has been extracted and modified from the AdisInsight database. AdisInsight tracks drug development worldwide through the entire development process, from discovery, through pre-clinical and clinical studies to market launch and beyond.
Rights and permissions
About this article
Cite this article
Syed, Y.Y. Sacituzumab Govitecan: First Approval. Drugs 80, 1019–1025 (2020). https://doi.org/10.1007/s40265-020-01337-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-020-01337-5