Abstract
Background
In controlled clinical trials, compared with placebo, a significantly greater proportion of participants using lasmiditan to treat a migraine attack achieved 2-h pain freedom (PF) and experienced ≥ 1 treatment-emergent adverse event (TEAE).
Objective
To better inform clinicians about treatment expectations by evaluating the association between TEAEs and efficacy outcomes after lasmiditan treatment.
Methods
Pooled data from SAMURAI, SPARTAN, MONONOFU, and CENTURION were analyzed. A common TEAE (CTEAE) was defined as occurring in ≥ 2% in the overall population. Central nervous system (CNS)-CTEAEs were based on Medical Dictionary for Regulatory Activities.
Results
At 2 h, a significantly higher percentage of lasmiditan 200 mg-treated participants who achieved PF experienced ≥ 1 CTEAE than non-responders who continued to experience moderate/severe pain (48.2% vs. 28.7%, respectively). Correspondingly, a significantly higher percentage of lasmiditan 200 mg-treated participants who experienced ≥ 1 CTEAE achieved PF at 2 h than those who did not (39.0% vs. 30.2%, respectively). Similar results were generally observed with individual CNS-CTEAEs, but for non-CNS-CTEAEs, this pattern was less evident or in the opposite direction. No consistent differences were observed for migraine-related functional disability freedom. The percentage of participants with improved patient global impression of change (PGIC) was greater with a CNS-CTEAE versus no CNS-CTEAE.
Conclusions
Those who had PF at 2 h were more likely to experience a CNS-CTEAE, and those with CNS-CTEAEs were more likely to experience PF. The occurrence of CTEAEs did not seem to negatively affect disability freedom or PGIC.
ClinicalTrials.gov Registration
SAMURAI (NCT02439320), SPARTAN (NCT02605174), MONONOFU (NCT03962738), CENTURION (NCT03670810), ClinicalTrials.gov: NCT02439320, NCT02605174, NCT03962738, NCT03670810
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The likelihood of experiencing a central nervous system common treatment-emergent adverse event (CNS-CTEAE) was greater in those who achieved pain freedom than in those with moderate/severe pain at 2 h, but more than 50% of participants with pain freedom did not have a CNS-CTEAE. |
The incidence of pain freedom was greater for those who experienced a CNS-CTEAE, but the absence of a CNS-CTEAE did not equate to lack of efficacy. |
The occurrence of a CNS-CTEAE was not associated with a lower likelihood of achieving disability freedom or improved patient global impression of change. |
1 Introduction
Lasmiditan is a highly selective, first-in-class ditan that exerts its therapeutic effects through agonist action on serotonin 1F (5-HT1F) receptors located in the peripheral and central nervous system [1]. In previous trials, in comparison with placebo, treatment with lasmiditan (50 mg, 100 mg, or 200 mg) resulted in a significantly higher proportion of participants achieving pain freedom [2,3,4], freedom from their most bothersome symptom [2,3,4], migraine-related functional disability freedom [2, 5], and patient global impression of change (PGIC) of much better or very much better (improved PGIC) [4] at 2 h post-dose. Adverse events were more common with lasmiditan compared to placebo and were generally mild or moderate in severity. The most common treatment-emergent adverse events (TEAEs) were dizziness, paresthesia, somnolence, fatigue, nausea, muscular weakness, and hypoesthesia. These TEAEs were generally transient and self-limiting. Many of the most common TEAEs were central nervous system (CNS)-related, consistent with entry of lasmiditan into the CNS [6]. Both efficacy and adverse events were dose related, with higher doses of lasmiditan associated with a greater incidence of pain freedom at 2 h and increased incidence of TEAEs.
The association between efficacy outcomes and TEAEs has been a topic of interest across therapeutic areas. This information helps clinicians and their patients make trade-off decisions when considering a treatment that offers an opportunity for efficacy and a potential for adverse events [7]. In migraine, a study with triptans demonstrated that certain CNS-TEAEs were more prevalent in headache responders than non-responders, and that the percentage of participants obtaining pain freedom at 2 h was higher in those who experienced a CNS-TEAE than those who did not [8]. These associations have also been explored with lasmiditan. Previous analyses of lasmiditan Phase 3 studies showed that participants who reported dizziness, fatigue, paresthesia, or somnolence achieved 2-h pain freedom at numerically higher rates than those not reporting the symptom [5, 6, 9]. It has also been shown that the frequency of TEAEs generally decreased with subsequent attacks treated with the same lasmiditan dose [10, 11]. Furthermore, for participants who increased their lasmiditan dose for treatment of a subsequent migraine attack, the change in incidence of TEAEs was less than the increase in incidence of efficacy outcomes [7].
Previous lasmiditan analyses did not investigate the frequency of TEAEs in participants based on their pain outcome nor address the timing of the TEAEs relative to achieving pain freedom or other efficacy outcomes. The objective of this post hoc analysis was to further evaluate the association and relative timing of TEAE onset with efficacy outcomes after lasmiditan treatment to better inform clinicians about treatment expectations. The current analyses also expand on previous results from SAMURAI [12] and SPARTAN [4] by adding two additional studies (MONONOFU [13] and CENTURION [10]).
2 Methods
2.1 Participants and Study Design
All studies were prospective, multicenter, randomized, double-blind, controlled trials in which adult participants with migraine with or without aura treated one or more migraine attacks with lasmiditan or placebo on an outpatient basis. Inclusion and exclusion criteria were similar for all trials: history of migraine for at least 1 year, three to eight migraine attacks per month, and disabling migraine as defined by a Migraine Disability Assessment score ≥ 11. SAMURAI excluded participants with known coronary artery disease, clinically significant arrhythmia, and uncontrolled hypertension, while SPARTAN, MONONOFU, and CENTURION did not. Full details can be found in the primary reports from the studies [4, 10, 12, 13].
SAMURAI (conducted at 99 sites in the USA) and SPARTAN (conducted at 125 sites in the USA, the UK, and Germany) were Phase 3 studies [4, 12]. Participants were randomized to treat a single migraine attack with lasmiditan 50 mg (SPARTAN only), 100 mg, 200 mg, or placebo.
MONONOFU was a Phase 2 study of Japanese adult participants. Participants were asked to treat a single migraine attack with study intervention and were randomized in a 7:3:7:6 ratio to placebo, lasmiditan 50 mg, 100 mg, and 200 mg [13].
CENTURION was a modified-parallel, Phase 3 study across four migraine attacks [10]. Participants were randomized in a 1:1:1 ratio to lasmiditan 200 mg, lasmiditan 100 mg, or a control group (that received placebo for three of the four attacks, and lasmiditan 50 mg for either the third or fourth attack in a randomized, blinded fashion). For comparability with other studies only the first treated attack was included in the analysis.
The studies were carried out in accordance with the International Conference on Harmonisation Good Clinical Practice guidelines and local regulatory requirements. The protocols were approved by an institutional review board or independent ethics committee at each study site. Written informed consent for study participation was obtained from each patient prior to the start of the study.
2.2 Procedures
Data collection and adverse event coding were conducted as described [4, 10, 12, 13]. Briefly, participants recorded the date and time of migraine onset. They were instructed to treat pain of moderate or severe intensity and to record the level of head pain in an electronic diary at baseline and at specified post-treatment intervals (including 30, 60, 90 (except for CENTURION), and 120 min). Head pain was assessed using the International Headache Society 4-point headache intensity rating scale: none, mild, moderate, or severe [14]. The primary endpoints of the studies were assessed 2 h post-treatment.
Pain improvement was also assessed on a continuous time scale by asking participants “Has headache relief become meaningful?” If the participant answered “Yes,” they were then asked the time at which headache relief became meaningful to them, followed by the question, “Have you been headache pain-free?” If the answer was “Yes,” they were then asked the time that they became pain-free. These questions were asked at every designated time point until a “Yes” answer was given.
Migraine-related functional disability (disability) was assessed by asking participants, “How much is your migraine interfering with your normal activities?” Response options were “not at all,” “mild interference,” “marked interference,” and “need complete bed rest.” Freedom from migraine-related functional disability (disability) was defined as having disability “not at all.”
PGIC is an integrated measure of drug efficacy and tolerability that captures the patient’s view of improvement or decline in overall well-being after treatment [5]. PGIC was assessed at 2 h with the question “How do you feel after taking study medication?” Responses were recorded using a 7-point Likert scale, ranging from “very much better” to “very much worse,” and participants who reported “much better” or “very much better” were considered to have improved with treatment.
Adverse events were captured by asking participants if they felt “anything unusual” since taking the study medication that they had not felt with a migraine before; if “Yes” in SAMURAI and SPARTAN, they received a follow-up phone call from the site; in CENTURION and MONONOFU, they were instructed to record relevant information in a paper journal. A TEAE was defined as an event that started or worsened after any dose of study medication and occurred within 48 h after dosing.
2.3 Statistical Analyses
The analyses were conducted using pooled data from SAMURAI, SPARTAN, MONONOFU, and CENTURION (using data from the first eligibly treated migraine attack) [4, 10, 12, 13]. For each efficacy analysis, the population was composed of all randomized participants who took at least one dose of study drug and recorded any post-dose assessment of the relevant efficacy endpoint. The safety population (all participants who were randomized and received at least one dose of study drug) was used to determine common TEAEs (CTEAEs) as well as demographic and baseline characteristics. A CTEAE was defined as any TEAE occurring in ≥ 2% in the overall population after rounding. The top five CTEAEs were assessed individually. For this post hoc analysis, a CTEAE was categorized as CNS-related if it was a member of the Neurological Disorders NEC (not elsewhere classified) High Level Group based on Medical Dictionary for Regulatory Activities version 24.0. Therefore, although fatigue is considered by some to be CNS-related, for the purposes of this study it is categorized as not CNS-related. Of the five CTEAEs, dizziness, somnolence, and paresthesia were considered CNS-CTEAEs.
Subgroup analyses were conducted for the incidence of CTEAEs for: multiple mutually exclusive patient categories based on the head pain status at 2 h (only those with moderate/severe pain at baseline); disability-free (Yes and No); and PGIC rating as “very much better” or “much better” (Yes and No). The mutually exclusive pain-related subgroups were pain freedom, mild pain, and moderate/severe pain at 2 h after dosing. Participants who took additional intervention (over-the-counter or approved rescue medication) at or before 2 h were included in the moderate/severe group.
In addition, participants were categorized into subgroups based on the presence or absence of a CTEAE within 48 h after the first dose (Yes vs. No CTEAE). Participants with CTEAEs were further classified into CTEAE onset occurring at or before 2 h versus after 2 h. CTEAEs with missing start date/time or dosing date/time were not included in the corresponding analysis.
Subgroup analyses with treatment and subgroup interaction terms for treatment comparison across subgroups were performed on the proportion of participants who achieved efficacy responses, using a logistic regression model with treatment, study, subgroup, and subgroup-by-treatment interaction. The treatment comparisons between lasmiditan doses and placebo within a subgroup were evaluated using the Mantel-Haenszel method stratified by study. The subgroup comparison in a treatment group was similarly assessed. Subgroup effects in a treatment group were presented using odds ratios and associated 95% confidence intervals. A p value < 0.05 was considered statistically significant. SAS Enterprise Guide 7.1 (SAS Institute, Cary, NC, USA) statistical package was used for analyses.
To better understand the timing of onset of a CTEAE relative to the timing of change in headache intensity, individual patient-level data were assessed. Of those with moderate or severe pain at baseline and at least one post-baseline pain assessment, the distribution of those with and without a CTEAE was plotted on an inner ring of a donut chart. On the outer ring of the donut chart, the distribution of these participants was further explored. For those who experienced a CTEAE, the distribution of CTEAE onset (≤ 2 h, > 2 h, and missing a complete onset time) was plotted. For those who did not experience a CTEAE, the pain level at 2 h was plotted.
Those who experienced a CTEAE at or before 2 h were then included in a rainbow chart. For this analysis, the onset of TEAEs was plotted against assessment time points when headache intensity information was collected. Missing headache intensity was imputed using the last non-missing observation.
Lastly, the onset of CTEAEs versus the patient-reported time of meaningful pain improvement or pain freedom was assessed. CTEAE onset was classified as “before,” simultaneous “with,” or “after” the time of first achieving each pain outcome. The number and percentage of participants in each onset category were reported over time.
3 Results
3.1 Participants
Demographics and baseline characteristics of participants in the safety population (6602 patients in total) are presented in Table 1 and were consistent across treatments. The majority of participants were White, female, and the age range was 18–81 years. There were some differences in regions (Table 1) and countries (Online Supplemental Materials (OSM) Table 1) across treatments due to the geographies where the trials were conducted, and only SPARTAN and MONONOFU included the 50 mg dose (for the first attack in CENTURION, participants were not assigned 50 mg lasmiditan).
3.2 Summary of Common Treatment-Emergent Adverse Events (CTEAEs)
The CTEAEs in the overall population are shown in Table 2. Only the five most frequent CTEAEs were investigated separately. In the placebo cohort, 187 participants (9.5%) had ≥ 1 CTEAE, 67 participants (3.4%) had dizziness, 45 participants (2.3%) had somnolence, 32 participants (1.6%) had paresthesia, 45 participants (2.3%) had nausea, and 18 participants (0.9%) had fatigue. With lasmiditan (pooled doses), 1,595 participants (34.5%) had ≥1 CTEAE, 892 participants (19.3%) had dizziness, 324 participants (7.0%) had somnolence, 291 participants (6.3%) had paresthesia, 219 participants (4.7%) had nausea, and 216 participants (4.7%) had fatigue (Table 2).
3.3 Efficacy Outcomes
Across all of the studies, 2-h pain freedom was dose-dependent: 15.5% with placebo, 27.3% with 50 mg lasmiditan, 29.0% with 100 mg lasmiditan, and 33.9% with 200 mg lasmiditan. The incidence of 2-h moderate/severe pain was 44.8% with placebo, 30.3% with 50 mg lasmiditan, 24.3% with 100 mg lasmiditan, and 23.8% with 200 mg lasmiditan (data derived from OSM Table 2)
3.4 CTEAEs in Participants Who Experienced a Given Efficacy Outcome
The likelihood of experiencing a CTEAE within 48 h post-dose in participants who reported a 2-h pain intensity, migraine-associated functional disability freedom, and PGIC “much better” or “very much better” versus those who did not was assessed.
3.4.1 CTEAEs in Those Who Did or Did Not Have Pain Improvement
The occurrence of ≥1 CTEAE in lasmiditan 200 mg-treated participants was significantly greater when participants experienced pain freedom (48.2% Yes > 1 CTEAE) or mild pain (49.3% Yes > 1 CTEAE) versus moderate/severe pain (28.7% Yes > 1 CTEAE) at 2 h (data derived from OSM Table 2). This increase in percentage of lasmiditan 200 mg-treated participants experiencing ≥ 1 CTEAE with pain improvement (pain freedom or mild pain) versus moderate/severe pain at 2 h was also significant for individual CNS-CTEAEs (dizziness, somnolence, and paresthesia), and fatigue (pain-free only), but not nausea (these results and those of other treatment arms are shown in Fig. 1a). Participants who improved to mild pain or were pain-free at 2 h had a similar or lower likelihood of experiencing nausea compared to participants with moderate/severe pain at 2 h post-dose (Fig. 1a, OSM Table 2).
(a). The percentage of participants in each pain group experiencing the indicated CTEAE within 48 h. Participants who achieve pain freedom or improve to mild pain were more likely to experience CNS-CTEAEs. *p < 0.05, **p < 0.01, ***p < 0.001 versus M/S. The only treatment by subgroup interaction p values < 0.1 were ≥ 1 CTEAE (0.021) and dizziness (0.033). (b) The incidence of CTEAEs is similar in those who do and do not achieve disability freedom. *p < 0.05, **p < 0.01, ***p < 0.001 Yes versus No disability freedom. The only treatment by subgroup interaction p value < 0.1 was for nausea (0.087). (c) The incidence of CNS-CTEAEs is similar in those who experienced improved PGIC (rating of “much better” or “very much better” vs. those who did not (all other ratings)). * p < 0.05, ** p < 0.01, *** p < 0.001 Yes versus No PGIC. No treatment by subgroup interaction p-values <0.1 were identified. CNS central nervous system, CTEAE common treatment-emergent adverse event, IMP improved to mild pain, L lasmiditan, M/S severe/moderate pain, PBO placebo, PF pain-free, PGIC patient global impression of change, TEAE treatment-emergent adverse event
3.4.2 TEAEs in Those Who Were or Were Not Functional Disability-Free
The percentages of participants experiencing a CTEAE were generally similar in those who were or were not disability-free at 2 h (Fig. 1b, OSM Table 3). The percentage of those experiencing nausea was higher in those that did not become disability-free.
3.4.3 TEAEs in Those Who Were or Were Not Patient Global Impression of Change (PGIC) “Much Better” or “Very Much Better”
The percentage of participants experiencing a CNS-CTEAE (dizziness, somnolence, and paresthesia) after lasmiditan treatment was generally similar in those who had improved PGIC versus other ratings at 2 h (Fig. 1c, OSM Table 4). The percentage of those experiencing nausea was lower in those with improved PGIC at 2 h.
3.5 Efficacy Outcomes in Those With and Without CTEAEs
The likelihood of achieving efficacy outcomes at 2 h in participants who reported a CTEAE versus those who did not report the CTEAE by 48 h post-dose was assessed.
3.5.1 Pain Freedom in Those With and Without CTEAEs
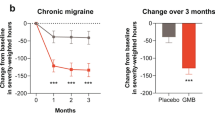
A significantly greater percentage of participants with ≥ 1 CTEAE became pain-free at 2 h compared to those with no CTEAE by 48 h post-dose for lasmiditan 100 mg (33.7% and 26.4%, respectively) and 200 mg (39.0% and 30.2%, respectively) doses. In general, lasmiditan-treated participants with ≥ 1 CTEAE, individual CNS-CTEAEs, or fatigue were numerically more likely to have pain freedom at 2 h than those without the individual CTEAEs. For nausea, the opposite association was noted (Fig. 2a, OSM Table 5).
The percentage of participants experiencing efficacy in those that did or did not experience the given CTEAE. A higher percentage of participants experiencing ≥ 1 CTEAE, dizziness, somnolence, or paresthesia achieved pain freedom than those who did not (a) No consistent differences were observed for disability freedom (b) between those with and those without a CNS-CTEAE. The percentage of participants with PGIC was greater with a CNS-CTEAE versus no CNS-CTEAE (c). *p < 0.05, **p < 0.01, ***p < 0.001 Yes versus No CTEAE. The only treatment by subgroup interaction p values < 0.1 were dizziness and pain freedom (0.061), and nausea and disability freedom (0.047). CNS central nervous system, CTEAE common treatment-emergent adverse event, L lasmiditan, PBO placebo, PGIC patient global impression of change
Lasmiditan-treated participants with onset of ≥ 1 CTEAE, dizziness, somnolence, paresthesia, and nausea occurring at or before 2 h generally became pain-free at 2 h at a higher rate than those with CTEAE onset after 2 h (Fig. 3a). The complete data set is presented in OSM Table 4.
The percentage of participants experiencing efficacy in those that experienced the given CTEAE before or after 2 h. Generally, a higher percentage of participants whose CTEAE started at or before 2 h became pain-free compared to those whose CTEAE started after 2 h (a). There were no clinically meaningful differences in disability freedom (b) or PGIC (c) in those with a CTEAE onset at or before 2 h versus after 2 h. *p < 0.05, **p < 0.01, ***p < 0.001 ≤ 2 h versus > 2 h. The only treatment by subgroup interaction p values < 0.1 were ≤ 1 CTEAE and pain freedom (0.075), ≤ 1 CTEAE and disability freedom (0.056), and dizziness and disability freedom (0.089). CTEAE common treatment-emergent adverse event, h hour, L lasmiditan, PBO placebo, PGIC patient global impression of change
3.5.2 Functional Disability in Those With and Without CTEAEs
There were no consistent differences in disability freedom at 2 h between those with versus without a CTEAE onset within 48 h with the exception of nausea (Fig. 2b, OSM Table 6). Regardless of treatment, fewer participants with nausea achieved disability freedom at 2 h compared to those without nausea. There was no consistent relationship between early or late onset of any of the CTEAEs and disability freedom at 2 h (Fig. 3b, OSM Table 6).
3.5.3 PGIC in Those With and Without CTEAEs
Generally, a numerically higher percentage of participants with a CTEAE after taking lasmiditan had improved PGIC at 2 h than those who did not experience the CTEAE (Fig. 2c, OSM Table 7). Similar to other endpoints, significantly fewer participants with nausea in all treatment groups had improved PGIC at 2 h compared to those without nausea.
There was a general pattern of a higher percentage of lasmiditan-treated participants having improved PGIC in those with onset of ≥ 1 CNS-CTEAE, dizziness, somnolence, or paresthesia occurring at or before 2 h compared to onset after 2 h (Fig. 3c, OSM Table 7).
3.6 Data Visualization
On an individual patient level, timing of a CTEAE onset was investigated relative to changes in pain to determine if the occurrence of a CTEAE consistently preceded the occurrence of pain freedom (Fig. 4 and OSM Interactive Fig. 4). OSM Interactive Fig. 4 is an interactive version of Fig. 4 that allows a user to select and visualize individual CTEAEs, dose, and pain level at the population level and individual patient level (for optimal viewing, please view OSM Interactive Fig. 4 on a laptop/desktop computer instead of a mobile device).
Data visualization demonstrating the timing of common treatment-emergent adverse event (CTEAE) onset relative to head pain intensity. In this representative image, only dizziness and pain freedom occurring with lasmiditan 200 mg is shown. An interactive version of this figure is available as OSM where pain freedom/relief and CTEAE's/dose combinations may be selected. Nested donuts: nested donut chart representing the distribution of participants who did (including onset information) and did not (including pain level at 2 h) experience the specified CTEAE. “Other” includes participants that took a second dose or rescue medication before or at 2 h. Rainbow: Time course of head pain intensity and CTEAE onset for individual participants’ panel who experienced the indicated CTEAE at or before 2 h. Missing headache intensity was imputed using the last non-missing observation. Sorting options (i.e sorting by CTEAE onset) are available in Interactive Fig. 4. All sorts use imputed pain values regardless of whether imputed value box is checked or not. Horizontal bar charts: Summary of the proportion of participants by timing of CTEAE onset relative to the time each patient first achieved pain freedom or first achieved meaningful pain relief (PR-Interactive Fig. 4 only) within 2 h. All values obtained on a continuous time scale
3.6.1 Nested Donuts
The percentage of participants without a CTEAE who experience pain freedom at 2 h was numerically greater than the percentage of participants who experience a CTEAE at any time, regardless of the specific CTEAE or dose (OSM Interactive Fig. 4, Donut Panel).
3.6.2 Horizontal Bar Charts
The relative order of onset of meaningful pain improvement/pain freedom and onset of a CTEAE was determined based on a continuous time scale. The bar charts show that CTEAE onset occurred before the time at which participants became head pain-free and generally before the time headache relief became meaningful (OSM Interactive Fig. 4, Bar Charts).
3.6.3 Rainbow
The individual patient-level data analysis of OSM Interactive Fig. 4 allows customized sorting of data. Individual participants from the “Yes” CTEAE with onset ≤ 2 h depicted in the outer donut ring were followed over time, and CTEAE onset and pain intensity status are indicated. The default sort shown, increasing pain in reverse chronological order (categorical) followed by CTEAE onset, demonstrates that, consistent with the results presented in the bar charts (continuous onset times for both parameters), CTEAE onset is generally before pain freedom regardless of CTEAE or treatment selected (OSM Interactive Fig. 4, Rainbow). By changing the sorting options, this tool can be used to gain insight into the influence of other patient level characteristics, such as baseline pain and CTEAE onset.
4 Discussion
The objective of these post hoc analyses was to explore the inter-relationship of the CTEAEs and efficacy outcomes reported (within treatment group comparisons only). We found that after lasmiditan treatment:
-
Participants who experienced CNS-CTEAEs were more likely to experience pain improvement (reduction from moderate or severe pain to pain freedom or mild pain).
-
Participants who experienced pain improvement were more likely to experience CNS-CTEAEs.
-
CTEAEs were not associated with increased migraine-related functional disability.
-
A higher percentage of participants with a CNS-CTEAE had improved PGIC at 2 h than those who did not, though this difference was not statistically significant.
We found that a higher percentage of participants who had mild or no pain at 2 h experienced a CNS-CTEAE than those with moderate or severe pain at 2 h. This association should not be interpreted as a CTEAE is required in order to achieve mild/no pain at 2 h. In fact, 50% of participants who achieved 2-h pain freedom after treating an attack with lasmiditan 200 mg reported no CTEAEs.
Participants who experienced ≥ 1 CTEAE or one of the CNS-CTEAEs (dizziness, somnolence, or paresthesia) by 48 h post-dose were numerically more likely to achieve pain freedom at 2 h compared to those who did not experience a CTEAE or the given CNS-CTEAE. It is important to note that at least 30% of participants without ≥ 1 CTEAE who received 200 mg lasmiditan still achieved 2-h pain freedom, but those who had ≥ 1 CTEAE had a significantly increased chance at pain freedom than those that did not experience ≥ 1 CTEAE.
To further explore the temporal relationship between CTEAEs and efficacy, we analyzed the timing of CTEAE onset relative to efficacy outcomes at 2 h. Participants who experienced a CTEAE at or before 2 h were more likely to achieve pain freedom at 2 h. The results from the individual patient analysis suggest that CTEAE onset usually preceded the occurrence of pain freedom.
Next, we assessed the association of CTEAEs with disability freedom and PGIC. Disability freedom at 2 h was similar in those with and without ≥ 1 CTEAE. Numerically, a higher percentage of participants with a CNS-CTEAE had improved PGIC at 2 h than those who did not. Moreover, the percentage of participants with improved PGIC was greater if the onset of the CNS-CTEAE was before or at 2 h versus after 2 h. While CNS-CTEAEs were associated with greater pain freedom, they were not associated with increased disability or attenuated PGIC at 2 h.
In each of the CTEAE versus no CTEAE analyses, nausea had an opposite association with efficacy outcomes compared to each of the CNS-CTEAEs. Specifically, the presence of nausea was associated with a lower likelihood of pain freedom, disability freedom, and improved PGIC. This may be indicative of the impact of nausea on drug absorption or the impact of nausea on participants’ ability to return to their usual daily activities and their perception of their overall condition [15]. An alternative possibility is that only the CNS-CTEAEs were associated with efficacy because they are mediated by a similar mechanism as that for efficacy.
The overall findings of CNS adverse events often being followed by pain reduction or elimination after lasmiditan dosing may have clinical implications and may be related to the central penetration of lasmiditan [1], with 5-HT1F receptors being widely expressed in the CNS [16]. 5-HT1F agonism both slows neural transmission and inhibits the release of neural transmitters such as calcitonin gene-related peptide [17,18,19] and glutamate [20]. These effects may account for efficacy but may also contribute to CNS side effects. For example, CTEAEs may be markers of rapid absorption or rapid achievement of high concentrations of drug at one or more CNS sites that lead to both CTEAEs and efficacy. The findings of a relationship between CTEAEs and pain reduction are consistent with findings reported by Goadsby et al. [8], but because onset of CTEAEs occurred before pain freedom and generally before pain relief, the hypothesis of unmasking CNS adverse events (or increased awareness of side effects once pain has lessened) seems unlikely in participants treated with lasmiditan. It seems more likely that the CNS adverse events and efficacy of lasmiditan are caused by similar effects on neurological pathways or that the CNS-adverse effects in some way contribute to efficacy, for example, by restoring homeostasis in the setting of migraine attacks caused by imbalance of excitatory-inhibitory pathways [21]. Other work has shown efficacy of lasmiditan in attacks typically considered to be “hard to treat” [22], and the present work suggests the possibility that this efficacy might be related to the central penetration and CNS effects of the drug. Further elucidation of these concepts would require the development of a 5-HT1F agonist that is not centrally penetrant. The finding that CNS-CTEAEs, generally mild to moderate, transient, and self-limited [6], may predict reduction in pain without worsening disability or PGIC may be relevant information for prescribers and for patients taking lasmiditan. For example, participants could be informed that they might or might not feel effects such as dizziness or somnolence after taking lasmiditan, and that these symptoms, if experienced, may indicate that pain improvement is likely to follow.
There were limitations to this report. These post hoc analyses should be considered exploratory without multiplicity control. Safety data were obtained from randomized clinical trials and should not be interpreted as real-world evidence. Trial designs limited exploration of many factors that could influence the results. For example, participants were instructed to treat attacks within 4 h of onset when pain was moderate or severe, which limited the ability to assess the impact of delayed dosing or baseline pain intensity on efficacy and CTEAE-associations. Also, data regarding peripheral or central sensitization associated with the attack were not obtained. However, a previously disclosed post-hoc analysis demonstrated that 100 and 200 mg lasmiditan was effective for achieving 2-h pain freedom in participants with severe head pain, coexistent nausea at the time of dosing, or delayed treatment (by 2 or more h from onset) [22]. Another limitation is the unknown variability of lasmiditan pharmacokinetics. The small numbers of participants experiencing paresthesia, nausea, and fatigue limited conclusions, especially for lower doses and placebo, and also limited assessment of associations across multiple attacks. In addition, pain intensity, disability, and PGIC were collected at discrete time points, while TEAEs were collected on a continuous time scale, limiting the exploration of outcomes at the exact time of CTEAE occurrence. Patient-reported time-to-pain freedom and time-to-meaningful pain relief, which were collected on a continuous timeline, partially addresses the limitation of comparing a categorical result variable with a continuous variable. However, this collection method is potentially limited by patient recall. Interpretation is further limited by missing or incomplete data.
5 Conclusion
Overall, while we observed a greater likelihood of experiencing a CNS-CTEAE with pain freedom than with moderate/severe pain at 2 h, more than 50% of participants with pain freedom did not have a CNS-CTEAE. While the absence of a CNS-CTEAE did not equate to lack of efficacy, the incidence of pain freedom was greater for those who experienced a CNS-CTEAE. The occurrence of a CNS-CTEAE was not associated with a lower likelihood of achieving disability freedom or improved PGIC. The results found in this study are relevant to and may impact migraine treatment decisions in the clinic.
References
Clemow DB, Johnson KW, Hochstetler HM, et al. Lasmiditan mechanism of action—review of a selective 5-HT1F agonist. J Headache Pain. 2020;21(1):71.
Ashina M, Vasudeva R, Jin L, et al. Onset of efficacy following oral treatment with lasmiditan for the acute treatment of migraine: integrated results from 2 randomized double-blind placebo-controlled phase 3 clinical studies. Headache. 2019;59(10):1788–801.
Doty EG, Krege JH, Jin L, et al. Sustained responses to lasmiditan: results from post-hoc analyses of two phase 3 randomized clinical trials for acute treatment of migraine. Cephalalgia. 2019;39(12):1569–76.
Goadsby PJ, Wietecha LA, Dennehy EB, et al. Phase 3 randomized, placebo-controlled, double-blind study of lasmiditan for acute treatment of migraine. Brain. 2019;142(7):1894–904.
Smith T, Krege JH, Rathmann SS, et al. Improvement in function after lasmiditan treatment: Post hoc analysis of data from phase 3 studies. Neurol Ther. 2020;9(2):459–71.
Krege JH, Rizzoli PB, Liffick E, et al. Safety findings from Phase 3 lasmiditan studies for acute treatment of migraine: Results from SAMURAI and SPARTAN. Cephalalgia. 2019;39(8):957–66.
Clemow DB, Hochstetler HM, Dong Y, et al. Effect of a change in lasmiditan dose on efficacy and safety in patients with migraine. Postgrad Med. 2021;133(4):449–59.
Goadsby PJ, Dodick DW, Almas M, et al. Treatment-emergent CNS symptoms following triptan therapy are part of the attack. Cephalalgia. 2007;27(3):254–62.
Tepper SJ, Krege JH, Lombard L, et al. Characterization of dizziness after lasmiditan usage: findings from the SAMURAI and SPARTAN acute migraine treatment randomized trials. Headache. 2019;59(7):1052–62.
Ashina M, Reuter U, Smith T, et al. Randomized, controlled trial of lasmiditan over four migraine attacks: FINDINGS from the CENTURION study. Cephalalgia. 2021;41(3):294–304.
Brandes JL, Klise S, Krege JH, et al. Interim results of a prospective, randomized, open-label, phase 3 study of the long-term safety and efficacy of lasmiditan for acute treatment of migraine (the GLADIATOR study). Cephalalgia. 2019;39(11):1343–57.
Kuca B, Silberstein SD, Wietecha L, et al. Lasmiditan is an effective acute treatment for migraine: a phase 3 randomized study. Neurology. 2018;91(24):e2222–32.
Sakai F, Takeshima T, Homma G, et al. Phase 2 randomized placebo-controlled study of lasmiditan for the acute treatment of migraine in Japanese patients. Headache. 2021;61(5):755–65.
Tfelt-Hansen P, Pascual J, Ramadan N, et al. Guidelines for controlled trials of drugs in migraine: third edition. A guide for investigators. Cephalalgia. 2012;32(1):6–38.
Lainez MJ, Garcia-Casado A, Gascon F. Optimal management of severe nausea and vomiting in migraine: improving patient outcomes. Patient Relat Outcome Meas. 2013;11(4):61–73.
Vila-Pueyo M. Targeted 5-HT1F therapies for migraine. Neurotherapeutics. 2018;15(2):291–303.
Amrutkar DV, Ploug KB, Hay-Schmidt A, et al. mRNA expression of 5-hydroxytryptamine 1B, 1D, and 1F receptors and their role in controlling the release of calcitonin gene-related peptide in the rat trigeminovascular system. Pain. 2012;153(4):830–8.
Gonzalez-Hernandez A, Manrique-Maldonado G, Lozano-Cuenca J, et al. The 5-HT(1) receptors inhibiting the rat vasodepressor sensory CGRPergic outflow: further involvement of 5-HT(1F), but not 5-HT(1A) or 5-HT(1D), subtypes. Eur J Pharmacol. 2011;659(2–3):233–43.
Labastida-Ramirez A, Rubio-Beltran E, Haanes KA, et al. Lasmiditan inhibits calcitonin gene-related peptide release in the rodent trigeminovascular system. Pain. 2020;161(5):1092–9.
Ma QP. Co-localization of 5-HT(1B/1D/1F) receptors and glutamate in trigeminal ganglia in rats. NeuroReport. 2001;12(8):1589–91.
Vecchia D, Pietrobon D. Migraine: a disorder of brain excitatory-inhibitory balance? Trends Neurosci. 2012;35(8):507–20.
Tepper SJ, Vasudeva R, Krege JH, et al. Evaluation of 2-hour post-dose efficacy of lasmiditan for the acute treatment of difficult-to-treat migraine attacks. Headache. 2020;60(8):1601–15.
Acknowledgements
The authors thank Zachary Skrivanek and Pratibha KS for developing the interactive data visualization (employees of Eli Lilly and Company).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study and its open access publication was sponsored/funded/supported by Eli Lilly and Company.
Conflicts of interests
RBL receives research support from the NIH, FDA, as well as the National Headache Foundation and the Marx Foundation. He also receives research support from Allergan/Abbvie, Amgen, Eli Lilly, and Electrocore. He receives personal fees as a consultant or advisor from Allergan/Abbvie, Amgen, Biohaven Holdings, Dr. Reddy's, GlaxoSmithKline, Grifols, Impel NeuroPharma, Eli Lilly, Lundbeck, Merck, Novartis, and Teva Pharmaceuticals. He holds stock or options in Biohaven Holdings, CtrlM Health and Manistee. EGD, PMH, JHK, MK, AMH, and YD are employees and minor stockholders of Eli Lilly and Company.
Ethics approval
The studies were carried out in accordance with the International Conference on Harmonisation Good Clinical Practice guidelines, and local regulatory requirements. The protocols were approved by an institutional review board or independent ethics committee at each study site.
Consent to participate
Written informed consent for study participation was obtained from each patient prior to the start of the study.
Consent for publication
Not applicable.
Code availability
Not applicable.
Authors’ contributions
AMH, EGD, JHK, PMH, and RBL, were involved in study conception and design. MK acquired data. EGD, PMH, and YD performed data analysis. EGD, JHK, MK, PMH, RBL, and YD, provided data interpretation. AMH, EGD, JHK, MK, PMH, RBL, and YD, were involved in drafting/revising the article. AMH, EGD, JHK, MK, PMH, RBL, and YD, have read and provided approval of the final submitted version of the manuscript and agree to be accountable for the presented work.
Availability of data and material
Lilly provides access to all individual participant data collected during the trial, after anonymization, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the US and EU and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, and blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.
Supplementary Information
Below are the links to the online supplementary materials.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Doty, E.G., Hauck, P.M., Krege, J.H. et al. The Association Between the Occurrence of Common Treatment-Emergent Adverse Events and Efficacy Outcomes After Lasmiditan Treatment of a Single Migraine Attack: Secondary Analyses from Four Pooled Randomized Clinical Trials. CNS Drugs 36, 771–783 (2022). https://doi.org/10.1007/s40263-022-00928-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-022-00928-y