Abstract
Introduction
In evaluating therapies for migraine prevention, emphasis is placed on frequency and less attention is paid to duration or severity. Total pain burden (TPB) combines frequency, duration, and severity of migraine headache, and has the potential to further characterize the benefit of preventive treatment using a single composite measure. TPB was previously used to characterize response to galcanezumab (GMB) in patients with migraine. In this post hoc analysis we assessed the impact of GMB in lowering TPB in patients who had previously not benefited from two to four categories of migraine preventive medication.
Methods
CONQUER trial patients (N = 462), 18–75 years old who had previously not benefited from two to four categories of migraine preventive medication, were randomized (1:1) to monthly placebo or GMB 120 mg with 240 mg loading dose. For each patient, monthly TPB in severity-weighted hours was calculated by multiplying migraine headache duration (hours) by maximum severity for each migraine headache day, then summing these daily scores over the month for the monthly score. Changes from baseline in monthly TPB across months 1–3 were analyzed. Spearman correlations between TPB and scores on the Migraine-Specific Quality-of-Life Questionnaire (MSQ) total and Migraine Disability Assessment Scale (MIDAS) were assessed at baseline.
Results
Mean (SD) baseline monthly TPB was 192.1 (158.3) and 188.2 (197.4) severity-weighted hours for GMB-treated and placebo-treated patients, respectively. Across the 3-month double-blind period, GMB-treated patients experienced significantly greater mean reductions from baseline in monthly TPB compared with placebo-treated patients, both for mean change (GMB − 82.7, placebo − 15.8, p < 0.001) and percentage change (GMB − 38.6%, placebo 9.4%, p < 0.001). Furthermore, baseline TPB correlated with MSQ score (r = − 0.39) and MIDAS score (r = 0.40), suggesting good association of TPB with functional and disability outcomes.
Conclusion
GMB reduced mean TPB in patients who had previously not benefited from two to four categories of migraine preventive medication.
Trial Registration
NCT03559257.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Total pain burden (TPB; a measure combining migraine headache frequency, duration, and severity) was previously used to characterize responses to galcanezumab in patients with episodic migraine or chronic migraine. Greater reduction in TPB was seen in patients with episodic migraine or chronic migraine treated with galcanezumab relative to placebo. |
In this post hoc analysis, we examined the effect of galcanezumab on TPB among patients enrolled in the CONQUER trial who had previously not benefited from two to four categories of migraine preventive medication. |
What was learned from the study? |
Galcanezumab reduced mean TPB in patients who had previously not benefited from two to four categories of migraine preventive medication. |
TPB provides a mechanism for assessing and integrating the impact of treatment on disease burden that otherwise remains isolated. |
The impact of galcanezumab treatment in lowering TPB was not just due to its effect on lowering the frequency of migraine headache days, as it also reduced the duration and severity of a migraine headache day. |
Digital Features
This article is published with digital features, including a video, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.20089112
Introduction
Migraine is a neurological disease characterized by moderate to severe headaches, accompanied by nausea and/or vomiting, or photophobia and phonophobia that carries a significant health burden [1, 2]. In the USA migraine and severe headache prevalence is 15.9%, while in Europe migraine prevalence is 11.4% [3, 4]. Migraine can be characterized as episodic or chronic, with chronic migraine defined as headaches occurring on at least 15 days per month for 3 months where at least 8 days per month met criteria for migraine [1]. Treatment guidelines for migraine include the following goals of preventive treatment: reduce attack frequency, severity, and duration; improve responsiveness to treatment of acute attacks; and improve function and reduce disability [2, 5].
Optimizing migraine preventive treatment remains challenging. Current guidelines of the International Headache Society for controlled trials of preventive treatment of migraine in adults recommend the primary endpoints: change from baseline in migraine days per unit time and change from baseline in moderate/severe headache days or 50% responder rate for the reduction of migraine days for episodic migraine [6], and either change in migraine days; change in moderate to severe headache days; or responder rate for chronic migraine [7]. In patients with migraine, the benefit provided by preventive treatment can span from no benefit in any component of migraine pain (frequency, duration, and severity) to benefits in all three components. In evaluating new and existing therapies for migraine, emphasis is generally placed on migraine frequency, with less attention paid to migraine duration and severity which may be inadequate in assessing the overall benefit of treatment. Evaluating the combined effects of a therapy on frequency, duration, and severity, under a single composite measure, may facilitate more patient-centric discussions around treatment expectations when considering options for migraine treatment. Total pain burden (TPB), a single composite measure assessing the frequency, duration, and severity of migraine [8], may provide a more robust evaluation of the potential benefits of a treatment in reducing the overall pain experience.
Galcanezumab (GMB) is a humanized IgG4 monoclonal antibody that binds calcitonin gene-related peptide (CGRP) and prevents its biological activity without blocking the CGRP receptor [9]. The efficacy of GMB as a preventive treatment for migraine has been reported in three randomized, double-blind, placebo-controlled phase 3 studies in patients with episodic (EVOLVE-1 and EVOLVE-2) and chronic (REGAIN) migraine [10,11,12]. Treatment with GMB has been shown to lower TPB in patients with episodic and chronic migraine using data from the EVOLVE-1/2 and REGAIN trials [8].
The CONQUER trial assessed the safety and efficacy of GMB compared to placebo in patients who had previously not benefited from two to four categories of migraine preventive medication [13]. It was shown that patients treated with GMB had fewer migraine headache days per month than patients in the placebo group. The GMB group had 4.1 (2.9 for episodic and 6.0 for chronic) fewer migraine headache days per month relative to their baseline, whereas the placebo group had 1.0 (0.3 for episodic and 2.2 for chronic) fewer migraine headache days per month relative to their baseline. However, it is not clear whether GMB lowered TPB in the population of patients seen in the CONQUER trial. The primary objective of this post hoc analysis was to assess the impact of GMB in lowering TPB in the study population of the CONQUER trial, evaluate the advantages of TPB over assessing individual components alone, and correlate this measure with patient-reported quality of life outcomes.
Methods
Study Design
CONQUER (NCT03559257) is a phase 3, multicenter, randomized, double-blind, parallel, placebo-controlled study to assess the efficacy and safety of GMB 120 mg per month (mg/month) in a treatment-resistant patient population with episodic or chronic migraine. Treatment resistance was defined as two to four categories of migraine preventive medication had failed in the last 10 years as a result of inadequate efficacy, reasons of safety and tolerability, or both. Eligible patients were randomized in 1:1 to GMB 120 mg/month (N = 232) or placebo (N = 230). Patients randomized to GMB received a loading dose of 240 mg, administered as two injections of 120 mg each at the first visit. Patients completed an electronic daily diary, answering questions about the occurrence of headaches, headache duration and features, severity of headache, and whether any acute headache medication was taken. Patients could continue to take their allowed acute medications for migraine during the treatment phase. Further details on the study design can be found in the primary manuscript from this trial [13].
Patient Disposition
Patients were 18–75 years old at enrollment, with a diagnosis of migraine as defined by the International Classification of Headache Disorders-3 (ICHD-3) guidelines [1], with a history of migraine of at least 1 year prior to enrollment, and migraine onset prior to age 50. Patients had a history of at least 4 migraine headache days and at least 1 headache-free day per month, on average, in the past 3 months; had documented two to four categories of migraine preventive medication had failed in the past 10 years. Further information on patient eligibility can be found in the clinical trial primary manuscript [13]. In this post hoc analysis, data are presented for patients from the intent-to-treat (ITT) cohort with episodic or chronic migraine, and the overall population (episodic and chronic combined).
Outcomes
For each patient, the daily pain burden was calculated by multiplying the number of hours of migraine by the maximum daily pain severity score of migraine (0 = none, 1 = mild, 2 = moderate, 3 = severe). The monthly TPB was calculated by adding the daily pain burden over the entire month (adjusted to a 30-day period). Days during the month with no migraine contribute a daily pain burden of 0. This TPB essentially combines the number of migraine headache days seen during a month, the average duration in hours per migraine headache day in that month, and the average pain severity of migraine headache day into one composite measure to provide a holistic measure of pain experienced by the patient during the month.
Two patient-reported outcomes (PROs) were also included in this analysis: the Migraine-Specific Quality-of-Life Questionnaire (MSQ version 2.1 total score; monthly) and the Migraine Disability Assessment Scale (MIDAS, at baseline and at month 3). The MSQ is a 14-item questionnaire addressing the physical and emotional effect of migraine on functioning over a 4-week recall period [14]. The MIDAS quantifies headache-related disability over a 3-month recall period [15].
Statistical Methods
Mean and Percentage Change from Baseline in Total Pain Burden
Mean change from baseline in monthly pain burden was compared between the GMB and placebo groups using a mixed model for repeated measures (MMRM) analysis. The following terms were included in the model as fixed effects and/or covariates: baseline TPB, treatment, month, treatment × month, baseline × month, and pooled country. A similar MMRM model was used to analyze the percentage change from baseline in monthly TPB between the two treatment groups as well. The use of the numeric scores 0, 1, 2, and 3 to indicate none, mild, moderate, and severe categories, respectively, of pain severity enforces the following relation between mild migraine severity and other higher categories of migraine severity: each hour of moderate migraine is equivalent to 2 h of mild migraine and each hour of severe migraine is equivalent to 3 h of mild migraine. This degree of association between severity of migraine categories can be considered arbitrary and unvalidated. To test the impact of the choice of the severity scores on the treatment effect, we conducted the following sensitivity analyses on the mean change from baseline analyses assuming two other severity score categories: one assuming the square root of the original severity category scores (0 = none, 1 = mild, 1.414 = moderate, 1.732 = severe) and the other analyses assuming the square of the original severity category scores (0 = none, 1 = mild, 4 = moderate, 9 = severe). These two additional sensitivity analyses either down-weight or up-weight the degree of association between mild and higher severity categories.
Relative Contribution of Each Component
Semi-partial correlation coefficients between TPB and the three individual components frequency of migraine headache days, average duration of migraine per day, and average pain severity were calculated using a linear regression model on log-transformed variables. The semi-partial correlation coefficients provide the percentage of variability additionally explained by each component on the TPB measure after adjusting for the other two components. To understand whether the treatment provides additional benefit in lowering TPB that cannot be explained by the lowering in frequency of migraine headache days, the MMRM model was repeated by analyzing the mean change from baseline in TPB after including an additional time-varying covariate of the change from baseline in the number of monthly migraine headache days. Additionally, each of the three components (monthly number of migraine headache days, monthly duration in hours per migraine headache day, and average severity of migraine headache day) was analyzed individually using similar MMRM models to assess the impact of treatment separately on each component.
Construct Validity
The associations between TPB and quality of life (MSQ) and disability (MIDAS) measures were analyzed using Spearman’s correlation coefficient to explore construct validity of the TPB measure.
General Considerations
Data were summarized using appropriate summary statistics such as mean, standard deviation and/or median and quartiles for numeric variables and frequency and percentages for categorical variables. Missing data was very minimal and therefore no specific methods such as multiple imputation were used to analyze the data. For all MMRM models, the correlation among repeated measures on the same patient was accounted for by assuming an unstructured covariance matrix on the residuals, and patients were included in the analysis if they had valid values at baseline and at least one post-baseline measurement. Kenward–Roger approximation was used to estimate the denominator degrees of freedom. All statistical tests conducted must be considered post hoc in nature assuming a two-sided significance level of 5%. No adjustments for multiple testing were made and all results should be considered exploratory in nature.
Ethics Statement
Appropriate institutional review boards reviewed and approved the study, which was conducted according to the Declaration of Helsinki, and all subjects provided informed consent to participate in the study.
Results
Patient Demographics and Baseline Disease Characteristics
A total of 462 patients in the ITT population (overall population) were considered for this post hoc analysis of which 269 experienced episodic migraine and 193 experienced chronic migraine during the baseline period. Among them, 11 (2.4%) patients had discontinued from the double-blind treatment period (4 in placebo group, 7 from the galcanezumab group). Four patients had insufficient eDiary data (2 in placebo and 2 in galcanezumab group) and did not contribute to the primary endpoint analysis for the study and for this post hoc analysis (n = 458) [13].
The patient populations were similar in terms of age and gender (Table 1). Patients with chronic migraine had a greater number of mean migraine headache days per month, a greater MIDAS total score, a lower MSQ total score, and a greater total monthly pain severity-weighted duration (hours) compared to patients with episodic migraine. Within each patient population demographics and disease characteristics at baseline were balanced between the placebo and GMB 120 groups.
Total Pain Burden
Mean Change from Baseline
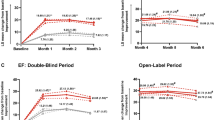
GMB 120 mg significantly lowered TPB compared with placebo in the episodic (Fig. 1a) and chronic (Fig. 1b) subpopulations. The mean difference relative to placebo in overall mean change from baseline was − 49.9 (95% CI − 64.7, − 35.1) and − 89.4 (95% CI − 128.8, − 50.1) for episodic and chronic migraine populations, respectively. GMB significantly lowered mean monthly TPB relative to placebo in the overall population. LS mean monthly change from baseline averaged across all 3 months was − 82.7 severity-weighted hours in the GMB 120 mg group compared to − 15.8 severity-weighted hours in the placebo group (mean difference = − 66.8; 95% CI − 85.5, − 48.2; p < 0.001, Fig. 1c). Further, in the overall population as well as the episodic and chronic subpopulations, significantly greater reductions in monthly TPB relative to placebo were observed at each individual month (all p < 0.001) (Fig. 1).
Effect of galcanezumab on total pain burden. LS mean change (SE) in severity-weighted hours from baseline at each month and overall across all months in patients with episodic migraine (a), chronic migraine (b), and in the overall population (c). ***p < 0.001 vs. placebo. Only patients with baseline and at least one post-baseline measurement were included in this analysis. Sample sizes are episodic migraine: placebo n = 132, GMB 120 mg n = 137; chronic migraine: placebo n = 96, GMB 120 mg n = 93; and overall: placebo n = 228, GMB 120 mg n = 230. CI confidence interval, GMB galcanezumab, LS least squares, PBO placebo, SE standard error
A sensitivity analysis was also conducted to address the impact of using severity scores of 0 for none, 1 for mild, 2 for moderate, and 3 for severity in the calculation of pain burden. This was done in two different ways as explained in the statistical methods, one using the square root of these scores in computation of TPB and the other using the square of these scores in computation of TPB. The mean change from baseline in TPB was still significantly lower relative to placebo in both these analyses. The mean difference relative to placebo in overall mean change from baseline was − 42.1 (95% CI − 53.9, − 30.4; p < 0.001) when using the square root of severity scores and − 174.9 (95% CI − 225.0, − 124.9; p < 0.001) when using the square of severity scores.
Percentage Change from Baseline
GMB 120 mg significantly lowered TPB compared with placebo in the episodic (Fig. 2a) and chronic (Fig. 2b) subpopulations. The mean difference relative to placebo in overall percentage change from baseline was − 53.1% (95% CI − 75.3%, − 31.0%, p < 0.001) and − 40.4% (95% CI − 53.4%, − 27.4%, p < 0.001) for the episodic and chronic migraine subpopulations, respectively. In the overall population, the GMB group showed a greater reduction in mean percentage change from baseline in TPB compared with placebo at each individual month and overall across all 3 months in the double-blind period. The LS mean (SE) percentage change from baseline in TPB averaged across all 3 months was − 38.6% in the GMB 120 mg group compared to 9.4% in the placebo group (mean difference = − 48.1%; 95% CI − 62.3% to − 33.9%; p < 0.001, Fig. 2c). For each patient in the placebo and GMB 120 mg groups, the TPB as a percentage of their baseline (TPB value at each month/baseline TPB × 100) at each month and the change over time from one month to another in the double-blind period are shown in Video 1 in the Supplementary Material.
Effect of galcanezumab on total pain burden. LS mean percentage change (SE) in total pain burden/severity-weighted hours from baseline at each month and overall across all months in patients with episodic migraine (a), chronic migraine (b), and in the overall population (c). ***p < 0.001 vs. placebo. Only patients with baseline and at least one post-baseline measurements were included in this analysis. Sample sizes are episodic migraine: placebo n = 132, GMB 120 mg n = 137; chronic migraine: placebo n = 96, GMB 120 mg n = 93; and overall: placebo n = 228, GMB 120 mg n = 230. CI confidence interval, GMB galcanezumab, LS least squares, PBO placebo, SE standard error
Video 1: The change in monthly TPB as a percent of baseline (left: placebo; right: galcanezumab 120 mg). Individual patients are rank ordered by percent of baseline TPB value at month 3 (solid fill = patients with episodic migraine, hollow fill = patients with chronic migraine). Patients with no values at month 3 due to missing data are placed towards the right side of the x-axis. Solid purple line = the mean percent of baseline in TPB within each treatment group at any point in time. Centre bar plot= observed/raw mean change in TPB from baseline to the end of each month for each treatment group (placebo=grey, galcanezumab 120 mg=red). Top: timeline bar tracks the month of treatment being shown. (MP4 14495 KB)
Contribution of Components to Total Pain Burden
Frequency of migraine headache days and its duration on a given migraine headache day contributed the greatest unique proportion of variability to the baseline TPB after adjusting for frequency of migraine headache days and maximum pain severity (Table 2).
Change from Baseline of Individual Components
The LS mean reductions from baseline for the individual components of migraine were significantly greater for patients treated with GMB in the overall population, and episodic and migraine subpopulations. In the overall population, the change from baseline in the number of monthly migraine headache days (− 1.02 for placebo vs. − 4.14 for GMB [13]), the change from baseline in the number of hours per migraine headache day (0.11 for placebo vs. − 0.83 for GMB), and the change from baseline in the severity of remaining migraine headache days (− 0.09 for placebo vs. − 0.25 for GMB) were all significantly different in favor of the GMB group. Similar improvements for the GMB group were also observed in episodic and chronic migraine subpopulations (Table 3).
Sensitivity Analysis
An additional sensitivity analysis was conducted to determine whether the effect of GMB treatment in lowering TPB would remain even after controlling for the reduction observed in migraine headache day frequency. This analysis demonstrated that for patients with episodic (Fig. 3a) and chronic migraine (Fig. 3b), as well as in the overall population (Fig. 3c), the reduction in TPB was still greater in patients treated with GMB compared to those treated with placebo even once migraine day reductions were accounted for. The mean reduction from baseline in TPB was greater in patients treated with GMB compared to placebo in patients with episodic migraine; mean difference (95% CI) in change from baseline was − 15.5 (95% CI − 26.4, − 4.6; p = 0.005), − 24.6 (95% CI − 55.5, 6.4; p = 0.12), and − 20.0 (95% CI − 34.8, − 5.15; p = 0.008) for the episodic, chronic, and overall populations, respectively (Fig. 3a–c).
Effect of galcanezumab on total pain burden following sensitivity analysis. LS mean change in severity-weighted hours from baseline after adjusting for change from baseline in monthly migraine headache days at each month and overall across all months in patients with episodic migraine (a), chronic migraine (b), and in the overall population (c). *p < 0.05 vs. placebo, **p < 0.01 vs. placebo. Only patients with baseline and at least one post-baseline measurements were included in this analysis. Sample sizes are episodic migraine: placebo n = 132, GMB 120 mg n = 137; chronic migraine placebo n = 96, GMB 120 mg n = 93; and overall: placebo n = 228, GMB 120 mg n = 230. CI confidence interval, GMB galcanezumab, LS least squares, PBO placebo
Total Pain Burden Correlations to MSQ and MIDAS
The MSQ total score and MIDAS scores at baseline were associated to TPB in the episodic (r = − 0.28 and r = 0.36, respectively) and chronic migraine populations (r = − 0.40 and r = 0.27, respectively), as well as in the overall population (r = − 0.39 and r = 0.40, respectively).
Discussion
Preventive migraine clinical trials have traditionally focussed on evaluating the impact of treatment on frequency of migraine headache days [13, 16]. However, focussing solely on frequency ignores the potential benefit of treatment on other facets such as duration and severity, and may limit the full potential of managing care. One patient may be more burdened by the number of days of migraine they experience while another might be more burdened by the duration or severity of pain on any given day. Ideally, individual patient treatment decisions consider frequency, duration, and severity together given their combined clinical relevance relative to frequency alone [17, 18]. Herein, we analyzed the impact of GMB in lowering TPB and tried to answer whether TPB is better than evaluating individual components of treatment effect.
It has previously been shown that GMB lowered TPB relative to placebo among patients with episodic and chronic migraine [8]. Here, we showed that GMB lowered TPB in patients with episodic and chronic migraine for whom two to four categories of migraine preventive medication had failed, indicating that this finding is consistent across patient populations in different GMB trials.
The results presented here also demonstrate that TPB is not just a surrogate measure for the frequency of migraine but a composite outcome with significant contributions from each individual component. This suggests that the overall pain experienced by patients at baseline comes not just from the number of days of migraine but a major facet of the pain burden measure as it is defined also comes from the number of hours of migraine experienced on any given migraine headache day and the maximum severity of migraine. Each component of the composite represents unique incremental burden experienced with migraine pain. TPB provides a mechanism for assessing and integrating the impact of treatment on disease burden that otherwise remains isolated. Further, through robust analyses, we show that the impact of treatment with GMB in lowering TPB was not just due to its effect on lowering the frequency of migraine headache days as it also reduced the duration and severity of a migraine headache day. TPB was also positively correlated with PROs MSQ and MIDAS, supporting adequate construct validity of this measure and suggesting TPB may be meaningful to the patient.
Strengths and Limitations
The results from this study provide additional evidence to limited but important current literature on TPB in migraine. The data for these analyses come from a large, prospective, randomized double-blind placebo-controlled clinical trial which provides greater confidence in the treatment effect estimates. However, these analyses should be considered post hoc in nature and results should be interpreted with caution. Maximum severity of migraine was recorded as opposed to more granular measurements of severity of migraine during the day. Another limitation of the analyses presented here could be the 4-point scale used to measure severity of migraine which may be less sensitive to detecting changes in pain within a patient than an 11 (0–10) point scale. Also, in this analysis, the calculation of TPB assumes a subjective score for the severity of pain category: 0 = no pain, 1 = mild pain, 2 = moderate pain, 3 = severe pain. However, through appropriate sensitivity analyses we have shown that the impact of GMB in lowering TPB is robust to changes in how severity categories are scored. Finally, although TPB was also positively correlated with PROs MSQ and MIDAS, future efforts should explore defining thresholds of TPB that represent a meaningful change within-patient change.
Conclusion
Treatment with galcanezumab 120 mg once-monthly provides a greater reduction in TPB relative to placebo among patients with episodic and chronic migraine for whom two to four categories of migraine preventive medication had failed. It can play a central role in assessing the potential benefit of a preventive treatment for patients with migraine. The results of this assessment are consistent with the main findings of the previous migraine efficacy studies relating to galcanezumab.
References
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211.
Ailani J, Burch RC, Robbins MS, Board of Directors of the American Headache S. The American Headache Society Consensus Statement: Update on integrating new migraine treatments into clinical practice. Headache. 2021;61(7):1021–39.
Burch R, Rizzoli P, Loder E. The prevalence and impact of migraine and severe headache in the United States: updated age, sex, and socioeconomic-specific estimates from government health surveys. Headache. 2021;61(1):60–8.
Woldeamanuel YW, Cowan RP. Migraine affects 1 in 10 people worldwide featuring recent rise: a systematic review and meta-analysis of community-based studies involving 6 million participants. J Neurol Sci. 2017;372:307–15.
Silberstein S, Holland S, Freitag F, Dodick D, Argoff C, Ashman E. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78(17):1337–45.
Diener H-C, Tassorelli C, Dodick DW, et al. Guidelines of the International Headache Society for controlled trials of preventive treatment of migraine attacks in episodic migraine in adults. Cephalalgia. 2020;40(10):1026–44.
Tassorelli C, Diener H-C, Dodick DW, et al. Guidelines of the International Headache Society for controlled trials of preventive treatment of chronic migraine in adults. Cephalalgia. 2018;38(5):815–32.
Ailani J, Andrews JS, Rettiganti M, Nicholson RA. Impact of galcanezumab on total pain burden: findings from phase 3 randomized, double-blind, placebo-controlled studies in patients with episodic or chronic migraine (EVOLVE-1, EVOLVE-2, and REGAIN trials). J Headache Pain. 2020;21(1):123.
EMGALITY. EMGALITY package insert. 2019.
Stauffer VL, Dodick DW, Zhang Q, Carter JN, Ailani J, Conley RR. Evaluation of galcanezumab for the prevention of episodic migraine: the EVOLVE-1 randomized clinical trial. JAMA Neurol. 2018;75(9):1080–8.
Skljarevski V, Matharu M, Millen BA, Ossipov MH, Kim BK, Yang JY. Efficacy and safety of galcanezumab for the prevention of episodic migraine: results of the EVOLVE-2 phase 3 randomized controlled clinical trial. Cephalalgia. 2018;38(8):1442–54.
Detke HC, Goadsby PJ, Wang S, Friedman DI, Selzler KJ, Aurora SK. Galcanezumab in chronic migraine: the randomized, double-blind, placebo-controlled REGAIN study. Neurology. 2018;91(24):e2211–21.
Mulleners WM, Kim BK, Láinez MJA, et al. Safety and efficacy of galcanezumab in patients for whom previous migraine preventive medication from two to four categories had failed (CONQUER): a multicentre, randomised, double-blind, placebo-controlled, phase 3b trial. Lancet Neurol. 2020;19(10):814–25.
Jhingran P, Osterhaus JT, Miller DW, Lee JT, Kirchdoerfer L. Development and validation of the Migraine-Specific Quality of Life Questionnaire. Headache. 1998;38(4):295–302.
Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology. 2001;56(6 Suppl 1):S20–8.
Tfelt-Hansen P, Block G, Dahlöf C, et al. Guidelines for controlled trials of drugs in migraine: second edition. Cephalalgia. 2000;20(9):765–86.
Lake AE, Saper JR. Chronic headache: new advances in treatment strategies. Neurology. 2002;59(5 suppl 2):S8–13.
McCrory DC, Gray RN, Tfelt-Hansen P, Steiner TJ, Taylor FR. Methodological issues in systematic reviews of headache trials: adapting historical diagnostic classifications and outcome measures to present-day standards. Headache. 2005;45(5):459–65.
Acknowledgements
The authors thank all the study participants, site investigators, and personnel involved in the CONQUER study. The authors thank Robert A Nicholson for medical review of this manuscript (employee of Eli Lilly and Company).
Funding
Sponsorship for this study and all associated publication costs, including the journal’s Rapid Service and Open Access Fees were funded by Eli Lilly and Company.
Medical Writing and Editorial Assistance
We thank Angela O’Sullivan and Sinead Ryan (both employees of Eli Lilly and Company) for their contribution to the writing and editing of this manuscript.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Study concept and design: Jeffrey Scott Andrews, Mallikarjuna Rettiganti; Analysis and interpretation of data: Mallikarjuna Rettiganti, Jeffrey Scott Andrews; Drafting of the manuscript: Mallikarjuna Rettiganti; Manuscript revision for intellectual content: Jessica Ailani, Jeffrey Scott Andrews, Richard Wenzel, Antje Tockhorn-Heidenreich, Mallikarjuna Rettiganti; Final approval of the completed manuscript: Jessica Ailani, Jeffrey Scott Andrews, Antje Tockhorn-Heidenreich, Richard Wenzel, Mallikarjuna Rettiganti.
Prior Presentation
The results have previously been presented at the following congresses: the European Academy of Neurology—7th Congress 2021, June 19–22, 2021, virtual; American Neurological Association—146th Annual Meeting, October 17–19, 2021, virtual; and PAIN Week 2021, September 7–11, 2021, Las Vegas, USA.
Disclosures
Antje Tockhorn-Heidenreich, Richard Wenzel, and Mallikarjuna Rettiganti are employees and stockholders of Eli Lilly and Company. Jessica Ailani reports honoraria for independent consulting from Amgen, Abbvie, Biohaven, BioDelivery Scientific International, Eli Lilly and Company, Lundbeck, Teva, Impel, Satsuma, Theranica, Axsome, Neso, GlaxoSmithKline, Aeon, Medscape, Neurolief; ownership of Stocks CtrlM; Speakers Bureau/honoraria for promotional speaking from Allergan/Abbvie, Amgen, Biohaven, Eli Lilly and Company, Lundbeck, Teva; Editorial services/Honoraria from Current Pain and Headache Reports, Section editor, Unusual Headache Syndromes, NeurologyLive, SELF (medical reviewer); and clinical Trial Grants (Fees to Institution) from American Migraine Foundation, Allergan, Biohaven, Eli Lilly and Company, Satsuma, and Zosano. Jeffrey Scott Andrews is an employee and stockholder of Takeda Pharmaceuticals, Limited, and was an employee of Eli Lilly and Company during the conduct of this study.
Compliance with Ethics Guidelines
Appropriate institutional review boards reviewed and approved the study, which was conducted according to the Declaration of Helsinki, and all subjects provided informed consent to participate in the study.
Data Availability
Lilly provides access to all individual participant data collected during the trial, after anonymization, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the USA and EU and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ailani, J., Andrews, J.S., Tockhorn-Heidenreich, A. et al. Effect of Galcanezumab on Total Pain Burden in Patients Who Had Previously Not Benefited from Migraine Preventive Medication (CONQUER Trial): A Post Hoc Analysis. Adv Ther 39, 4544–4555 (2022). https://doi.org/10.1007/s12325-022-02233-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02233-y