Abstract
Background
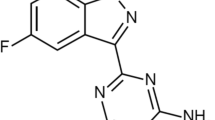
Vericiguat, a direct stimulator of soluble guanylate cyclase, has been developed as a first-in-class therapy for symptomatic chronic heart failure (HF) and ejection fraction < 45%.
Methods
Safety, pharmacodynamic (PD), and pharmacokinetic (PK) interactions between vericiguat and drugs used in HF (sacubitril/valsartan [SV] and aspirin [acetylsalicylic acid]) or with a narrow therapeutic index (warfarin) were evaluated in three phase I studies.
Results
Vericiguat 15 mg (single dose [SD]) had no effect on bleeding time or platelet aggregation when coadministered with aspirin 1000 mg versus aspirin alone: estimated differences in least squares means 2.7% (95% confidence interval [CI] − 90.4 to 95.8) and 2.4% (95% CI − 7.0 to 11.8) turbidimetry, respectively. Vericiguat 10 mg (once daily) had no effect on coagulation inhibition elicited by warfarin 25 mg (SD; mean ratios of area under the concentration–time curve from time zero to 96 h for clotting parameter treatment comparisons approximated 100.0%). There were no clinically relevant PD changes whether SV 97/103 mg was administered with single or multiple doses of vericiguat 2.5 mg or placebo (differences in systolic blood pressure [BP] − 1.66 mmHg [90% CI − 4.22 to 0.90]; diastolic BP − 1.80 mmHg [90% CI − 3.24 to − 0.36]; heart rate − 0.33 beats/min [90% CI − 2.25 to 1.60]). Vericiguat demonstrated no PK interactions when coadministered with aspirin, warfarin, or SV at steady state. Treatments were well tolerated.
Conclusions
Coadministration of vericiguat with SV, aspirin, or warfarin was well tolerated. No clinically relevant PD or PK interactions were observed, supporting concomitant use of these drugs, commonly used by patients with HF, with vericiguat and no dose adjustment.
EudraCT number
2014-000765-52; 2014-004880-19; 2015-004809-16.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patients with heart failure (HF) with reduced ejection fraction often have multiple comorbidities and receive concomitant medications |
Vericiguat coadministered with sacubitril/valsartan (SV), aspirin (acetylsalicylic acid), or warfarin was well tolerated, with no clinically relevant pharmacodynamic or pharmacokinetic interactions observed |
These findings support concomitant use of SV, aspirin, or warfarin, commonly used by patients with HF, with vericiguat |
1 Introduction
Heart failure (HF) is a rising global problem [1]. Despite advances in management and prevention, the morbidity and mortality associated with HF remains high [1,2,3], underlining the need for more effective strategies.
Vericiguat, a direct stimulator of soluble guanylate cyclase, has been investigated as a first-in-class therapy for patients with chronic HF with reduced ejection fraction (HFrEF) following a worsening event in the phase III VICTORIA study (NCT02861534) [4, 5] and in patients with HF with preserved ejection fraction [6]. As one in six patients with HFrEF develop worsening events within 18 months of diagnosis [7], the availability of new treatment options for these patients is needed.
Previous studies demonstrated that vericiguat is rapidly absorbed, displays dose-proportional pharmacokinetics (PK), and has an acceptable safety profile [8, 9]. In the SOCRATES-REDUCED study (NCT01951625), vericiguat treatment resulted in dose-dependent reductions in N-terminal pro-B-type natriuretic peptide, a biomarker for HF, in stabilized patients with HF following a worsening event and reduced ejection fraction, indicating its potential value in such patients [10].
During the development of vericiguat, the angiotensin receptor–neprilysin inhibitor sacubitril/valsartan (SV) was approved as a treatment for patients with HFrEF at a target dose of 97 mg/103 mg twice daily [11, 12]. SV is recommended to replace angiotensin-converting enzyme inhibitors in ambulatory patients with HFrEF who remain symptomatic despite optimal therapy [13] and in newly diagnosed patients with HFrEF [14]. It is therefore likely that SV will be coadministered with vericiguat in patients with HF following a worsening event. Furthermore, patients with HFrEF often present with multiple comorbidities and concomitant medications [13, 15]. Previous PK studies show vericiguat is unlikely to be a victim or perpetrator of drug–drug interactions (DDIs) [16, 17]; however, given the possibility of interactions, a clinical evaluation of the PK and pharmacodynamic (PD) effects of coadministration of vericiguat with drugs frequently administered to patients with HFrEF will be useful to inform future clinical practice.
Three PD DDI studies between vericiguat and drugs often prescribed in HF populations (SV, warfarin, aspirin [acetylsalicylic acid]), including one with a narrow therapeutic index (warfarin), were conducted in healthy volunteers. In this study, we describe the results of these phase I studies, which investigated the potential PD and PK interactions between vericiguat and SV, warfarin, and aspirin.
2 Methods
2.1 Study Population
Healthy male volunteers with a body mass index (BMI) of 18.0–30.0 kg/m2 and aged 18–45 or 18–55 years were eligible for participation in the aspirin and warfarin studies, respectively. Male subjects with a BMI of 18.0–29.9 and aged 40–60 years were eligible for participation in the SV study. A total of 15, 29, and 32 subjects were randomized in the aspirin, warfarin, and SV studies, respectively. Exclusion criteria included known hypersensitivity to study drug or reference drugs; regular use of medications up to 4 weeks before study drug administration; second- or third-degree atrioventricular block; prolonged QRS complex of > 120 ms or a QTc interval > 450 ms; systolic blood pressure (SBP) < 100 mmHg or > 145 mmHg; diastolic blood pressure (DBP) < 60 mmHg or > 95 mmHg (only DBP > 95 mmHg for the aspirin study); and heart rate (HR) < 50 or > 90 beats/min. Owing to safety reasons and the combination of two cardioactive drugs in the SV study, the exclusion criteria included a QRS complex interval of > 100 ms. Concomitant medication use other than the study drug was not permitted without informing the study investigator.
Participants gave written informed consent to participate before entering the studies. Studies were conducted in accordance with the currently accepted version of the Declaration of Helsinki—the International Conference on Harmonisation Good Clinical Practice Guideline. All protocol and protocol amendments were reviewed by each study site’s Independent Ethics Committee (IEC) or Institutional Review Board (IRB) and approved under the leadership of the IEC/IRB of the coordinating investigator (Ethik-Kommission der Aerztekammer Nordrhein, Duesseldorf, Germany) before the start of the study.
2.2 Study Designs, Assessments, and Analysis
All three studies were randomized, single-center studies. Individual study designs and treatment groups are shown in Table 1. In the aspirin study, vericiguat was administered in the fasted state due to analytical reasons involving interferences with clotting parameters, and, due to the effects of food [18], 15 mg was selected such that vericiguat plasma levels would approximate those following administration of 10 mg (fed). In the warfarin study, vericiguat 10 mg once daily was evaluated, as this would have reached steady state by day 6 (warfarin coadministration). In the SV study, vericiguat 2.5 mg was evaluated, as it was well tolerated in phase II studies [10].
2.2.1 Aspirin Interaction Study
This open-label study consisted of two parts: a pilot part, in which subjects received a single dose (SD) of vericiguat 15 mg (3 × 5 mg immediate-release [IR] tablets); and a three-period, crossover main part, in which subjects received three treatments: [(A) vericiguat 15 mg on day 1; (B): aspirin 500 mg on day –1 and day 1; and (C): aspirin 500 mg on day –1 and vericiguat 15 mg concomitantly with aspirin 500 mg on day 1)] in randomized sequence order with a washout period of > 14 days between treatments (Table 1). During treatments B and C, subjects received aspirin 1000 mg over the course of 2 days. The pilot part assessed the safety and tolerability of vericiguat 15 mg (3 × 5 mg IR tablets, fasted state), as the vericiguat 15 mg oral solution was not well tolerated in the first-in-human study [9]. Subjects participated in one part of the study only.
Bleeding time was assessed at a blood pressure of 40 mmHg according to Mielke [19]. Platelet aggregation was determined by the turbidimetric method of Born and Cross [20], using collagen and arachidonic acid as inductive agents, in addition to exploratory analyses using impedance aggregometry on a Multiplate analyzer (Roche Diagnostics International Ltd, Rotkreuz, Switzerland). Bleeding times and platelet aggregation were measured at 0, 1, 2, and 3 h after administration of vericiguat on day 1 (treatment A), and at 0 h on day –1 and 1, 2, and 3 h after study medication on day 1 in treatments B and C.
Blood sampling for PK assessments was taken before dosing and at regular intervals up to 48 h. Plasma concentrations of vericiguat were determined by high-performance liquid chromatography with tandem mass spectrometry. PK parameters were calculated using WinNonlin version 5.3 (Pharsight Corporation, Mountain View, CA, USA).
2.2.2 Warfarin Interaction Study
Subjects received a single ‘priming’ dose of warfarin 25 mg (day –21), followed by multiple doses (MDs) of vericiguat 10 mg or placebo (once daily, days 1–9), with an SD of warfarin 25 mg (day 6) (Table 1). The priming dose was administered 21 days before the start of the study such that any residual effects of the R- and S-enantiomers of warfarin would be negligible. Warfarin administration was unblinded, whereas vericiguat/placebo administration was double-blinded.
Clotting profiles (prothrombin time [PT], activated partial prothrombin time [aPTT], international normalized ratio [INR], and clotting factors II, VII, and X) were measured at screening (within 14 days before the ‘priming’ warfarin dose), day −21 through to day –17, and day 1 (predose) through to day 13 and follow-up. The effect of vericiguat with warfarin was assessed by calculating the area under the concentration–time curve from time zero to 96 h (AUC96) of the clotting parameters, i.e. PT and factors VII, II, and X [21, 22].
Blood samples for vericiguat PK assessments were taken before dosing on days 2, 3, and 4, and before dosing and at regular intervals on study days 5 and 6 up to day 7. To investigate the possible effect of warfarin on vericiguat, blood samples for a PK profile of vericiguat were taken at 0, 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, and 15 h on day 5 (without warfarin) and day 6 (with warfarin).
The predefined time points for measuring bleeding time and platelet aggregation, and for INRs, were selected based on previous studies with the soluble guanylate cyclase stimulator riociguat coadministered with warfarin [23] and aspirin [24, 25], and the anticoagulant rivaroxaban coadministered with warfarin and aspirin [26].
For PK investigations, plasma concentrations of R- and S-warfarin and vericiguat were determined on the day of warfarin administration (day 6) in treatment A (vericiguat plus warfarin) and treatment B (placebo plus warfarin) until 120 h postdose.
2.2.3 Sacubitril/Valsartan Interaction Study
This was a single-blind, placebo-controlled study with two parallel treatment groups and two treatment periods, separated by a washout period of 7–10 days. In period 1, subjects received vericiguat 2.5 mg once daily or placebo on day 1. In period 2, eligible subjects commenced a run-in phase, starting at the recommended initial dose of SV 49/51 mg twice daily for 14 days (days 1–14) and uptitrating to SV 97/103 mg twice daily for 13 days (days 15–27) [11, 12]. Subjects then received a combination of vericiguat 2.5 mg once daily (or placebo) with SV 97/103 mg twice daily for 14 days (days 28–41 inclusive) (Fig. 1).
Hemodynamic profiles consisted of SBP, DBP, and HR measurements on all profile days, including day 1 of period 1 (vericiguat 2.5 mg/placebo), and days 1 (SV 49/51 mg alone), 15 (SV 97/103 mg twice daily), 27 (SV 97/103 mg twice daily), 28 (SV 97/103 mg twice daily + vericiguat 2.5 mg/placebo), and 41 (SV 97/103 mg twice daily + vericiguat 2.5 mg/placebo) of period 2. Hemodynamic measurements were recorded at the same time of the day to account for circadian variability.
Blood samples for PK assessments of vericiguat were taken pre-vericiguat dose and at 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, and 15 h postdose on day 1 (period 1), day 28 (period 2), and day 41 (period 2), and once in the morning on day 2 (period 1), day 29 (period 2), and day 42 (period 2). Blood samples for PK assessments of sacubitril and valsartan were taken pre-SV dose until 12 h after administration of SV (morning doses) on days 27, 28, and 41 (period 2). PK parameters for vericiguat and SV (metabolites) were calculated to assess the effect of a SD and MDs of vericiguat 2.5 mg on the PK of SV 97/103 mg at steady state. The effect of SV 97/103 mg on vericiguat 2.5 mg (SD) was also evaluated.
2.3 Safety Evaluation
Safety assessments in all studies included recording of all adverse events (AEs) and serious AEs (SAEs), vital signs, physical examinations, and laboratory assessments.
2.4 Statistical Analysis
Statistical evaluation was performed using SAS software (SAS Institute Inc., Cary, NC, USA).
2.4.1 Pharmacodynamic (PD) Analyses
In the aspirin study, summary statistics were calculated for bleeding time and platelet aggregation. Analysis of covariance (ANCOVA) was performed on baseline-adjusted bleeding time and platelet aggregation.
In the warfarin study, treatments were compared with respect to AUC96 for PT, factor VII, and factor II and X clotting activity through ANCOVA after log transformation of the data. Point estimates and 90% confidence intervals (CIs) for the vericiguat plus warfarin/placebo plus warfarin ratios of the true means were calculated. No effect of vericiguat on coagulation inhibition by warfarin was determined if the 90% CI for AUC96 of PT and factor VII (main parameters) were within the intervals of 95.0–105.0% and 90.0–111.0%, respectively.
In the SV study, changes in seated SBP, DBP, and HR after the SV dose on day 41 were analyzed using ANCOVA. Point estimates (least squares mean) and exploratory 90% CIs for treatment differences were calculated.
2.4.2 Pharmacokinetic Analyses
In the main part of the aspirin study and in the warfarin study, the PK characteristics AUC and maximum plasma concentration (Cmax) of vericiguat were analyzed assuming log-normally distributed data. The logarithms of these characteristics were analyzed using analysis of variance (ANOVA). A lack of PK interaction was concluded if the 90% CI for the AUC and Cmax ratios were in the range of 80.0–125.0%. For safety assessments, descriptive analyses were performed.
3 Results
Most baseline characteristics were generally similar across the studies. In the SV study, mean age was notably higher than in the aspirin and warfarin studies (Table 2) due to study design and age inclusion criteria in order to obtain data from a population representative of HF.
3.1 Aspirin Study
In the pilot part, 11 subjects received and completed treatment with SD vericiguat 15 mg. As the vericiguat 15 mg dose was safe and well tolerated, treatment continued with the 15 mg dose in the main part, in which 13 subjects were valid for PD analysis and 14 were valid for safety and PK analyses. One subject dropped out due to an SAE of appendicitis, which was not related to the study drug, and one subject withdrew due to concomitant medication.
3.1.1 Pharmacodynamic Findings
Bleeding times within 3 h after administration of vericiguat 15 mg alone showed minor deviations from the mean baseline (381 s [6.35 min]), with mean changes (standard deviation) from baseline of 32.3 s (162.2 s) at 1 h postdose to −57.7 s (87.0 s) at 3 h postdose. The mean bleeding time following aspirin alone increased from 312 s (5.21 min) at baseline to a maximum of 557 s (9.29 min) at 2 h postdose. Following coadministration of aspirin with vericiguat, the mean bleeding time changed from 399 s (6.65 min) at baseline to a maximum of 9.8 min, 1 h after the second dose of aspirin plus vericiguat. No significant differences in bleeding time were demonstrated between aspirin plus 15 mg vericiguat and aspirin alone [Δ2.7 s (95% CI −90.4 to 95.8)], an order of magnitude lower than that observed for aspirin alone.
Platelet aggregation was unaffected by treatment with vericiguat 15 mg (SD) alone. Mean values varied by < 5% in the turbidimetric method. Following administration of aspirin, alone or with vericiguat 15 mg, mean platelet aggregation after arachidonic acid stimulation decreased immediately to below the lower limit of quantitation. Using collagen stimulation, maximum differences from baseline were similar for aspirin alone (−44.8% ± 14.2%) and aspirin plus vericiguat 15 mg (−45.6% ± 17.4%). The mean change from baseline in collagen-induced aggregation measured by turbidimetry was 2.4% (95% CI −7.0 to 11.8; p = 0.598). No significant difference in platelet aggregation resulted from the addition of vericiguat 15 mg to treatment with aspirin alone.
Impedance aggregometric results generally supported those of the turbidimetric method. The time course of platelet aggregation is depicted in Fig. 2.
Pharmacodynamic interactions—platelet aggregation. Data are expressed as means ± standard deviation. Treatments were vericiguat 15 mg, aspirin 500 mg, and vericiguat 15 mg plus aspirin 2 × 500 mg (500 mg administered qd for 2 days). a Impedance aggregometry, arachidonic acid; b impedance aggregometry, collagen-induced; both measured in units; and c turbidimetry, collagen-induced measured in percentages (PD analysis set, n = 13). Values below the LLOQ were substituted by half the LLOQ for the calculation of statistics. LLOQ lower limit of quantification, PD pharmacodynamic, qd once daily
3.1.2 Pharmacokinetic Findings
Mean ratios of vericiguat 15 mg plus aspirin/vericiguat 15 mg alone for AUC and Cmax were 94.9% (90% CI 84.7–106.3) and 93.2% (90% CI 81.1–107.3), respectively.
3.1.3 Safety Findings
A total of 12 of the 14 treated subjects (85.7%) in the main part of the study reported treatment-emergent AEs (TEAEs). One subject experienced an SAE of acute appendicitis, unrelated to study medication, and was discontinued from the study prior to receiving treatment B. Ten subjects (71.4%) reported at least one TEAE after treatment with vericiguat alone, seven (53.8%, n = 13) after treatment with aspirin alone, and five (38.5%, n = 13) after the combination of vericiguat and aspirin. Most TEAEs were mild in intensity (Table 3).
3.2 Warfarin Study
A total of 23 healthy male subjects were included in the PD and PK analysis sets and 29 were included in the safety analysis set. Seven subjects dropped out postrandomization (five subjects withdrew themselves, one subject dropped out due to a protocol violation, and one was withdrawn due to an AE of increased lipase, unrelated to study medication).
3.2.1 Pharmacodynamic Findings
Least squares mean ratios (values provided as percentages) of AUC96 for the treatment comparisons vericiguat plus warfarin/placebo plus warfarin for PT and factors VII, II, and X were 100.1% (90% CI 99.1–101.2), 97.4% (90% CI 95.5–99.3), 100.0% (90% CI 97.8–102.2), and 100.4% (90% CI 98.2–102.6), respectively. The 90% CIs of the treatment comparisons for the main parameters, PT and factor VII, were within the predefined ranges of 95.0–105.0% (PT) and 90.0–111.0 (factor VII). The point estimates for the secondary parameters, factors II and X, approximated 100.0%, with 90% CIs within the predefined range. Furthermore, no clinically significant changes were observed in clotting parameters at follow-up (14 days after the last study drug administration) and the prothrombin INR ratio remained unchanged at follow-up relative to screening levels. Therefore, no effect of MDs of vericiguat 10 mg on the coagulation inhibition elicited by an SD of warfarin 25 mg was observed (Fig. 3).
Point estimates, 90% CIs, and 95% prediction intervals for the ratio vericiguat plus warfarin/placebo plus warfarin of PD parameters and prothrombin INR. a Prothrombin time; b factor VII activity; c factor II activity; d factor X activity; and e INR by treatment. The shaded boxes represent the IQR (25th–75th percentiles). The line inside the box represents the median, and the rhombus inside the box represents the arithmetic mean. Whiskers represent the maximum value below 1.5*IQR above the 75th percentile and the minimum value above 1.5*IQR below the 25th percentile. Symbols outside the whiskers represent outliers. CIs confidence intervals, INR international normalized ratio, IQR interquartile range, PD pharmacodynamic, IQR interquartile range, AUC96 area under the concentration–time curve from time zero to 96 h after dosing
3.2.2 Pharmacokinetic Findings
The concentration–time profiles for R-warfarin and S-warfarin were similar in both treatments (Fig. 4). The ANOVA analyses of the PK of R- and S-warfarin yielded point estimates for the ratios vericiguat plus warfarin/placebo plus warfarin of AUC and Cmax which approached 100.0% (Table 4). All 90% CIs were included in the predefined bioequivalence range of 80.0–125.0%. No PK interactions were observed after administration of MDs of vericiguat with warfarin compared with MDs of placebo with warfarin. In addition, no influence of warfarin on the PK of vericiguat was observed.
Geometric mean/standard deviation for concentrations of drugs in plasma (n = 23). Mean plasma concentration profile of a R-warfarin, b S-warfarin, and c vericiguat. Square symbols represent vericiguat plus warfarin; circular symbols represent placebo plus warfarin (a, b). Square symbols represent profile day 5; circular symbols represent profile day 6 (c)
3.2.3 Safety Findings
In total, 14 of 29 subjects (48.3%) who received treatment had at least one TEAE, none of which were considered warfarin-related. Seven subjects (24.1%) experienced at least one TEAE related to vericiguat/placebo treatment (Table 3). Generally, TEAEs were of mild or moderate intensity and resolved by the end of the study. One subject discontinued the study due to an event of increased lipase, which was judged as unrelated to vericiguat or warfarin.
3.3 Sacubitril/Valsartan Study
A total of 30 subjects were included in the PD analysis set. The safety and PK analysis sets consisted of 32 and 29 subjects, respectively.
3.3.1 Pharmacodynamic Findings
Mean change from baseline and point estimates for the difference of SV plus vericiguat, and SV plus placebo, for SBP, DBP, and HR are shown in Table 5. No significant PD interactions between vericiguat and placebo with SV were observed for SBP and HR. DBP was significantly decreased with SV plus vericiguat compared with SV plus placebo, by < 2 mmHg.
3.3.2 Pharmacokinetic Findings
The concentration–time profiles showed a slight decrease in vericiguat concentration 2–8 h postdose when administered in conjunction with SV (data not shown). The 90% CIs for the point estimates for the ratio of SV plus vericiguat (day 28) to vericiguat alone (day 1) for AUC24 and Cmax fell within the prespecified bioequivalence range of 80.0–125.0%, indicating no evidence for an effect of SV (MDs) on a SD of vericiguat PK (Table 6).
The ratio of vericiguat plus SV (day 41)/SV alone (day 27) indicated an 18.2% increase in the maximum observed drug concentration (Cmax,md) of sacubitril. Exposure and peak concentration of LBQ657 (sacubitrilat), the active metabolite of sacubitril, remained virtually unchanged (Table 6). In the placebo group, a similar but inverse trend was observed with a decrease in Cmax,md of sacubitril. For valsartan, exposure and peak concentration were increased with SV plus MDs of vericiguat relative to SV alone of approximately 12% and 13%, respectively (Table 6). However, similar increases for valsartan were also seen in the placebo group (AUC: 20,400 μg·h/L on day 27 and 23,000 μg·h/L on day 41; Cmax,md: 3830 μg/L on day 27 and 4760 μg/L on day 41). The 90% CIs for the ratios of sacubitril and valsartan were within the bioequivalence range of 80.0–125.0%, except for the ratios of Cmax of sacubitril, with a SD and MDs of vericiguat, and for the ratios of AUC12,md and Cmax,md of valsartan after MDs of vericiguat.
3.3.3 Safety Findings
In total, 19 (59.4%) of the 32 subjects in the safety analysis had at least one TEAE. Of these, seven subjects (21.9%) experienced one or more TEAEs, considered to be related to vericiguat/placebo; 13 subjects (40.6%) had TEAEs related to SV. The most common overall TEAEs were nervous system disorders, reported for 11 subjects (34.4%), especially headache, reported for seven subjects (21.9%), followed by biochemical investigations, reported for 10 subjects (31.3%). Seven subjects received concomitant medication for the treatment of AEs during the study.
TEAEs were mild (16 subjects, 50.0%) to moderate (three subjects, 9.4%) in maximum intensity. No SAEs occurred in the study (Table 7). One subject discontinued the study due to a TEAE of increased levels of glutamate dehydrogenase related to SV, which had started before coadministration of vericiguat and SV. All TEAEs were resolved by the end of the study.
4 Discussion
These three studies in healthy volunteers investigated the safety and tolerability, as well as the potential PD and PK interactions, of vericiguat administered with a number of drugs commonly used in patients with HF. Combinations of vericiguat with aspirin, warfarin, or SV were well tolerated, and no significant or clinically relevant effects on PD or PK parameters were observed. The studies were in line with US FDA guidance [27].
Vericiguat 15 mg (SD) alone had no effect on bleeding time or platelet aggregation. As expected, aspirin treatment extended bleeding times from baseline measurements, and combining aspirin with vericiguat had no additional effects on this parameter. Platelet aggregation decreased relative to baseline in subjects treated with aspirin, but there was no change from baseline with vericiguat alone. Moreover, the combination of aspirin with vericiguat did not decrease platelet aggregation any further than with aspirin alone, confirming a lack of interaction between vericiguat and aspirin, and that no dose adjustment is required when administered together. A previous study in mice demonstrated that soluble guanylate cyclase has an important role in platelet aggregation [28]. The current findings are in line with a previous DDI study of another soluble guanylate cyclase stimulator, riociguat, which likewise demonstrated no clinically relevant interaction with aspirin [25].
None of the ANOVA analyses supported a difference in the bioavailability of vericiguat when administered alone or when coadministered with aspirin. Although the ANOVA for the fraction of unbound vericiguat indicated an increase of unbound drug of approximately 20% after coadministration with aspirin, this was negligible as the unbound fraction of vericiguat is approximately 2% with or without administration of aspirin, indicating coadministration of aspirin had no effect on the systemic exposure of vericiguat.
As exposure remained unchanged in the warfarin study, during the first 96 h poststudy drug administration and also at follow-up, we concluded no short- or long-term PD effect of MDs of vericiguat on the coagulation inhibition elicited by an SD of warfarin (on day 6) was observed. The long-term effects were in line with a previous model, which considers patient genotypes that affect anticoagulant response and the delay between warfarin exposure and INR response [29,30,31].
Similarly, no PK interactions between warfarin and vericiguat were observed after administration of MDs of vericiguat 10 mg with a SD of warfarin 25 mg. All 90% CIs were within the predefined bioequivalence range of 90% CI 80.0–125.0%, indicating no effect of the combination treatment on the maximum plasma levels and overall exposure of R- and S-warfarin. These findings are in line with a previous PK/PD interaction study of riociguat that concluded riociguat had no clinically relevant interaction with warfarin [25]. In a similar manner, our results show that warfarin does not affect the PK of vericiguat.
Because SV is approved for the treatment of HFrEF [11, 12], we investigated the effects of vericiguat on the PD and PK profile of SV 97/103 mg twice daily. As a proportion of patients with HFrEF will likely be prescribed SV, there is a possibility that vericiguat could be coadministered with SV in future practice. SV acts by inhibiting neprilysin, resulting in increased cyclic guanosine monophosphate. Owing to the involvement of cyclic guanosine monophosphate, common to the mechanism of action of vericiguat, the potential for PK and PD DDIs during coadministration of SV and vericiguat was investigated. The SV interaction study did not reveal any clinically relevant PD interactions between vericiguat and SV (at steady state). When SV was coadministered with vericiguat, there was a reduction in DBP of < 2 mmHg compared with SV plus placebo, which is not clinically relevant. Furthermore, coadministration of vericiguat and SV had no effect on the Cmax and AUC of SV or vericiguat alone. The slight increase in exposure of sacubitril between days 27 and 41 was likely due to intersubject variability of sacubitril concentrations as previously described [32]. With high variability of sacubitril between subjects during the first hour after SV administration until Cmax of sacubitril and increases in valsartan exposure from days 27 to 41 also seen in the placebo group, neither deviation from the equivalence range is likely to be related to interactions with vericiguat. Overall, neither an SD nor MDs of vericiguat 2.5 mg showed a clinically relevant impact on the PK of SV, nor MDs of SV 97/103 mg on the PK of vericiguat.
5 Conclusions
Coadministration of vericiguat together with SV, aspirin, or warfarin was well tolerated. Vericiguat, alone or in combination with aspirin, had no effect on bleeding time or platelet aggregation, and there was no change in coagulation inhibition when vericiguat was administered with warfarin. There were no clinically relevant effects of SV, aspirin, or warfarin on the PK or PD of vericiguat. In addition, there were no relevant effects of vericiguat on the PK of SV or warfarin. Together, these findings support concomitant use of SV, aspirin, or warfarin with vericiguat without the need for dose adjustment.
References
Cook C, Cole G, Asaria P, Jabbour R, Francis DP. The annual global economic burden of heart failure. Int J Cardiol. 2014;171(3):368–76.
Cheng RK, Cox M, Neely ML, Heidenreich PA, Bhatt DL, Eapen ZJ, et al. Outcomes in patients with heart failure with preserved, borderline, and reduced ejection fraction in the Medicare population. Am Heart J. 2014;168(5):721–30.
Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, et al. Heart failure: preventing disease and death worldwide. ESC Heart Fail. 2014;1(1):4–25.
Armstrong PW, Roessig L, Patel MJ, Anstrom KJ, Butler J, Voors AA, et al. A multicenter, randomized, double-blind, placebo-controlled trial of the efficacy and safety of the oral soluble guanylate cyclase stimulator: the VICTORIA trial. JACC Heart Fail. 2018;6(2):96–104.
Armstrong PW, Pieske B, Anstrom KJ, Ezekowitz J, Hernandez AF, Butler J, et al. Vericiguat in patients with heart failure and reduced ejection fraction. N Engl J Med. 2020;382(20):1883–93.
Butler J, Lam CSP, Anstrom KJ, Ezekowitz J, Hernandez AF, O'Connor CM, et al. Rationale and design of the VITALITY-HFpEF trial. Circ Heart Fail. 2019;12(5):e005998.
Butler J, Yang M, Manzi MA, Hess GP, Patel MJ, Rhodes T, et al. Clinical course of patients with worsening heart failure with reduced ejection fraction. J Am Coll Cardiol. 2019;73(8):935–44.
Boettcher M, Loewen S, Gerrits M, Becker C. Pharmacodynamic and pharmacokinetic interaction profile of vericiguat. European Society of Cardiology Heart Failure 2019 Congress; 25–28 May 2019: Athens. P1183.
Boettcher M, Thomas D, Mueck W, Loewen S, Arens E, Yoshikawa K, et al. Safety, pharmacodynamic and pharmacokinetic characterisation of vericiguat: key results from six phase I studies in healthy subjects. European Society of Cardiology Heart Failure 2019 Congress; 25–28 May 2019: Athens.
Gheorghiade M, Greene SJ, Butler J, et al. Effect of vericiguat, a soluble guanylate cyclase stimulator, on natriuretic peptide levels in patients with worsening chronic heart failure and reduced ejection fraction: the SOCRATES-REDUCED randomized trial. J Am Med Assoc. 2015;314:2251–62.
electronic Medicines Compendium. Entresto SmPC. 2018 [cited Jul 2019]. https://www.medicines.org.uk/emc/product/5074/smpc.
Novartis Pharmaceuticals Corporation. Entresto prescribing information. 2018 [cited Jul 2019]. https://www.pharma.us.novartis.com/sites/www.pharma.us.novartis.com/files/entresto.pdf.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18(8):891–975.
Seferovic PM, Ponikowski P, Anker SD, Bauersachs J, Chioncel O, Cleland JGF, et al. Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21(10):1169–86.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136(6):e137–e161161.
Lobmeyer M, Gerisch M, Boettcher M-F, Thomas D, Gerrits M, Mueck W, et al. Metabolism and pharmacokinetic drug interaction profile of vericiguat, a soluble guanylate cyclase stimulator. Eur J Heart Fail. 2019;21 Suppl. S1:425.
Boettcher M, Gerisch M, Lobmeyer M, Besche N, Thomas D, Gerrits M, et al. Metabolism and pharmacokinetic drug-drug interaction profile of vericiguat, a soluble guanylate cyclase stimulator: results from preclinical and phase I healthy volunteer studies. Clin Pharmacokinet. 2020. https://doi.org/10.1007/s40262-020-00895-x.
Becker C, Boettcher M, Loewen S, Mueck W. Biopharmaceutical profile, bioavailability, food effect, and pharmacokinetics of vericiguat: a novel soluble guanylate cyclase stimulator [abstract no. M1430-13-86]. The American Association of Pharmaceutical Scientists (AAPS); 3–6 Nov 2019; San Antonio, TX.
Mielke CH. Measurement of the bleeding time. Thromb Haemost. 1984;52(2):210–1.
Born GV, Cross MJ. The aggregation of blood platelets. J Physiol. 1963;168:178–95.
Duursema L, Müller FO, Hundt HKL, Heyns ADP, Meyer BH, Luus HG. Model to detect warfarin–drug interactions in man. Drug Investig. 1992;4(5):395–402.
Grind M, Murphy M, Warrington S, Aberg J. Method for studying drug–warfarin interactions. Clin Pharmacol Ther. 1993;54(4):381–7.
Frey R, Mück W, Kirschbaum N, Krätzschmar J, Weimann G, Wensing G. Warfarin pharmacodynamics and pharmacokinetics are not affected by the soluble guanylate cyclase stimulator riociguat (BAY 63–2521). BMC Pharmacol. 2009;9 Suppl 1:15.
Frey R, Becker C, Saleh S, Unger S, van der Mey D, Mück W. Clinical pharmacokinetic and pharmacodynamic profile of riociguat. Clin Pharmacokinet. 2018;57(6):647–61.
Frey R, Reber M, Kratzschmar J, Unger S, Muck W, Wensing G. Riociguat (BAY 63–2521) and aspirin: a randomized, pharmacodynamic, and pharmacokinetic interaction study. Pulm Circ. 2016;6(Suppl 1):S35–42.
Mueck W, Stampfuss J, Kubitza D, Becka M. Clinical pharmacokinetic and pharmacodynamic profile of rivaroxaban. Clin Pharmacokinet. 2014;53(1):1–16.
Food and Drug Administration. Clinical drug interaction studies—study design, data analysis, and clinical implications guidance for industry. 2017 [cited 8 Jul 2019]. https://www.fda.gov/media/82734/download.
Zhang G, Xiang B, Dong A, Skoda RC, Daugherty A, Smyth SS, et al. Biphasic roles for soluble guanylyl cyclase (sGC) in platelet activation. Blood. 2011;118(13):3670–9.
Hamberg AK, Wadelius M, Lindh JD, Dahl ML, Padrini R, Deloukas P, et al. A pharmacometric model describing the relationship between warfarin dose and INR response with respect to variations in CYP2C9, VKORC1, and age. Clin Pharmacol Ther. 2010;87(6):727–34.
Jin B, Hong Y, Zhu J, Li Y, Shi HM. The impact of VKORC1-1639G > A genetic polymorphism upon warfarin dose requirement in different ethnic populations. Curr Med Res Opin. 2014;30(8):1505–11.
Zhang H, Ma K, Liu W, Yang F, Liu J, Zhou H. Impact of CYP2C19 gene polymorphism on warfarin maintenance doses in patients with non-valvular atrial fibrillation. Gene. 2016;591(1):80–4.
Shi J, Wang X, Nguyen J, Wu AH, Bleske BE, Zhu HJ. Sacubitril is selectively activated by carboxylesterase 1 (CES1) in the liver and the activation is affected by CES1 genetic variation. Drug Metab Dispos. 2016;44(4):554–9.
Acknowledgements
Medical writing and editorial assistance were provided by Laila Guzadhur, PhD. This assistance was funded by Bayer AG, Berlin, Germany, and Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. Part of this analysis was presented at the 2019 European Society of Cardiology Heart Failure Congress.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Michael Boettcher and Corina Becker are employees of Bayer AG and may own stock in the company. Stephanie Loewen is an employee of Chrestos Concept GmbH & Co. KG, and a paid consultant for Bayer Healthcare Pharmaceuticals. At the time of performing the studies Mireille Gerrits was an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA.
Funding
Funding for this research was provided by Bayer AG, Berlin, Germany, and Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the relevant IEC or IRB and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards, and the International Conference on Harmonisation guideline E6: Good Clinical Practice (GCP).
Consent to participate
Written informed consent was obtained from individuals in each study.
Consent for publication
All authors drafted the article and/or revised it critically for important intellectual content and provided final approval of the published version.
Availability of data and materials
Availability of the data underlying this publication will be determined according to Bayer’s commitment to the EFPIA/PhRMA “Principles for responsible clinical trial data sharing”. This pertains to scope, timepoint and process of data access. As such, Bayer commits to sharing upon request from qualified scientific and medical researchers patient-level clinical trial data, study-level clinical trial data, and protocols from clinical trials in patients for medicines and indications approved in the United States (US) and European Union (EU) as necessary for conducting legitimate research. This applies to data on new medicines and indications that have been approved by the EU and US regulatory agencies on or after January 1, 2014. Interested researchers can use http://www.clinicalstudydatarequest.com to request access to anonymized patient-level data and supporting documents from clinical studies to conduct further research that can help advance medical science or improve patient care. Information on the Bayer criteria for listing studies and other relevant information is provided in the Study sponsors section of the portal. Data access will be granted to anonymized patient-level data, protocols and clinical study reports after approval by an independent scientific review panel. Bayer is not involved in the decisions made by the independent review panel. Bayer will take all necessary measures to ensure that patient privacy is safeguarded.
Code availability
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Boettcher, M., Loewen, S., Gerrits, M. et al. Pharmacodynamic and Pharmacokinetic Interaction Profile of Vericiguat: Results from Three Randomized Phase I Studies in Healthy Volunteers. Clin Pharmacokinet 60, 337–351 (2021). https://doi.org/10.1007/s40262-020-00935-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-020-00935-6