Abstract
Background
Kidney replacement therapy (KRT) is a lifesaving but costly treatment for patients with end-stage kidney disease (ESKD). The objective of this study was to review full economic evaluations comparing KRT modalities specified as hemodialysis (HD), peritoneal dialysis (PD), and kidney transplantation (KT) for patients with ESKD.
Methods
We conducted a systematic review of the literature from PubMed, Embase, EconLit (EBSCO), Web of Science, Cochrane Library, National Health Service Economic Evaluation Database (NHS EED), Centre for Reviews and Dissemination (CRD) Database of Abstracts of Reviews of Effects (DARE), and CRD Health Technology Assessment Database from inception until 5 January 2020. Full economic evaluations were included if they compared three forms of KRT specified as PD, HD, and KT. The reporting quality of included studies was assessed using the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist.
Results
Ten studies were identified in the review. The majority of the studies were model-based evaluations and included a cost-utility analysis. Four studies were conducted from a public healthcare perspective, three from a societal perspective, and three from a third-party payer perspective. None of the studies adequately addressed all the applicable items of the CHEERS checklist. The most infrequently reported items were characterizing heterogeneity, target population, and characterizing uncertainty. There is a lack of studies that conduct from a societal perspective and take into account characterizing heterogeneity. All included studies indicate that KT is the most cost-effective KRT modality, with either a dominant position over HD and PD or an incremental cost-effectiveness ratio well below the accepted willingness-to-pay threshold. The majority of studies suggest that PD is less costly and offers comparable or better health outcomes than HD.
Conclusions
Our systematic review suggests that KT is the most cost-effective KRT modality, but there is no firm conclusion about the cost-effectiveness of HD and PD. Further economic evaluations can be conducted from a societal perspective and detail the evidence for subsets of patients with different characteristics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Kidney transplantation is the most cost-effective kidney replacement therapy modality, but there is no firm conclusion about the cost-effectiveness of hemodialysis and peritoneal dialysis. |
Future economic evaluations of the kidney replacement therapy modality can be conducted from a societal perspective and take into account characterizing heterogeneity. |
1 Introduction
End-stage kidney disease (ESKD) is the final and permanent stage of chronic kidney disease (CKD) [1]. The increasing prevalence of ESKD has been a significant public healthcare challenge worldwide [2]. From 2003 to 2016, the ESKD prevalence has steadily increased worldwide, with a median percent increase of 43% [3]. In 2016, ESKD prevalence ranging from 600 to 999 per million general population (PMP) was reported in approximately 45% of countries [3]. Driven by population aging and the rising incidence of diabetes and hypertension, the prevalence of ESKD is expected to rise to an even greater extent in the next few decades [1, 4, 5].
Kidney replacement therapy (KRT) is a lifesaving but costly treatment for patients with ESKD [6]. There are three primary forms of KRT, namely hemodialysis (HD), peritoneal dialysis (PD), and kidney transplantation (KT) [2]. HD is principally performed in dialysis centers by healthcare workers but also can be carried out independently by patients at home [7]. PD is predominantly performed by patients at home without assistance from clinical staff [8]. Globally, the number of people receiving KRT was more than 2.6 million in 2010 and this number is projected to more than double to 5.4 million by 2030 [6]. The use of the different KRT modalities varies considerably across countries and regions. In 2016, KT for patients with ESKD ranged from less than 20% in roughly one-third of countries to 50–70% in approximately one-quarter of countries [3]. In-center HD was the predominant KRT modality in most countries and it accounted for more than 80% of dialysis in 79% of countries in 2016 [3]. Several countries and regions have initiated PD-First policies or PD-Favored policies to encourage the use of PD as the first treatment modality for appropriate patients because PD is deemed to have lower costs than HD, comparable survival and improved quality of life (QOL) [9,10,11,12]. Accordingly, higher rates of PD uptake were reported in those countries and regions, such as Hong Kong (71%), the Jalisco region of Mexico (61%), and Guatemala (57%) [3].
The rising prevalence of ESKD and extensive use of KRT have challenged the economic capacity of many countries, especially in low-income countries where there are limited resources and a large gap in access to KRT [7]. Approximately 64% of countries provided public funding for KRT [13]. It is estimated that total ESKD expenditure accounts for 0.91–7.1% of national health system expenditure in countries with a high prevalence of ESKD even though ESKD patients contribute a relatively small proportion of the entire CKD population [14].
As the burden of ESKD on society and healthcare budgets has increased considerably, it is essential to assess the cost-effectiveness of the different KRT modalities to establish cost-effective service provision strategies. An economic evaluation is a comparative analysis that examines two or more interventions in terms of their costs and consequences. It can provide useful insight for prioritizing the programs in the healthcare sector and for optimal resource allocation [15]. Several economic evaluations have been conducted regionally. Nevertheless, there have been few systematic reviews of economic evaluations of all KRT modalities. Previous systematic studies in this area have focused on subsets of KRT modalities, such as comparing alternative dialysis modalities [8, 16] or dialysis modalities with different intensities [17]. Therefore, this study aims to review full economic evaluations comparing KRT modalities specified as PD, HD, and KT for patients with ESKD.
2 Methods
2.1 Data Sources and Search Strategies
This review was conducted according to the guidelines of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) (see Resource 1, Online Supplemental Material (OSM)) [18]. Studies were identified by searching electronic databases and scanning reference lists of relevant studies. The electronic databases, including PubMed, Embase, EconLit (EBSCO), Web of Science, Cochrane Library, National Health Service Economic Evaluation Database (NHS EED), Centre for Reviews and Dissemination (CRD) Database of Abstracts of Reviews of Effects (DARE), and CRD Health Technology Assessment Database, were systematically searched from inception until 5 January 2020. The search strategy used Medical Subject Headings (MeSH) terms and a range of text words pertinent to the identification of studies that included KRT modalities of PD, HD, and KT, and text words relevant to economic evaluations. The search strategies are provided in Resource 2 (OSM).
2.2 Eligibility Criteria
For inclusion, the following criteria had to be fulfilled: (1) full economic evaluations that considered both costs and effects, including cost–benefit analysis (CBA), cost-utility analysis (CUA), cost-effectiveness analysis (CEA), and cost-minimization analysis (CMA); (2) comparing three forms of KRT specified as PD, HD, and KT; (3) studies in the English language. All alternative modalities of PD (e.g., automated PD, continuous ambulatory PD), HD (e.g., home HD, in-center HD, nocturnal home HD), and KT (e.g., living-donor transplantation (LT), deceased-donor transplantation (DT)) were considered for inclusion. Exclusion criteria were: (1) partial economic evaluations, such as outcome description, cost description, cost-outcome description, effectiveness evaluation, and cost analysis; (2) systematic reviews, commentaries, congress abstracts; (3) studies without at least three comparators of PD, HD, and KT. No limits were applied for country, publication date, and publication status.
2.3 Study Selection
Two reviewers independently performed the study selection in an unblended standardized manner. The titles and abstracts of all citations were evaluated to identify articles for full-text review. Any citations without electronically available abstracts were discarded unless the title was convincing of the study’s relevance. Full-text publications were reviewed by two reviewers using the pre-defined eligibility criteria. All disagreements between reviewers were resolved by discussion and consensus.
2.4 Data Extraction and Risk of Bias Assessment
We extracted the following items from each included study: general study characteristics (author, publication year, country, study population, type of economic evaluations, study design, study perspective), model design and structure (model type, cycle length, time horizon, discount rate, number and names of key states/pathways), parameter sources and values (health outcomes, utility values, data sources for utility values, methods of measurement of utility, type and category of included costs, country and reference year of costs, cost values, data sources for cost values), summary of cost-effectiveness results (incremental cost-effectiveness ratios (ICERs), main results, type of sensitivity analyses, outcomes of sensitivity analyses, author’s/authors’ conclusions). One reviewer completed the extraction and the second reviewer checked the extracted data with disagreement resolved by consensus. The risk of bias of included studies was assessed using the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist [19]. All assessments were performed and agreed upon by two reviewers.
3 Results
3.1 Study Selection
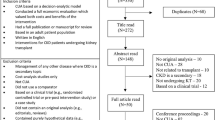
The initial search of electronic databases provided a total of 3784 citations. After adjusting for duplicates, 3236 abstracts were screened and the full-text articles of 91 citations were examined in more detail. Of these, nine studies met the inclusion criteria and were included in the review. One additional study that met the inclusion criteria was identified by scanning reference lists of relevant studies and review articles. A total of ten studies were identified for inclusion in the systematic review. Figure 1 shows the flow diagram of the study selection.
3.2 Study Characteristics
Table 1 provides a summary of the included studies. The included studies were from upper-middle-income countries and high-income countries. The study population of all studies were patients with ESKD, but only four studies described characteristics of the base case population [20, 24, 27, 29]. Five of the ten studies conducted a CUA [20,21,22,23,24], one conducted a CEA [25], and four conducted both a CEA and CUA [26,27,28,29]. Eight studies were model-based economic evaluations using Markov models [20,21,22,23, 26,27,28,29] and the remaining two studies were a multicenter cross-section study [24] and a retrospective cohort study [25], respectively. Four studies were conducted from a public healthcare perspective [21, 22, 24, 27], three from a societal perspective [20, 23, 29] and three from a third-party payer perspective [25, 26, 28].
3.3 Quality of Reporting and Risk of Bias within Studies
Figure 2 shows the proportions of included studies that complied with applicable items of the CHEERS checklist. None of the included studies addressed all the applicable items of the CHEERS checklist. The most infrequently reported items were characterizing heterogeneity, target population and subgroups, and characterizing uncertainty. About 60% of the studies failed to describe characteristics of the base-case population. All studies stated the time horizon, but none of them clearly described the rationale for choosing the specified time horizon. Most of the studies failed to describe the population used to elicit preference-based outcomes, even though they reported methods used to derive utility values. Four studies did not report value ranges or probability distributions for parameters. In terms of characterizing uncertainty, five studies were restricted to exploring the effects of a few input parameters and none of the studies explored the uncertainty related to the structure of the model and assumptions. One criterion that may have the potential for a higher risk of bias was the characterizing heterogeneity. Most studies did not conduct subgroup analyses, while the study that had conducted subset analyses did not report differences in outcomes between subgroups [29]. The performance of each included study for the CHEERS checklist can be found in Resource 3 (OSM).
3.4 Model Design and Structure
Table 2 shows the characteristics of the model design and structure. A variety of time horizons were employed in the included studies, varying from 2, 5, 6, 10, and 15 years to lifetime horizons. The cycle length in the models was either 1 month or 1 year, aside from one model that did not specify the cycle length [29]. The discounting is the same for costs and outcomes within each study, with discounting rates varying from 3%, 3.5%, 5% to 6%, aside from one study that explicitly ruled out discounting on the basis of their 2-year time horizon [25]. The majority of model-based economic evaluations used a four-state Markov model approach and the remaining studies developed the Markov model with eight, 12, and 38 states. Moradpour et al. [20] and Villa et al. [23] used the same four-state model structure, but the model by Moradpour et al. [20] applied the 1-month cycle length and the model by Villa et al. [23] applied the 1-year cycle length. Haller et al. [27] defined 12 different states depending on time of initiation of a certain treatment modality. The study by de Wit et al. [29] combined six treatment modalities, three age-groups, and two treatment stages to define 36 states.
3.5 Parameter Sources and Values
3.5.1 Parameter Sources and Values for Utility
In terms of effectiveness outcomes, nine out of ten studies used QALYs as the main outcome measure. Therefore, this review focuses on the derivation of utility values.
Table 3 presents the parameter sources and values. Data sources for utility values include observational surveys and previous literature. The methods used to measure utility values include Time Trade-Off (TTO), Standard Gamble (SG), EuroQol five-dimension scale (EQ-5D), Health Utilities Index (HUI), and SF-6D derived from SF-36 health survey. Moradpour et al. [20], Kontodimopoulos et al. [24], and de Wit et al. [29] obtained their utility scores from their observational surveys, and the remainder used utility values from previous literature. None of those studies obtaining utility values from previous literature fully describe the population characteristics of their cited studies. In the study by Jensen et al. [21], the utility values were derived from Sennfält et al. [30], who used the EQ-5D instrument to investigate a matched population in Sweden. Haller et al. [27] used the utility values directly from de Wit et al. [29]. The study by de Wit et al. [29] used SG, TTO, and EQ-5D to assess dialysis patients’ health states. It is worth noting that de Wit et al. [29] estimated the utility for KT based on three previous studies rather than by interview. Moradpour et al. [20] investigated a total of 214 ESKD patients using the Euro QOL EQ-5D-5L Persian version and they failed to report the main patient characteristics according to the KRT modality. Kontodimopoulos et al. [24] surveyed a total sample of 874 nationally representative ESKD patients and obtained their SF-6D utilities derived from SF-36. It should be noted that, in the study by Kontodimopoulos et al. [24], KT patients were significantly younger and had less co-morbidities than PD and HD patients, which may influence the utilities measured.
There is a wide range of utility values across the included studies. The utility values for HD ranged from 0.44 to 0.72; for PD from 0.53 to 0.81; for KT from 0.57 to 0.90. In seven of the nine studies, KT utility was higher than PD utility, and PD utility was higher than HD utility [20,21,22, 24, 26]. In two of the nine studies, KT utility was higher than PD and HD utility, with PD and HD utility being equal [23, 28]. The study by de Wit et al. [29] suggests that conflicting results of utility valuations existed among different valuation methods. For example, continuous ambulatory PD patients’ EQ-5D scores were higher than those of center HD patients, while continuous ambulatory PD patients’ SG and TTO scores were lower than those of center HD patients.
3.5.2 Parameter Sources and Cost Inputs
Cost inputs were generally obtained from a combination of multiple sources, including the study hospitals, national institutions, published studies, expert opinion, and interviews with patients. Most of the studies reported adequate information on the key data sources, methods of cost estimation, the breakdown of cost items, currency, and the price year. However, it is not clearly reported in most studies whether resource use was valued at charges or real costs. Four studies [20, 24, 25, 27] obtained some of their resources from databases reflecting actual patient healthcare use, which facilitates the accuracy of the costs associated with each treatment modality. Moradpour et al. [20] and de Wit et al. [29] obtained their data on direct non-medical costs and indirect costs from interviews with patients.
There was a wide variety of types and categories of included costs, with the majority of studies including only the direct healthcare costs (such as diagnostic costs, outpatient routine costs, and hospitalization costs). Three of the ten studies claimed to have been conducted from a societal perspective [20, 23, 29], but only one study considered the productivity losses of patients and caregivers [20]. Although de Wit et al. [29] claimed to have adopted a societal perspective, they excluded time costs and indirect costs (productivity loss) in the cost analysis. Six of the ten studies differentiated between costs in the first year and subsequent years after initiation of KRT [22, 24, 25, 27,28,29]. This cost differentiation is necessary given that KT costs accumulate primarily in the first year and decrease substantially in subsequent years.
3.6 Summary of Cost-Effectiveness Results
3.6.1 Cost-Effectiveness Results
Table 4 summarizes the main results of the included studies. The variability in study design and study perspective hampers our ability to conduct a quantitative statistical analysis to combine the results of included studies. Overall, the majority of studies showed that KT was the most cost-effective KRT modality, and PD was more cost-effective than HD. Most studies suggested that KT held a dominant position over HD and PD with both lower costs and higher effectiveness [21, 22, 24, 26,27,28,29]. Studies conducted by Moradpour et al. [20] and Sesso et al. [25] indicated that KT did not dominate but was cost-effective compared with dialysis at the given willingness-to-pay (WTP) thresholds. All but the study by Sesso et al. [25] suggested that PD was more cost-effective than HD. Five out of ten studies evaluated the cost-effectiveness of different KRT assignment strategies [22, 23, 27,28,29]. These studies suggested that increased uptake of KT and PD by new ESKD patients would reduce costs and improve health outcomes or would be more cost-effective than current practice patterns.
3.6.2 Analyses of Uncertainty
The issue of uncertainty was only partially explored in deterministic sensitivity analyses and probabilistic sensitivity analyses (PSA). All of the reviewed studies conducted sensitivity analyses to explore the implications of parameter uncertainty for the results of economic evaluations. However, none of the model-based economic evaluations dealt with the uncertainty related to the structure of the model. Moradpour et al. [20], Rosselli et al. [26], and Jensen et al. [21] performed PSA, while the remaining seven studies only performed deterministic one-way sensitivity analysis. Half of the included studies [20, 21, 23, 26, 27] performed sensitivity analyses for all input parameters, including transition probabilities, costs, and utilities. There was no key input parameter that was consistently influential across the included studies. In the majority of the studies, sensitivity analyses suggested that parameter changes did not substantially influence the results.
4 Discussion
4.1 Statement of Principal Findings
4.1.1 Model Design and Structure
All included model-based studies used a Markov model, indicating that these studies considered this approach appropriate for modelling ESKD. The structure of each model seemed adequate for reflecting the ESKD-specific health processes. All but one study [25] used time horizons of greater than 5 years, which seems suitable to reflect the long-term treatment outcomes. The study by Howard et al. [28] is the only study that contained time-dependent probabilities. Given that a patient characteristic may determine future patient pathways, the use of individual-level microsimulation could be of value in this condition. In addition, guidelines on good modeling practice advocate the need to explore structural uncertainty, which include simplifications and scientific judgments regarding the construction and interpretation of a model [44]. Nevertheless, none of the studies justified their approach in a sensitivity analysis.
4.1.2 Parameter Sources and Measurement
To some degree, there is a lack of availability of utility data sources with high quality for ESKD patients. The included studies used utility values from previous literature or observational surveys. Rosselli et al. [26] and Villa et al. [23] conducted a literature review to obtained utility values. However, this review was not systematic and they did not provide a critical appraisal of the primary studies included in their review. Several included studies derived their utility values from different sources, which makes it difficult to assess the validity of the results. In addition, utility values derived from observational studies are likely to suffer from selection bias given that study subjects were not randomly assigned to a treatment modality. Jensen et al. [21] obtained utility values from the previous literature by Sennfält et al. [30], which is the only study that aimed to minimize selection bias by matching on selected covariates, such as age, diabetes, heart disease, and living situation. However, this study had a relatively small sample size that comprised 27 matched triplets, thereby affecting the reliability of the results. In study by Haller et al. [27], there were differences in patient characteristics among HD, PD, and KT groups, with HD patients on average being more than 10 years older than PD and KT patients, which might impact the effectiveness of the three modalities. Nonetheless, Haller et al. [27] failed to explicitly discuss issues related to these differences and the impact that they could have on the results.
This raises a concern that the differences in utility values of three KRT modalities might be partly determined by the differences in patient characteristics and conditions. Sculpher points out that [45] the subgroup differences in cost-effectiveness can be attributed to different types of heterogeneity that can be associated with the treatment, the underlying disease, or patient preference. Previous studies suggest that patients commencing PD are usually younger and self-determined healthier individuals, while those commencing HD are in worse conditions and of older age [7, 27]. Given that most included studies did not report the population used to derive utility values or perform subgroup analyses, it remains unclear whether the differences in utility values can be explained by variations between subgroups of patients with different characteristics. Furthermore, it is unclear to what extent the cost-effectiveness results will be impacted by the selection bias.
In terms of cost inputs, the data sources for cost inputs in most reviewed studies were appropriate as they included the most relevant data sources in their setting. Most of the studies provided adequate details on the data sources, methods of cost estimation, and the breakdown of cost items, which enhances the validity of their cost measurement. The variation in the source and type of costs confounds evaluation of costs and makes it challenging to compare across studies.
The study perspective essentially determines the scope of costs that need to be accounted for in the economic evaluations [15]. Nonetheless, it is worth noting that two studies attempted societal perspective analyses but showed no evidence of indirect costs, especially productivity loss, in their analyses. Compared with the third-party payer and public healthcare perspective, the societal perspective considers a broader scope of healthcare costs and other costs associated with the relevant stakeholders in the society, such as time costs of informal caregivers and productivity loss of patients. The societal perspective allows for the identification of the transfer costs from the healthcare system to the household and society [8]. Hence, growing importance has been attached to considering the indirect costs borne by patients and their families [15, 36]. HD is primarily administered in ambulant dialysis units, while PD is predominantly performed at home [37]. The adoption of home-based HD and PD can shift some burden onto family members [27]. Moreover, previous studies show that KT patients have significantly higher employment rates compared with dialysis patients, with employment rates of 11–32% in HD patients, 28–50% in PD patients, and 30–70% in KT recipients [38,39,40,41,42,43]. The societal perspective can provide decision makers with a more comprehensive understanding of the cost-effectiveness of alternative options and may result in an optimal resource allocation in decision making.
4.1.3 Implications from Cost-Effectiveness Results
Overall, evidence collected from included studies indicates that KT is the most cost-effective KRT modality, with either a dominant position over HD and PD or an ICER well below the accepted WTP threshold. Although the data on costs and health outcomes are country-specific in each study, the comparative costs and effectiveness of KT relative to dialysis modalities are similar across studies. This finding remains consistent over time even though the clinical practice of KRT is likely to evolve. In addition, the majority of included studies suggest that PD is less costly and offers comparable or better health outcomes than HD. We interpret this finding with caution, as the evidence regarding this issue was inconclusive. In terms of cost differences between PD and HD, the majority of studies indicate that PD is a cost-saving therapy compared to HD. The lower cost of PD may be attributable to the minimal use of equipment, infrastructure, and staff time since PD is a primarily home-based treatment option [20]. Nonetheless, the study by Howard et al. [28] indicates that dialysis cost is highly health system-specific and their professional staff expenditure can vary widely from country to country. In terms of health outcomes, several studies assumed equal survival for HD and PD patients [20, 23, 27]. In terms of QOL, HD patients are inclined to have better social interaction and less isolation fear [31, 32]. In contrast, PD patients tend to report less illness intrusion, higher satisfaction, and better renal care [33, 34]. Overall, however, previous studies suggest that no significant difference in QOL exists between PD and HD patients [9, 29, 35]. Therefore, there is limited ability to generalize the finding that PD is more favorable than HD beyond the specific settings and assumptions.
Most of the included studies suggest that KT and PD should be prioritized and encouraged as a primary strategy for KRT for eligible patients when planning KRT services. Nonetheless, it should be noted that modality selection is a complex issue that can be driven by both medical and non-medical factors. Medical factors, such as contraindications, may disqualify patients from choosing a certain modality [46]. Under this circumstance, the cost-effectiveness findings may not be able to override the medical determinants of the modality selection. The cost-effectiveness findings can be of value in situations where non-medical factors play a significant role in influencing modality selection. Financial reimbursement policies have been identified as the most important non-medical factor contributing to modality selection [10]. In several countries that have initiated PD-First policies, efforts have been made to revise the reimbursement policy in a way to encourage utilization of PD [10]. In this sense, the cost-effectiveness findings that KT and PD are more favorable KRT modalities have essential policymaking implications.
Although it has been shown consistently across studies that KT is the optimal KRT modality, the expansion of KT may be challenging to achieve given the limited availability of donor organs. It is estimated that less than 20% of treated ESKD patients are living with a KT in approximately one-third of countries [3]. Therefore, in order to promote cost-effective management of ESKD, it is of great importance to implement specific strategies aimed at increasing kidney donations, such as reducing financial disincentive to living donors, improving donor transplant coordination, and increasing the use of expanded criteria donors [47, 48].
4.2 Strengths and Limitations
To our knowledge, this is the first systematic review that has focused on economic evaluations that compared three forms of KRT modalities specified as HD, PD, and KT. We included numerous electronic databases and manually searched the reference lists of relevant studies to ensure the sensitivity of the search strategy. The studies included in our review were conducted in several countries and represented various healthcare systems. Moreover, two reviewers independently carried out the study screening, data extraction and study appraisal, which reduced potential bias in the review process.
Our review has several limitations. First of all, we could not combine data across studies to draw any definitive conclusions regarding the cost-effectiveness of KRT modalities because of the heterogeneity in study designs. As described, all studies varied in their study designs, such as study perspective, cost category and estimations, time horizons, and model structure. Hence, it is impossible to convert findings across studies into a common estimation for comparison. Second, we included studies that compare HD, PD, and KT and excluded studies that compare only one modality or a mix of two different types of dialysis because other researchers have already carried out a systematic review or meta-analysis on them, while studies comparing all three modalities exist but nobody has reviewed them. Third, we excluded studies published in non-English languages and thus there is a potential omission of relevant articles from some cultures or ethnic backgrounds. Fourth, our review focused solely on the published literature, which represents a potential publication bias. Finally, we used the CHEERS checklist to appraise the included studies, which is prone to subjective reviewer judgments.
4.3 Considerations for Future Research
Our review has important implications for future research. First, considering the productivity costs associated with the KRT modality, more economic evaluations can be conducted from a societal perspective to quantify indirect costs such as productivity loss borne by patients and their families. Second, though most established models seemed adequate for reflecting the disease and its progression, many studies assumed time-independent probabilities for switching between modalities. Future research might expand more on complicated models to reflect the real-world disease progression and treatment patterns. Third, evidence on the cost-effectiveness of KRT modality in different subgroups of patients is scarce, with no included study having addressed the item of characterizing heterogeneity in the CHEERS checklist. The results may be confounded by differences between subgroups other than the KRT modality. Therefore, if feasible, further studies should also detail the evidence for subsets of patients with different characteristics. Finally, as evidence from future studies becomes available, it is necessary to update the assessment of the cost-effectiveness of KRT modality.
References
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–33.
Vanholder R, Annemans L, Brown E, Gansevoort R, Gout-Zwart JJ, Lameire N, et al. Reducing the costs of chronic kidney disease while delivering quality health care: a call to action. Nat Rev Nephrol. 2017;13:393–409.
United States Renal Data System. 2018 USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128.
Jha V, Garcia-Garcia G, Iseki K, Li Z, Naicker S, Plattner B, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382(9888):260–72.
Liyanage T, Ninomiya T, Jha V, Jha V, Neal B, Patrice HM, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–82.
Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al. Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure. Health Technol Assess. 2003;7(2):1–174.
Howell M, Walker RC, Howard K. Cost effectiveness of dialysis modalities: a systematic review of economic evaluations. Appl Health Econ Health Policy. 2019;17:315–30.
Chaudhary K, Sangha H, Khanna R. Peritoneal dialysis first: rationale. Clin J Am Soc Nephrol. 2011;6(2):447–56.
Liu FX, Gao X, Inglese G, Chuengsaman P, Pecoits-Filho R, Yu A. A global overview of the impact of peritoneal dialysis first or favored policies: an opinion. Perit Dial Int. 2015;35(4):406–20.
Yang CW, Harris DCH, Luyckx VA, Nangaku M, Hou FF, Garcia GG, et al. Global case studies for chronic kidney disease/end-stage kidney disease care. Kidney Int Suppl. 2020;10(1):e24–e48.
Li PK-T, Chow KM. Peritoneal dialysis-first policy made successful: perspectives and actions. Am J Kidney Dis. 2013;62(5):993–1005.
Bello AK, Levin A, Lunney M, Osman MA, Ye F, Ashuntantang GE, et al. Status of care for end stage kidney disease in countries and regions worldwide: international cross sectional survey. BMJ. 2019;367:l5873. https://doi.org/10.1136/bmj.l5873.
Ismail H, Abdul Manaf MR, Abdul Gafor AH, Mohamad Zaher ZM, Nur Ibrahim AI. International comparisons of economic burden of end-stage renal disease to the national healthcare systems. IIUM Med J Malays. 2019;18(3):188–96.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 4th ed. Oxford: Oxford University Press; 2015.
Walker R, Marshall MR, Morton RL, McFarlane P, Howard K. The cost-effectiveness of contemporary home haemodialysis modalities compared with facility haemodialysis: a systematic review of full economic evaluations. Nephrology. 2014;19(8):459–70.
Laplante S, Liu FX, Culleton B, Bernardo A, King D, Hudson P. The cost effectiveness of high-dose versus conventional haemodialysis: a systematic review. Appl Health Econ Health Policy. 2016;14:185–93.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:2535.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated health economic evaluation reporting standards (CHEERS) statement. Value Health. 2013;16(2):e1–5.
Moradpour A, Hadian M, Tavakkoli M. Economic evaluation of end stage renal disease treatments in Iran. Clin Epidemiol Glob Health. 2020;8(1):199–204.
Jensen CE, Sorensen P, Petersen KD. In Denmark kidney transplantation is more cost-effective than dialysis. Dan Med J. 2014;61(3):A4796.
Shimizu U, Saito S, Lings Y, Iino N, Kazama JJ, Akazawa K. Cost-effectiveness achieved through changing the composition of renal replacement therapy in Japan. J Med Econ. 2012;15(3):444–53.
Villa G, Fernandez-Ortiz L, Cuervo J, Rebollo O, Selgas R, Gonzalez T, et al. Cost-effectiveness analysis of the Spanish renal replacement therapy program. Perit Dial Int. 2012;32(2):192–9.
Kontodimopoulos N, Niakas D. An estimate of lifelong costs and QALYs in renal replacement therapy based on patients’ life expectancy. Health Policy. 2008;86(1):85–96.
Sesso R, Eisenberg JM, Stabile C, Draibe S, Ajzen H. Cost-effectiveness analysis of the treatment of end-stage renal disease in Brazil. Int J Technol Assess Health Care. 1990;6(1):107–14.
Rosselli D, Rueda JD, Diaz CE. Cost-effectiveness of kidney transplantation compared with chronic dialysis in end-stage renal disease. Saudi J Kidney Dis Transpl. 2015;26(4):733–8.
Haller M, Gutjahr G, Kramar R, Harnoncourt F, Oberbauer R. Cost-effectiveness analysis of renal replacement therapy in Austria. Nephrol Dial Transpl. 2011;26(9):2988–95.
Howard K, Salkeld G, White S, McDonald S, Chadban S, Craig JC, et al. The cost-effectiveness of increasing kidney transplantation and home-based dialysis. Nephrology. 2009;14(1):123–32.
de Wit GA, Ramsteijn PG, de Charro FT. Economic evaluation of end stage renal disease treatment. Health Policy. 1998;44(3):215–32.
Sennfält K, Magnusson M, Carlsson P. Comparison of hemodialysis and peritoneal dialysis—a cost-utility analysis. Peritoneal Dialysis Int. 2002;22:39–47.
Juergensen E, Wuerth D, Finkelstein SH, Juergensen PH, Bekui A, Finkelstein FO. Hemodialysis and peritoneal dialysis: patients’ assessment of their satisfaction with therapy and the impact of the therapy on their lives. Clin J Am Soc Nephrol. 2006;1(6):1191–6.
McLaughlin K, Manns B, Mortis G, Hons R, Taub K. Why patients with ESRD do not select self-care dialysis as a treatment option. Am J Kidney Dis. 2003;41(2):380–5.
Brown EA, Johansson L, Farrington K, Gallagher H, Sensky T, Gordon F, et al. Broadening options for long-term dialysis in the elderly (BOLDE): differences in quality of life on peritoneal dialysis compared to haemodialysis for older patients. Nephrol Dial Transplant. 2010;25(11):3755–63.
Goodlad C, Brown E. The role of peritoneal dialysis in modern renal replacement therapy. Postgraduate Med J. 2013;89(1056):584–90.
Liem YS, Bosch JL, Arends LR, Heijenbrok-Kal MH, Hunink MG. Quality of life assessed with the Medical Outcomes Study Short Form 36-Item Health Survey of patients on renal replacement therapy: a systematic review and meta- analysis. Value Health. 2007;10(5):390–7.
Gilbertson EL, Krishnasamy R, Foote C, Kennard AL, Jardine MJ, Gray NA. Burden of care and quality of life among caregivers for adults receiving maintenance dialysis: a systematic review. Am J Kidney Dis. 2019;73(3):332–43.
Scholten N, Ohnhaeuser T, Schellartz I, von Gersdorff G, Hellmich M, Karbach U, et al. Multidimensional analysis of factors responsible for the low prevalence of ambulatory peritoneal dialysis in Germany (MAU-PD): a cross-sectional Mixed-Methods Study Protocol. BMJ Open. 2019;9:e025451.
van Manen JG, Korevaar JC, Dekker FW, Reuselaars MC, Boeschoten EW, Krediet RT, NECOSAD Study Group. Netherlands cooperative study on adequacy of dialysis: changes in employment status in end-stage renal disease patients during their first year of dialysis. Perit Dial Int. 2001;21(6):595–601.
Curtin RB, Oberley ET, Sacksteder P, Friedman A. Differences between employed and nonemployed dialysis patients. Am J Kidney Dis. 1996;27(4):533–40.
Hirth RA, Chernew ME, Turenne MN, Pauly MV, Orzol SM, Held PJ. Chronic illness, treatment choice and workforce participation. Int J Health Care Finance Econ. 2003;3(3):167–81.
Rubin HR, Fink NE, Plantinga LC, Sadler JH, Kliger AS, Powe NR. Patient ratings of dialysis care with peritoneal dialysis vs hemodialysis. JAMA. 2004;291(6):697–703.
Helanterä I, Haapio M, Koskinen P, Grönhagen-Riska C, Finne P. Employment of patients receiving maintenance dialysis and after kidney transplant: a cross-sectional study from Finland. Am J Kidney Dis. 2012;59(5):700–6.
van der Mei SF, Krol B, van Son WJ, de Jong PE, Groothoff JW, van den Heuvel WJ. Social participation and employment status after kidney transplantation: a systematic review. Qual Life Res. 2006;15(6):979–94.
Bojke L, Claxton K, Sculpher M, et al. Characterizing structural uncertainty in decision analytic models: a review and application of methods. Value in Health. 2009;12(5):739–49.
Sculpher M. Subgroups and heterogeneity in cost-effectiveness analysis. Pharmacoeconomics. 2008;26(9):799–806.
Blake PG, Quinn RR, Oliver MJ. Peritoneal dialysis and the process of modality selection. Perit Dial Int. 2013;33(3):233–41.
Mathew T, Faull R, Snelling P. The shortage of kidneys for transplantation in Australia. Med J Aust. 2005;182:204–5.
Hamm D, Tizzard J. Presumed consent for organ donation is an ethical and effective way of dealing with organ donation shortages. BMJ. 2008;336:230.
Higashiyama A, Okamura T, Watanabe M, et al. Effect of chronic kidney disease on individual and population medical expenditures in the Japanese population. Hypertens Res. 2009;32:450–4.
Nakatani T, Uchida J, Naganuma T. Health economics of kidney transplant. Jpn J Transplant. 2009;44:18–25 (Japanese).
Lee AJ, Morgan CL, Conway P, et al. Characterisation and comparison of health-related quality of life for patients with renal failure. Curr Med Res Opin. 2005;21:1777–833.
Groome PA, Hutchinson TA, Tousignant P, et al. The repeatability of three methods for measuring prospective patients’ values in the context of treatment choice for end-stage renal disease. J Clin Epidemiol. 1999;52:849–60.
Villa G, Rodríguez-Carmona A, Fernández-Ortiz L, Cuervo J, Rebollo P, Otero A, et al. Cost analysis of the Spanish renal replacement therapy programme. Nephrol Dial Transplant. 2011;26:3709–14.
Agar JW, Knight RJ, Simmonds RE, Boddington JM, Waldron CM, Somerville CA. Nocturnal haemodialysis: an Australian cost comparison with conventional satellite haemodialysis. Nephrology (Carlton). 2005;10:557–70.
Commonwealth Department of Health and Ageing. National Hospital Cost Data Collection. Cost Report Round 8 (2003–2004) AR-DRG v4.2. Canberra: Commonwealth Department of Health and Ageing; 2005.
Accountants BCC. Costing analysis of the renal dialysis services funded by the Health Department of Western Australia. Perth: Health Department of Western Australia; 1999.
Laupacis A, Keown P, Pus N, et al. A study of the quality of life and cost-utility of renal transplantation. Kidney Int. 1996;50:235–42.
Hellenic National Transplant Organization. Interim report on the proposed reimbursement of organ transplants in Greece. Athens: Hellenic National Transplant Organization; 2003 (in Greek).
Hilbrands LB, Hoitsma AJ, Koene RP. Randomized, prospective trial of cyclosporine monotherapy versus azathioprine-prednisone from three months after renal transplantation. Transplantation. 1996;61:1038–46.
Author information
Authors and Affiliations
Contributions
FY and ML designed the study. FY and ML developed the search strategy and screened the studies for eligibility. ML and FY extracted data from the included studies and reviewed reporting against CHEERS. ML and FY drafted the manuscript, with input from PW, ZY and YL. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Funding
This study was funded by the Clinical Cultivation Project Foundation of Southern Medical University [LC2016PY029] and Shenzhen Key Research Base of Humanities and Social Sciences.
Conflict of interest
Fei Yang, Meixia Liao, Pusheng Wang, Zheng Yang, and Yongguang Liu declare that they have no conflicts of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Code availability
Not applicable.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yang, F., Liao, M., Wang, P. et al. The Cost-Effectiveness of Kidney Replacement Therapy Modalities: A Systematic Review of Full Economic Evaluations. Appl Health Econ Health Policy 19, 163–180 (2021). https://doi.org/10.1007/s40258-020-00614-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-020-00614-4