Abstract
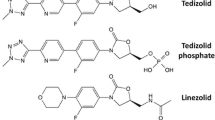
Twenty-one agents are approved by the US Food and Drug Administration (FDA) for the therapy of skin and soft tissue infections. Of these, the five newest agents, tedizolid, telavancin, oritavancin, dalbavancin, and ceftaroline, are active against and “non-inferior” to vancomycin against methicillin-resistant Staphylococcus aureus (MRSA). Oritavancin is indicated as a single-dose intravenous regimen, while dalbavancin is a two-dose intravenous regimen given 1 week apart. Telavancin has multiple mechanisms of action. A 6-day regimen of once-daily intravenous or oral dose of tedizolid was compared with 10 days of linezolid and found to be “non-inferior” and have fewer side effects. Ceftaroline has not only MRSA activity but also activity against Escherichia coli and Klebsiella spp. We review the spectra of activity of these new agents, their clinical trials and their therapeutic efficacy, noting differences in their dosing schedules, in vitro activities and costs as potential determinants for appropriate utilization.
Similar content being viewed by others
References
US Department of Health and Human Services. Guidance for Industry Acute Bacterial Skin and Skin Structure Infections: Developing Drugs for Treatment. Silver Spring: Food and Drug Administration Center for Drug Evaluation and Research, 2013.
Adams PF, Kirzinger WK, Martinez ME. Summary health statistics for the US population: National Health Interview Survey, 2011. National Center for Health Statistics. Vital Health Stat 10(255). 2012.
Pallin DJ, Egan DJ, Pelletier AJ, Espinola JA, Hooper DC, Camargo CA Jr. Increased US emergency department visits for skin and soft tissue infections, and changes in antibiotic choices, during the emergence of community-associated methicillin-resistant Staphylococcus aureus. Ann Emerg Med. 2008;51(3):291–8.
Pallin DJ, Espinola JA, Leung DY, Hooper DC, Camargo CA Jr. Epidemiology of dermatitis and skin infections in United States physicians’ offices, 1993–2005. Clin Infect Dis. 2009;49(6):901–7.
Edelsberg J, Taneja C, Zervos M, Haque N, Moore C, Reyes K, et al. Trends in US hospital admissions for skin and soft tissue infections. Emerg Infect Dis. 2009;15(9):1516–8.
Moran GJ, Abrahamian FM, Lovecchio F, Talan DA. Acute bacterial skin infections: developments since the 2005 Infectious Diseases Society of America (IDSA) guidelines. J Emerg Med. 2013;44(6):e397–412.
Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, McDougal LK, Carey RB, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355(7):666–74.
Kollef MH. Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis. 2000;31(Suppl 4):S131–8.
Dowell JA, Goldstein BP, Buckwalter M, Stogniew M, Damle B. Pharmacokinetic-pharmacodynamic modeling of dalbavancin, a novel glycopeptide antibiotic. J Clin Pharmacol. 2008;48(9):1063–8.
Candiani G, Abbondi M, Borgonovi M, Romano G, Parenti F. In-vitro and in-vivo antibacterial activity of BI 397, a new semi-synthetic glycopeptide antibiotic. J Antimicrob Chemother. 1999;44(2):179–92.
Malabarba A, Goldstein BP. Origin, structure, and activity in vitro and in vivo of dalbavancin. J Antimicrob Chemother. 2005;55 Suppl 2:ii15–20.
Goldstein EJ, Citron DM, Merriam CV, Warren YA, Tyrrell KL, Fernandez HT. In vitro activities of the new semisynthetic glycopeptide telavancin (TD-6424), vancomycin, daptomycin, linezolid, and four comparator agents against anaerobic Gram-positive species and Corynebacterium spp. Antimicrob Agents Chemother. 2004;48(6):2149–52.
Nagarajan R. Antibacterial activities and modes of action of vancomycin and related glycopeptides. Antimicrob Agents Chemother. 1991;35(4):605–9.
Bennett JW, Lewis JS, Ellis MW. Dalbavancin in the treatment of complicated skin and soft-tissue infections: a review. Ther Clin Risk Manag. 2008;4(1):31–40.
Jones RN, Sader HS, Flamm RK. Update of dalbavancin spectrum and potency in the USA: report from the SENTRY Antimicrobial Surveillance Program (2011). Diagn Microbiol Infect Dis. 2013;75(3):304–7.
Citron DM, Tyrrell KL, Goldstein EJ. Comparative in vitro activities of dalbavancin and seven comparator agents against 41 Staphylococcus species cultured from osteomyelitis infections and 18 VISA and hVISA strains. Diagn Microbiol Infect Dis. 2014;79(4):438–40.
Buckwalter M, Dowell JA. Population pharmacokinetic analysis of dalbavancin, a novel lipoglycopeptide. J Clin Pharmacol. 2005;45(11):1279–87.
Boucher HW, Wilcox M, Talbot GH, Puttagunta S, Das AF, Dunne MW. Once-weekly dalbavancin versus daily conventional therapy for skin infection. N Engl J Med. 2014;370(23):2169–79.
Jauregui LE, Babazadeh S, Seltzer E, Goldberg L, Krievins D, Frederick M, et al. Randomized, double-blind comparison of once-weekly dalbavancin versus twice-daily linezolid therapy for the treatment of complicated skin and skin structure infections. Clin Infect Dis. 2005;41(10):1407–15.
Allen NE, Nicas TI. Mechanism of action of oritavancin and related glycopeptide antibiotics. FEMS Microbiol Rev. 2003;26(5):511–32.
McKay GA, Beaulieu S, Arhin FF, Belley A, Sarmiento I, Parr T Jr, et al. Time-kill kinetics of oritavancin and comparator agents against Staphylococcus aureus, Enterococcus faecalis and Enterococcus faecium. J Antimicrob Chemother. 2009;63(6):1191–9.
Belley A, Arhin FF, Sarmiento I, Deng H, Rose W, Moeck G. Pharmacodynamics of a simulated single 1,200-milligram dose of oritavancin in an in vitro pharmacokinetic/pharmacodynamic model of methicillin-resistant Staphylococcus aureus infection. Antimicrob Agents Chemother. 2013;57(1):205–11.
Arhin FF, Sarmiento I, Parr TR Jr, Moeck G. Activity of oritavancin and comparators in vitro against standard and high inocula of Staphylococcus aureus. Int J Antimicrob Agents. 2012;39(2):159–62.
Mendes RE, Farrell DJ, Sader HS, Flamm RK, Jones RN. Activity of oritavancin against Gram-positive clinical isolates responsible for documented skin and soft-tissue infections in European and US hospitals (2010–13). J Antimicrob Chemother. 2015;70(2):498–504.
Morrissey I, Seifert H, Canton R, Nordmann P, Stefani S, Macgowan A, et al. Activity of oritavancin against methicillin-resistant staphylococci, vancomycin-resistant enterococci and beta-haemolytic streptococci collected from Western European countries in 2011. J Antimicrob Chemother. 2013;68(1):164–7.
Dunbar LM, Milata J, McClure T, Wasilewski MM. Comparison of the efficacy and safety of oritavancin front-loaded dosing regimens to daily dosing: an analysis of the SIMPLIFI trial. Antimicrob Agents Chemother. 2011;55(7):3476–84.
Rubino CM, Van Wart SA, Bhavnani SM, Ambrose PG, McCollam JS, Forrest A. Oritavancin population pharmacokinetics in healthy subjects and patients with complicated skin and skin structure infections or bacteremia. Antimicrob Agents Chemother. 2009;53(10):4422–8.
Corey GR, Kabler H, Mehra P, Gupta S, Overcash JS, Porwal A, et al. Single-dose oritavancin in the treatment of acute bacterial skin infections. N Engl J Med. 2014;370(23):2180–90.
Corey GR, Good S, Jiang H, Moeck G, Wikler M, Green S, et al. Single-dose oritavancin versus 7–10 days of vancomycin in the treatment of Gram-positive acute bacterial skin and skin structure infections: the SOLO II Noninferiority Study. Clin Infect Dis. 2015;60(2):254–62.
Shaw KJ, Poppe S, Schaadt R, Brown-Driver V, Finn J, Pillar CM, et al. In vitro activity of TR-700, the antibacterial moiety of the prodrug TR-701, against linezolid-resistant strains. Antimicrob Agents Chemother. 2008;52(12):4442–7.
Schaadt R, Sweeney D, Shinabarger D, Zurenko G. In vitro activity of TR-700, the active ingredient of the antibacterial prodrug TR-701, a novel oxazolidinone antibacterial agent. Antimicrob Agents Chemother. 2009;53(8):3236–9.
Rodriguez-Avial I, Culebras E, Betriu C, Morales G, Pena I, Picazo JJ. In vitro activity of tedizolid (TR-700) against linezolid-resistant staphylococci. J Antimicrob Chemother. 2012;67(1):167–9.
Livermore DM, Mushtaq S, Warner M, Woodford N. Activity of oxazolidinone TR-700 against linezolid-susceptible and -resistant staphylococci and enterococci. J Antimicrob Chemother. 2009;63(4):713–5.
Locke JB, Hilgers M, Shaw KJ. Novel ribosomal mutations in Staphylococcus aureus strains identified through selection with the oxazolidinones linezolid and torezolid (TR-700). Antimicrob Agents Chemother. 2009;53(12):5265–74.
Thomson KS, Goering RV. Activity of tedizolid (TR-700) against well-characterized methicillin-resistant Staphylococcus aureus strains of diverse epidemiological origins. Antimicrob Agents Chemother. 2013;57(6):2892–5.
Prokocimer P, Bien P, Deanda C, Pillar CM, Bartizal K. In vitro activity and microbiological efficacy of tedizolid (TR-700) against Gram-positive clinical isolates from a phase 2 study of oral tedizolid phosphate (TR-701) in patients with complicated skin and skin structure infections. Antimicrob Agents Chemother. 2012;56(9):4608–13.
Prokocimer P, De Anda C, Fang E, Mehra P, Das A. Tedizolid phosphate vs linezolid for treatment of acute bacterial skin and skin structure infections: the ESTABLISH-1 randomized trial. JAMA. 2013;309(6):559–69.
Moran GJ, Fang E, Corey GR, Das AF, De Anda C, Prokocimer P. Tedizolid for 6 days versus linezolid for 10 days for acute bacterial skin and skin-structure infections (ESTABLISH-2): a randomised, double-blind, phase 3, non-inferiority trial. Lancet Infect Dis. 2014;14(8):696–705.
Prokocimer P, Bien P, Surber J, Mehra P, DeAnda C, Bulitta JB, et al. Phase 2, randomized, double-blind, dose-ranging study evaluating the safety, tolerability, population pharmacokinetics, and efficacy of oral torezolid phosphate in patients with complicated skin and skin structure infections. Antimicrob Agents Chemother. 2011;55(2):583–92.
Flanagan S, Bartizal K, Minassian SL, Fang E, Prokocimer P. In vitro, in vivo, and clinical studies of tedizolid to assess the potential for peripheral or central monoamine oxidase interactions. Antimicrob Agents Chemother. 2013;57(7):3060–6.
VIBATIV® (telavancin) for injection, for intravenous use [Package Insert]. South San Francisco: Theravance, Inc.; 2013.
CLSI. Performance standards for antimicrobial susceptibility testing; Twenty-fourth informational supplement, CLSI document M100-S24. Wayne: Clinical and Laboratory Standards Institute; 2015.
Mendes RE, Sader HS, Farrell DJ, Jones RN. Worldwide appraisal and update (2010) of telavancin activity tested against a collection of Gram-positive clinical pathogens from five continents. Antimicrob Agents Chemother. 2012;56(7):3999–4004.
Rubinstein E, Lalani T, Corey GR, Kanafani ZA, Nannini EC, Rocha MG, et al. Telavancin versus vancomycin for hospital-acquired pneumonia due to Gram-positive pathogens. Clin Infect Dis. 2011;52(1):31–40.
Stryjewski ME, O’Riordan WD, Lau WK, Pien FD, Dunbar LM, Vallee M, et al. Telavancin versus standard therapy for treatment of complicated skin and soft-tissue infections due to Gram-positive bacteria. Clin Infect Dis. 2005;40(11):1601–7.
Stryjewski ME, Graham DR, Wilson SE, O’Riordan W, Young D, Lentnek A, et al. Telavancin versus vancomycin for the treatment of complicated skin and skin-structure infections caused by Gram-positive organisms. Clin Infect Dis. 2008;46(11):1683–93.
Stryjewski ME, Barriere SL, O’Riordan W, Dunbar LM, Hopkins A, Genter FC, et al. Efficacy of telavancin in patients with specific types of complicated skin and skin structure infections. J Antimicrob Chemother. 2012;67(6):1496–502.
Polyzos KA, Mavros MN, Vardakas KZ, Makris MC, Rafailidis PI, Falagas ME. Efficacy and safety of telavancin in clinical trials: a systematic review and meta-analysis. PLoS One. 2012;7(8):e41870.
Red Book Online [database online]. Greenwood Village, CO: Truven Health Analytics Inc; 2015.
Goldstein EJ, Citron DM, Merriam CV, Tyrrell KL. Comparative in vitro activity of ceftaroline, ceftaroline-avibactam, and other antimicrobial agents against aerobic and anaerobic bacteria cultured from infected diabetic foot wounds. Diagn Microbiol Infect Dis. 2013;76(3):347–51.
Richter SS, Heilmann KP, Dohrn CL, Riahi F, Costello AJ, Kroeger JS, et al. Activity of ceftaroline and epidemiologic trends in Staphylococcus aureus isolates collected from 43 medical centers in the United States in 2009. Antimicrob Agents Chemother. 2011;55(9):4154–60.
Riccobene T JA, Rank D, Thye DA. An open-label pharmacokinetic, safety and tolerability study of single-dose intravenous ceftaroline in subjects with end-stage renal disease on intermittent haemodialysis. Program and abstracts of the European Congress of Clinical Microbiology and Infectious Diseases. Helsinki, Finland; 2009.
Teflaro® (ceftaroline fosamil) for injection [package insert]. St Louis, MO: Forest Pharmaceuticals; 2013.
Steed ME, Rybak MJ. Ceftaroline: a new cephalosporin with activity against resistant gram-positive pathogens. Pharmacotherapy. 2010;30(4):375–89.
Saravolatz LD, Stein GE, Johnson LB. Ceftaroline: a novel cephalosporin with activity against methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2011;52(9):1156–63.
Corey GR, Wilcox M, Talbot GH, Friedland HD, Baculik T, Witherell GW, et al. Integrated analysis of CANVAS 1 and 2: phase 3, multicenter, randomized, double-blind studies to evaluate the safety and efficacy of ceftaroline versus vancomycin plus aztreonam in complicated skin and skin-structure infection. Clin Infect Dis. 2010;51(6):641–50.
Corey GR, Wilcox MH, Talbot GH, Thye D, Friedland D, Baculik T; CANVAS 1 investigators. CANVAS 1: the first Phase III, randomized, double-blind study evaluating ceftaroline fosamil for the treatment of patients with complicated skin and skin structure infections. J Antimicrob Chemother. 2010;65 Suppl 4:iv41–51. doi:10.1093/jac/dkq254
Wilcox MH, Corey GR, Talbot GH, Thye D, Friedland D, Baculik T; CANVAS 2 investigators. CANVAS 2: the second Phase III, randomized, double-blind study evaluating ceftaroline fosamil for the treatment of patients with complicated skin and skin structure infections. J Antimicrob Chemother. 2010;65 Suppl 4:iv53–65. doi:10.1093/jac/dkq255.
Friedland HD, O’Neal T, Biek D, Eckburg PB, Rank DR, Llorens L, et al. CANVAS 1 and 2: analysis of clinical response at day 3 in two phase 3 trials of ceftaroline fosamil versus vancomycin plus aztreonam in treatment of acute bacterial skin and skin structure infections. Antimicrob Agents Chemother. 2012;56(5):2231–6.
Lipsky BA, Cannon CM, Ramani A, Jandourek A, Calmaggi A, Friedland HD, et al. Ceftaroline fosamil for treatment of diabetic foot infections: the CAPTURE study experience. Diabetes Metab Res Rev. 2014 Nov 21.
Goldstein EJ, Citron DM, Merriam CV, Tyrrell KL. Ceftaroline versus isolates from animal bite wounds: comparative in vitro activities against 243 isolates, including 156 Pasteurella species isolates. Antimicrob Agents Chemother. 2012;56(12):6319–23.
Moise PA, Sakoulas G, Forrest A, Schentag JJ. Vancomycin in vitro bactericidal activity and its relationship to efficacy in clearance of methicillin-resistant Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2007;51(7):2582–6.
Cervera C, Castaneda X, de la Maria CG, del Rio A, Moreno A, Soy D, et al. Effect of vancomycin minimal inhibitory concentration on the outcome of methicillin-susceptible Staphylococcus aureus endocarditis. Clin Infect Dis. 2014;58(12):1668–75.
Miller LG, Eells SJ, David MZ, Ortiz N, Taylor AR, Kumar N, et al. Staphylococcus aureus Skin Infection Recurrences Among Household Members: An Examination of Host, Behavioral, and Pathogen-Level Predictors. Clin Infect Dis. 2014 Nov 26.
(CLSI) CaLSI. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-fourth Informational Supplement; CLSI document M100-S24. Wayne, Pennsylvania 2014.
DALVANCE (dalbavancin) for injection, for intravenous use [Package Insert]: Durata Therapeutics U.S. Limited; 2014.
ORBACTIV (oritavancin) for injection, for intravenous use [Package Insert]. Parsippany, NJ: The Medicines Company; 2014.
ZYVOX® (linezolid) injection, Tablets and oral suspension [Package Insert]. New York, NY: Pharmacia & Upjohn Company; 2011.
Teflaro™ (ceftaroline fosamil) injection for intravenous (IV) use [Package Insert]. St Louis, MO: Forest Pharmaceuticals, Inc.; 2010.
John G. Bartlett PGA, Paul A. Pham John Hopkins Antibiotic Guide; Diagnosis and Treatment of Infectious Diseases 2012.
SIVEXTRO (tedizolid phosphate) for injection, for intravenous use SIVEXTRO (tedizolid phosphate) tablet, for oral use [Package Insert]. Lexington, MA: Cubist Pharmaceuticals; 2014.
CUBICIN ® (daptomycin for injection) [Package Insert]. Lexington, MA: Cubist Pharmaceuticals U.S.; 2014.
Conflict of interest
MC N Tran has no conflict of interest to declare.
S Naumovski has no conflict of interest to declare.
EJC Goldstein is on Advisory Boards for Merck, Bio K+, Bayer, Summit corp plc, Kindred Healthcare corp, Novartis, Sankyo-Daichi, Rempex. He is on the speaker bureau for Bayer Inc, Merck & Co, Forest Pharmaceuticals, Cubist. He has received research grants from Merck, Optimer, GSK, Cubist, Cerexa and Forrest Pharmaceuticals, Cerexa, Impex Pharmaceuticals, Novartis, Clinical Microbiology Institute, Genzyme, Nanopacific Holding Inc, Romark Laboratories LC, Viroxi Corp, Avidbiotics Corp, GLSynthesis Inc, Immunome Inc, Toltec Pharma LLC, Salix, Summit Corp plc, Rempex Pharmaceuticals, Symbiomix Therapeutics, Amicrobe Inc, Durata, Gynuity Heralth Project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tran, MC.N., Naumovski, S. & Goldstein, E.J.C. The Times They Are A-Changin’: New Antibacterials for Skin and Skin Structure Infections. Am J Clin Dermatol 16, 137–146 (2015). https://doi.org/10.1007/s40257-015-0125-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-015-0125-9