Abstract
Aim and background
The underlying mechanism of exercise-induced insulin resistance (IR) improvement is unclear. Adropin is a multifunctional peptide has a significant role in the regulation of physical activity and insulin sensitivity. Thus, the aim of this study was to evaluate the effects of various circuit resistance (CRT) intensities on circulating adropin levels and IR and their relation.
Method
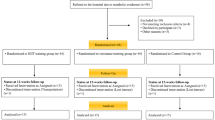
Forty-five voluntarily male men randomly were divided into 5 groups; control and 4 groups of CRT (20%, 40%, 60% and 80% of one-repetition maximum (1-RM)). Training groups performed CRT protocol 3 times a week for 6 weeks. Blood samples were drawn before and 48 h after the last training session and used for analyzing serum levels of adropin, glucose and insulin.
Results
The results showed that varying CRT intensities were associated with adropin elevation in comparison to the control group. Further analysis revealed that plasma adropin is higher in the 20% 1-RM group compared to the 40% 1-RM group. Furthermore, fasting insulin and glucose, as well as IR, were decreased in response to different CRT intensities. In addition, these reductions were significantly correlated with adropin level.
Conclusion
It can be speculated that different CRT intensities improve IR probably via increasing adropin level, and should be considered as an effective training method for diminishing glucose metabolism disorders.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Aydin S, Kuloglu T, Aydin S, Eren MN, Yilmaz M, Kalayci M, et al. Expression of adropin in rat brain, cerebellum, kidneys, heart, liver, and pancreas in streptozotocin-induced diabetes. Mol Cell Biochem. 2013;380(1):73–81.
Ganesh-Kumar K, Zhang J, Gao S, Rossi J, McGuinness OP, Halem HH, et al. Adropin deficiency is associated with increased adiposity and insulin resistance. Obesity. 2012;20(7):1394–402.
Kumar KG, Trevaskis JL, Lam DD, Sutton GM, Koza RA, Chouljenko VN, et al. Identification of adropin as a secreted factor linking dietary macronutrient intake with energy homeostasis and lipid metabolism. Cell Metab. 2008;8(6):468–81.
Wong C-M, Wang Y, Lee JTH, Huang Z, Wu D, Xu A, et al. Adropin is a brain membrane-bound protein regulating physical activity via the NB-3/notch signaling pathway in mice. J Biol Chem. 2014;289(37):25976–86.
Thapa D, Xie B, Manning JR, Zhang M, Stoner MW, Huckestein BR, et al. Adropin reduces blood glucose levels in mice by limiting hepatic glucose production. Physiological reports. 2019;7(8):1–8.
Gao S, McMillan RP, Jacas J, Zhu Q, Li X, Kumar GK, et al. Regulation of substrate oxidation preferences in muscle by the peptide hormone adropin. Diabetes. 2014;63(10):3242–52.
Stein LM, Yosten GL, Samson WK. Adropin acts in brain to inhibit water drinking: potential interaction with the orphan G protein-coupled receptor, GPR19. Am J Phys Regul Integr Comp Phys. 2016;310(6):R476–R80.
Wu L, Fang J, Chen L, Zhao Z, Luo Y, Lin C, et al. Low serum adropin is associated with coronary atherosclerosis in type 2 diabetic and non-diabetic patients. Clin Chem Lab Med (CCLM). 2014;52(5):751–8.
Fujie S, Hasegawa N, Sato K, Fujita S, Sanada K, Hamaoka T, et al. Aerobic exercise training-induced changes in serum adropin level are associated with reduced arterial stiffness in middle-aged and older adults. Am J Phys Heart Circ Phys. 2015;309(10):H1642–H7.
Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement executive summary. Diabetes Care. 2010;33(12):2692–6.
Kolahdouzi S, Baghadam M, Kani-Golzar FA, Saeidi A, Jabbour G, Ayadi A, et al. Progressive circuit resistance training improves inflammatory biomarkers and insulin resistance in obese men. Physiol Behav. 2019;205:15–21.
Eves ND, Plotnikoff RC. Resistance training and type 2 diabetes: considerations for implementation at the population level. Diabetes Care. 2006;29(8):1933–41.
Harber MP, Fry AC, Rubin MR, Smith JC, Weiss LW. Skeletal muscle and hormonal adaptations to circuit weight training in untrained men. Scand J Med Sci Sports. 2004;14(3):176–85.
Márquez G, Romero-Arenas S, Marín-Pagán C, Vera-Ibañez A, Fernandez Del Olmo M, Taube W. Peripheral and central fatigue after high intensity resistance circuit training. Muscle Nerve. 2017;56(1):152–9.
Paoli A, Pacelli QF, Moro T, Marcolin G, Neri M, Battaglia G, et al. Effects of high-intensity circuit training, low-intensity circuit training and endurance training on blood pressure and lipoproteins in middle-aged overweight men. Lipids Health Dis. 2013;12(1):1–8.
Umpierre D, Ribeiro P, Schaan B, Ribeiro J. Volume of supervised exercise training impacts glycaemic control in patients with type 2 diabetes: a systematic review with meta-regression analysis. Diabetologia. 2013;56(2):242–51.
Ibañez J, Izquierdo M, Argüelles I, Forga L, Larrión JL, García-Unciti M, et al. Twice-weekly progressive resistance training decreases abdominal fat and improves insulin sensitivity in older men with type 2 diabetes. Diabetes Care. 2005;28(3):662–7.
Ishii T, Yamakita T, Sato T, Tanaka S, Fujii S. Resistance training improves insulin sensitivity in NIDDM subjects without altering maximal oxygen uptake. Diabetes Care. 1998;21(8):1353–5.
Cooke WH, Carter JR. Strength training does not affect vagal–cardiac control or cardiovagal baroreflex sensitivity in young healthy subjects. Eur J Appl Physiol. 2005;93(5–6):719–25.
Ghanbari Niaki A, Ardeshiri S, AliakbariBaydokhty M, Saeidi A. Effects of circuit resistance training with Crocus sativus supplementation on insulin and estradiol hormones response. Quart Horizon Med Sci. 2016;22(2):125–30.
Gao S, McMillan RP, Zhu Q, Lopaschuk GD, Hulver MW, Butler AA. Therapeutic effects of adropin on glucose tolerance and substrate utilization in diet-induced obese mice with insulin resistance. Molec Metabol. 2015;4(4):310–24.
Magkos F, Tsekouras Y, Kavouras SA, Mittendorfer B, Sidossis LS. Improved insulin sensitivity after a single bout of exercise is curvilinearly related to exercise energy expenditure. Clin Sci. 2008;114(1):59–64.
Wang X, Patterson BW, Smith GI, Kampelman J, Reeds DN, Sullivan SA, et al. A∼ 60-min brisk walk increases insulin-stimulated glucose disposal but has no effect on hepatic and adipose tissue insulin sensitivity in older women. J Appl Physiol. 2013;114(11):1563–8.
Tabata I, Suzuki Y, Fukunaga T, Yokozeki T, Akima H, Funato K. Resistance training affects GLUT-4 content in skeletal muscle of humans after 19 days of head-down bed rest. J Appl Physiol. 1999;86(3):909–14.
Gao S, Ghoshal S, Zhang L, Stevens JR, McCommis KS, Finck BN, et al. The peptide hormone adropin regulates signal transduction pathways controlling hepatic glucose metabolism in a mouse model of diet-induced obesity. J Biol Chem. 2019;294(36):13366–77.
White AT, Schenk S. NAD+/NADH and skeletal muscle mitochondrial adaptations to exercise. Am J Physiol-Endocrinol Metabol. 2012;303(3):E308–E21.
Pesta DH, Goncalves RL, Madiraju AK, Strasser B, Sparks LM. Resistance training to improve type 2 diabetes: working toward a prescription for the future. Nutr Metabol. 2017;14(1):1–10.
Balducci S, Zanuso S, Cardelli P, Salvi L, Bazuro A, Pugliese L, et al. Effect of high-versus low-intensity supervised aerobic and resistance training on modifiable cardiovascular risk factors in type 2 diabetes; the Italian diabetes and exercise study (IDES). PLoS One. 2012;7(11):e49297.
Yang P, Swardfager W, Fernandes D, Laredo S, Tomlinson G, Oh PI, et al. Finding the optimal volume and intensity of resistance training exercise for type 2 diabetes: the FORTE study, a randomized trial. Diabetes Res Clin Pract. 2017;130:98–107.
Kuhla A, Hahn S, Butschkau A, Lange S, Wree A, Vollmar B. Lifelong caloric restriction reprograms hepatic fat metabolism in mice. J Gerontol Ser A: Biomed Sci Med Sci. 2014;69(8):915–22.
Gotshalk LA, Berger RA, Kraemer WJ. Cardiovascular responses to a high-volume continuous circuit resistance training protocol. J Strength Condition Res. 2004;18(4):760–4.
Franklin NC, Robinson AT, Bian J-T, Ali MM, Norkeviciute E, McGinty P, et al. Circuit resistance training attenuates acute exertion-induced reductions in arterial function but not inflammation in obese women. Metab Syndr Relat Disord. 2015;13(5):227–34.
Jasaszwili M, Wojciechowicz T, Billert M, Strowski MZ, Nowak KW, Skrzypski M. Effects of adropin on proliferation and differentiation of 3T3-L1 cells and rat primary preadipocytes. Mol Cell Endocrinol. 2019;496:110532.
Zhang H, Jiang L, Yang Y-J, Ge R-K, Zhou M, Hu H, et al. Aerobic exercise improves endothelial function and serum adropin levels in obese adolescents independent of body weight loss. Sci Rep. 2017;7(1):1–8.
Acknowledgements
The authors would like to thank all the participants who gave us their time and participated in this trial.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest concerning this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rezaeinezhad, N., Alizadeh, R. & Ghanbari-Niaki, A. Short-term circuit resistance training improves insulin resistance probably via increasing circulating Adropin. J Diabetes Metab Disord 21, 583–588 (2022). https://doi.org/10.1007/s40200-022-01020-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-022-01020-4