Abstract
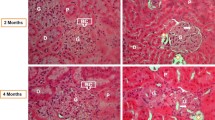
We have investigated how diabetes affects the expression of adropin (ADR) in rat brain, cerebellum, kidneys, heart, liver, and pancreas tissues. The rats in the diabetic group were administered an intraperitoneal (i.p.) injection of a single dose of 60 mg/kg streptozotocin (STZ) dissolved in a 0.1 M phosphate–citrate buffer (pH 4.5). The rats were maintained in standard laboratory conditions in a temperature between 21 and 23 °C and a relative humidity of 70 %, under a 12-h light/dark cycle. The animals were fed a standard commercial pellet diet. After 10 weeks, the animals were sacrified. ADR concentrations in the serum and tissue supernatants were measured by ELISA, and immunohistochemical staining was used to follow the expression of the hormones in the brain, cerebellum, kidneys, heart, liver, and pancreas tissues. The quantities were then compared. Increased ADR immunoreaction was seen in the brain, cerebellum, kidneys, heart, liver, and pancreas in the diabetes-induced rats compared to control subjects. ADR was detected in the brain (vascular area, pia mater, neuroglial cell, and neurons), cerebellum (neuroglial cells, Purkinje cells, vascular areas, and granular layer), kidneys (glomerulus, peritubular interstitial cells, and peritubular capillary endothelial cells), heart (endocardium, myocardium, and epicardium), liver (sinusoidal cells), and pancreas (serous acini). Its concentrations (based on mg/wet weight tissues) in these tissues were measured by using ELISA showed that the levels of ADR were higher in the diabetic rats compared to the control rats. Tissue ADR levels based on mg/wet weight tissues were as follows: Pancreas > liver > kidney > heart > brain > cerebellar tissues. Evidence is presented that shows ADR is expressed in various tissues in the rats and its levels increased in STZ-induced diabetes; however, this effect on the pathophysiology of the disorder remains to be understood.








Similar content being viewed by others
References
Nicholson G, Hall GM (2011) Diabetes mellitus: new drugs for a new epidemic. Br J Anaesth 107:65–73
http://www.who.int/mediacentre/factsheets/fs312/en/. Accessed March 2013
McNay EC, Teske JA, Kotz CM, Dunn-Meynell A, Levin BE, McCrimmon RJ, Sherwin RS (2013) Long-term, intermittent, insulin-induced hypoglycemia produces marked obesity without hyperphagia or insulin resistance: a model for weight gain with intensive insulin therapy. Am J Physiol Endocrinol Metab 304:E131–E138
Aydin S (2013) Role of NUCB2/nesfatin-1 as a possible biomarker. Curr Pharm Des. PMID: 23537082
Aydin S (2010) The presence of the peptides apelin, ghrelin and nesfatin–1 in the human breast milk, and the lowering of their levels in patients with gestational diabetes mellitus. Peptides 31:2236–2240
Kuloglu T, Dabak DO (2009) Determination of ghrelin immunoreactivity in kidney tissues of diabetic rats. Ren Fail 31:562–566
Yang M, Zhang Z, Wang C, Li K, Li S, Boden G, Li L, Yang G (2012) Nesfatin-1 action in the brain increases insulin sensitivity through Akt/AMPK/TORC2 pathway in diet-induced insulin resistance. Diabetes 61:1959–1968
Luo KR, Chao CC, Hsieh PC, Lue JH, Hsieh ST (2012) Effect of glycemic control on sudomotor denervation in type 2 diabetes. Diabetes Care 35:612–616
Sokolovska J, Isajevs S, Sugoka O, Sharipova J, Paramonova N, Isajeva D, Rostoka E, Sjakste T, Kalvinsh I, Sjakste N (2012) Comparison of the effects of glibenclamide on metabolic parameters, GLUT1 expression, and liver injury in rats with severe and mild streptozotocin-induced diabetes mellitus. Medicina (Kaunas) 48:532–543
van de Ven KC, Tack CJ, Heerschap A, van der Graaf M, de Galan BE (2013) Patients with type 1 diabetes exhibit altered cerebral metabolism during hypoglycemia. J Clin Invest 123:623–629
Zhang L, Xiong XQ, Fan ZD, Gan XB, Ago XY, Zhu GQ (2012) Involvement of enhanced cardiac sympathetic afferent reflex in sympathetic activation in early stage of diabetes. J Appl Physiol 113:47–55
Kumar KG, Trevaskis JL, Lam DD, Sutton GM, Koza RA, Chouljenko VN, Kousoulas KG, Rogers PM, Kesterson RA, Thearle M, Ferrante AW Jr, Mynatt RL, Burris TP, Dong JZ, Halem HA, Culler MD, Heisler LK, Stephens JM, Butler AA (2008) Identification of adropin as a secreted factor linking dietary macronutrient intake with energy homeostasis and lipid metabolism. Cell Metab 8:468–481
Ganesh Kumar K, Zhang J, Gao S, Rossi J, McGuinness OP, Halem HH, Culler MD, Mynatt RL, Butler AA (2012) Adropin deficiency is associated with increased adiposity and insulin resistance. Obesity (Silver Spring) 20:1394–1402
Celik E, Yilmaz E, Celik O, Ulas M, Turkcuoglu I, Karaer A, Celik ESimsek Y, Minareci Y, Aydin S (2013) Maternal and fetal adropin levels in gestational diabetes mellitus. J Perinat Med 1–6
Aydin S (2013) Presence of adropin, nesfatin–1, apelin–12, ghrelins and salusins peptides in the milk, cheese whey and plasma of dairy cows. Peptides 43:83–87
Hsu SM, Raine L, Fanger H (1981) Use of avidin–biotin–peroxidase complex (ABC) in immunoperoxidase technique. J Histochem Cytochem 29:577–580
Aydin S, Ozercan IH, Geckil H, Dagli F, Aydin S, Kumru S, Kilic N, Sahin I, Ozercan MR (2007) Ghrelin is present in teeth. J Biochem Mol Biol 40:368–372
Kuloglu T, Aydin S (2013) Immunohistochemical expressions of adropin and inducible nitric oxide synthase in the renal tissues of rats with streptozotocin-induced experimental diabetes. Biotech Histochem (Submitted)
Gutierrez JC, Bahamonde J, Prater MR, Yefi CP, Holladay SD (2010) Production of a type 2 maternal diabetes rodent model using the combination of high-fat diet and moderate dose of streptozocin. Endocr Res 35:59–70
Celik A, Balin M, Kobat MA, Erdem K, Baydas A, Bulut M, Altas Y, Aydin S, Aydin S (2013) Deficiency of a new protein associated with cardiac syndrome X; called adropin. Cardiovasc Ther 3:174–178
Aberg ND, Brywe KG, Isgaard J (2006) Aspects of growth hormone and insulin-like growth factor-I related to neuroprotection, regeneration, and functional plasticity in the adult brain. Sci World J 6:53–80
Liu X, Yao DL, Bondy CA, Brenner M, Hudson LD, Zhou J, Webster HD (1994) Astrocytes express insulin-like growth factor-I (IGF-I) and its binding protein, IGFBP-2, during demyelination induced by experimental autoimmune encephalomyelitis. Mol Cell Neurosci 5:418–430
Aydin S, Dag E, Ozkan Y, Erman F, Dagli AF, Kilic N, Sahin I, Karatas F, Yoldas T, Barim AO, Kendir Y (2009) Nesfatin-1 and ghrelin levels in serum and saliva of epileptic patients: hormonal changes can have a major effect on seizure disorders. Mol Cell Biochem 328:49–56
Oh-I S, Shimizu H, Satoh T, Okada S, Adachi S, Inoue K, Eguchi H, Yamamoto M, Imaki T, Hashimoto K, Tsuchiya T, Monden T, Horiguchi K, Yamada M, Mori M (2006) Identification of nesfatin-1 as a satiety molecule in the hypothalamus. Nature 443:709–712
O’Carroll AM, Selby TL, Palkovits M, Lolait SJ (2000) Distribution of mRNA encoding B78/apj, the rat homologue of the human APJ receptor, and its endogenous ligand apelin in brain and peripheral tissues. Biochim Biophys Acta 1492:72–80
Dagli AF, Aydin S, Karaoglu A, Akpolat N, Ozercan IH, Ozercan MR (2009) Ghrelin expression in normal kidney tissue and renal carcinomas. Pathol Res Pract 205:165–173
Day RT, Cavaglieri RC, Feliers D (2013) Apelin retards the progression of diabetic nephropathy. Am J Physiol Renal Physiol 6:53–80
Hus-Citharel A, Bouby N, Frugière A, Bodineau L, Gasc JM, Llorens-Cortes C (2008) Effect of apelin on glomerular hemodynamic function in the rat kidney. Kidney Int 74:486–494
Sahin I, Aydin S (2012) Serum concentration and kidney expression of salusin-α and salusin-β in rats with metabolic syndrome induced by fructose. Biotech Histochem 88:153–160
Aydin S, Eren MN, Aydin S, Ozercan IH, Dagli AF (2012) The bioactive peptides salusins and apelin-36 are produced in human arterial and venous tissues and the changes of their levels during cardiopulmonary bypass. Peptides 37:233–239
Kleinz MJ, Davenport AP (2004) Immunocytochemical localization of the endogenous vasoactive peptide apelin to human vascular and endocardial endothelial cells. Regul Pept 118:119–125
Kleinz MJ, Skepper JN, Davenport AP (2005) Immunocytochemical localisation of the apelin receptor, APJ, to human cardiomyocytes, vascular smooth muscle and endothelial cells. Regul Pept 126:233–240
Dezaki K, Yada T (2012) Islet β-cell ghrelin signaling for inhibition of insulin secretion. Methods Enzymol 514:317–331
Dun SL, Brailoiu GC, Brailoiu E, Yang J, Chang JK, Dun NJ (2006) Distribution and biological activity of obestatin in the rat. J Endocrinol 191:481–489
Grönberg M, Tsolakis AV, Magnusson L, Janson ET, Saras J (2008) Distribution of obestatin and ghrelin in human tissues: immunoreactive cells in the gastrointestinal tract, pancreas, and mammary glands. J Histochem Cytochem 56:793–801
Drenckhahn D, Mannherz HG (1983) Distribution of actin and the actin-associated proteins myosin, tropomyosin, alpha-actinin, vinculin, and villin in rat and bovine exocrine glands. Eur J Cell Biol 30:167–176
Murakami K, Taniguchi H, Baba S (1982) Presence of insulin-like immunoreactivity and its biosynthesis in rat and human parotid gland. Diabetologia 22:358–361
Murakami K, Taniguchi H, Tamagawa M, Ejiri K, Baba S (1982) Modulation of somatostatin release by endogenous glucagon and insulin: physiological relationship between A, B and D cells in rat pancreatic islets. Endocrinol Jpn 29:503–508
Conflict of interest
The authors have not disclosed any potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aydin, S., Kuloglu, T., Aydin, S. et al. Expression of adropin in rat brain, cerebellum, kidneys, heart, liver, and pancreas in streptozotocin-induced diabetes. Mol Cell Biochem 380, 73–81 (2013). https://doi.org/10.1007/s11010-013-1660-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-013-1660-4