Abstract
Purpose
The present study aimed to verify the clustering of cardiometabolic risk factors for cardiovascular diseases (CVD) and its relationship with the continuous cardiometabolic risk score (cMetS).
Methods
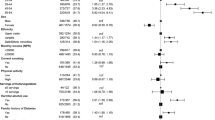
Cross-sectional study with 631 children aged 6 to 9 years. Cardiorespiratory fitness, glucose, systolic blood pressure, total cholesterol/high-density lipoprotein cholesterol ratio, triglycerides, and waist circumference were assessed. The number of children in whom the risk factors were not independently distributed was analyzed. Z-scores were computed for each risk factor to calculate the cMetS.
Results
There was a high proportion of children with clustering of risk factors for CVD. The clustering of risk factors was apparent in 11.3% of the children for four or more risk factors, and 21.9% had three or more risk factors. The cMetS showed a linear relationship with the increase in the number of risk factors. A cMetS value higher than 0.91 indicated clustering of cardiometabolic risk factors amongst children.
Conclusion
The use of clustering of cardiometabolic risk factors identified a high proportion of children with the presence of relevant cardiometabolic alterations. A cMetS value higher than 0.91 (relative to an international standard) indicated higher clustering of cardiometabolic risk factors amongst children.


Similar content being viewed by others
Availability of data and material
Data are available under reasonable request with the corresponding author.
References
Andersen LB, Wedderkopp N, Hansen HS, Cooper AR, Froberg K. Biological cardiovascular risk factors cluster in danish children and adolescents: The European youth heart study. Prev Med (Baltim). 2003;37:363–7. https://doi.org/10.1016/s0091-7435(03)00145-2.
Vanlancker T, Schaubroeck E, Vyncke K, et al. Comparison of definitions for the metabolic syndrome in adolescents. The HELENA study. Eur J Pediatr. 2017;176:241–52. https://doi.org/10.1007/s00431-016-2831-6.
Andersen LB, Lauersen JB, Brønd JC, et al (2015) A new approach to define and diagnose cardiometabolic disorder in children. J Diabetes Res 1–10. https://doi.org/10.1155/2015/539835
Reuter CP, Andersen LB, de Moura Valim AR, Reuter ÉM, Borfe L, Renner JDP, de Mello ED (2019) Cutoff points for continuous metabolic risk score in adolescents from southern Brazil. Am J Hum Biol. https://doi.org/10.1002/ajhb.23211
Stavnsbo M, Skrede T, Aadland E, Aadland KN, Chinapaw M, Anderssen SA, Andersen LB, Resaland GK (2019) Cardiometabolic risk factor levels in Norwegian children compared to international reference values: The ASK study. PLoS One. https://doi.org/10.1371/journal.pone.0220239
IDF (2007) The IDF consensus definition of the Metabolic Syndrome in children and adolescents. https://www.idf.org/e-library/consensus-statements/61-idf-consensus-definition-of-metabolic-syndrome-in-children-and-adolescents.html. Accessed 12 Feb 2021
Reuter CP, Burgos MS, Barbian CD, Renner JDP, Franke SIR, de Mello ED. Comparison between different criteria for metabolic syndrome in schoolchildren from Southern Brazil. Eur J Pediatr. 2018;177:1471–7. https://doi.org/10.1007/s00431-018-3202-2.
Welser L, Lima RA, Silveira JF de C, Andersen LB, Pfeiffer KA, Renner JDP, Reuter CP (2021) Cardiometabolic risk factors in children and adolescents from southern Brazil: comparison to international reference values. J Pediatr Endocrinol Metab. Ahead of Print
Damiani D, Kuba VM, Cominato L, Damiani D, Dichtchekenian V, de Menezes Filho HC. Síndrome metabólica em crianças e adolescentes: Dúvidas na terminologia, mas não nos riscos cardiometabólicos. Arq Bras Endocrinol Metabol. 2011;55:576–82. https://doi.org/10.1590/S0004-27302011000800011.
Andersen LB, Sardinha L, Froberg K, Riddoch CJ, Page AS, Anderssen SA. Fitness, fatness and clustering of cardiovascular risk factors in children from Denmark, Estonia and Portugal: The European Youth Heart Study. Int J Pediatr Obes. 2008;3:58–66. https://doi.org/10.1080/17477160801896366.
Stabelini Neto A, de Campos W, dos Santos GC, Mazzardo Junior O. Metabolic syndrome risk score and time expended in moderate to vigorous physical activity in adolescents. BMC Pediatr. 2014;14:42. https://doi.org/10.1186/1471-2431-14-42.
Andersen LB, Bugge A, Dencker M, Eiberg S, El-Naaman B. The association between physical activity, physical fitness and development of metabolic disorders. Int J Pediatr Obes. 2011;6:29–34. https://doi.org/10.3109/17477166.2011.606816.
Taylor RW, Jones IE, Williams SM, Goulding A. Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3–19 y. Am J Clin Nutr. 2000;72:490–5. https://doi.org/10.1093/ajcn/72.2.490.
Sociedade Brasileira de Cardiologia, Sociedade Brasileira de Hipertensão, Sociedade Brasileira de Nefrologia. VI Diretrizes Brasileiras de Hipertensão. Arq Bras Cardiol. 2010;1:1–51.
PROESP-BR. Projeto Esporte Brasil (2015) Manual de testes e avaliação - Versão 2015. https://www.ufrgs.br/proesp/. Accessed 16 Jan 2016
Bergmann G, Bergmann M, De Castro A, Lorenzi T, Pinheiro E, Moreira R, Marques A, Gaya A (2014) Use of the 6-minute walk/run test to predict peak oxygen uptake in adolescents. Rev Bras Atividade Física Saúde. https://doi.org/10.12820/rbafs.v.19n1p64
Stavnsbo M, Resaland GK, Anderssen SA, et al. Reference values for cardiometabolic risk scores in children and adolescents: Suggesting a common standard. Atherosclerosis. 2018;278:299–306. https://doi.org/10.1016/j.atherosclerosis.2018.10.003.
Altman DG (1991) Theoretical distributions. In: Pract Stat Med Res. London: Chapman & Hall. pp 68–70
Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, Anderssen SA. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study). Lancet. 2006;368:299–304. https://doi.org/10.1016/S0140-6736(06)69075-2.
Machado-Rodrigues AM, Leite N, Coelho-E-Silva MJ, Martins RA, Valente-Dos-Santos J, Mascarenhas LPG, Boguszewski MCS, Padez C, Malina RM. Independent association of clustered metabolic risk factors with cardiorespiratory fitness in youth aged 11–17 years. Ann Hum Biol. 2014;41:271–6. https://doi.org/10.3109/03014460.2013.856471.
Marques KC, de C Silveira JF, Schneiders LDB, Souza S, de Mello ED, Reuter CP. Escore contínuo de risco metabólico em escolares com diferentes níveis de aptidão cardiorrespiratória. Rev Andaluza Med del Deport. 2019;12:354–7.
Saldanha Filho N, Reuter CP, Renner JDP, Barbian CD, de C Silveira JF, de BorbaSchneiders L, Pohl HH. Low levels of cardiorespiratory fitness and abdominal resistance are associated with metabolic risk in schoolchildren. J Pediatr Endocrinol Metab. 2019;32:455–60. https://doi.org/10.1515/jpem-2018-0236.
Silveira JF de C, Reuter CP, Welser L, Pfeiffer KA, Andersen LB, Pohl HH, Lima RA (2021) Tracking of cardiometabolic risk in a Brazilian schoolchildren cohort: a 3-year longitudinal study. J Sports Med Phys Fitness. https://doi.org/10.23736/S0022-4707.20.11479-8
Kennedy AB, Lavie CJ, Blair SN. Fitness or fatness which is more important? JAMA - J Am Med Assoc. 2018;319:231–2. https://doi.org/10.1001/jama.2017.21649.
Lerum Ø, Aadland E, Andersen LB, Anderssen SA, Resaland GK. Validity of noninvasive composite scores to assess cardiovascular risk in 10-year-old children. Scand J Med Sci Sport. 2017;27:865–72. https://doi.org/10.1111/sms.12826.
Viitasalo A, Lakka TA, Laaksonen DE, et al. Validation of metabolic syndrome score by confirmatory factor analysis in children and adults and prediction of cardiometabolic outcomes in adults. Diabetologia. 2014;57:940–9. https://doi.org/10.1007/s00125-014-3172-5.
Eisenmann JC. On the use of a continuous metabolic syndrome score in pediatric research. Cardiovasc Diabetol. 2008;7:17. https://doi.org/10.1186/1475-2840-7-17.
Eisenmann JC, Laurson KR, Dubose KD, Smith BK, Donnelly JE. Construct validity of a continuous metabolic syndrome score in children. Diabetol Metab Syndr. 2010;2:8. https://doi.org/10.1186/1758-5996-2-8.
Okosun IS, Lyn R, Davis-Smith M, Eriksen M, Seale P. Validity of a continuous metabolic risk score as an index for modeling metabolic syndrome in adolescents. Ann Epidemiol. 2010;20:843–51. https://doi.org/10.1016/j.annepidem.2010.08.001.
Villa JKD, Silva ARE, Santos TSS, Ribeiro AQ, Sant’Ana LFDR. Risco de síndrome metabólica em crianças: uso de um escore único. Rev Paul Pediatr. 2015;33:187–93. https://doi.org/10.1016/j.rpped.2014.11.001.
Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: Findings from the third national health and nutrition examination survey, 1988–1994. Arch Pediatr Adolesc Med. 2003;157:821–7. https://doi.org/10.1001/archpedi.157.8.821.
Weiss R, Bremer AA, Lustig RH. What is metabolic syndrome, and why are children getting it? Ann N Y Acad Sci. 2013;1281:123–40. https://doi.org/10.1111/nyas.12030.
Ragland DR. Dichotomizing continuous outcome variables: Dependence of the magnitude of association and statistical power on the cutpoint. Epidemiology. 1992;3:434–40. https://doi.org/10.1097/00001648-199209000-00009.
Bakhshi E, McArdle B, Mohammad K, Seifi B, Biglarian A (2012) Let continuous outcome variables remain continuous. Comput Math Methods Med 1–13. https://doi.org/10.1155/2012/639124
Funding
The present study did not receive funding resources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Committee of Ethics in Research with Human Subjects of the University of Santa Cruz do Sul (UNISC), under number 37338314.6.0000.5343.
Consent to participate and for publication
All parents or guardians were informed about the study objectives and signed informed consent.
Conflicts of interest
The authors state no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Reuter, C.P., Renner, J.D.P., de Castro Silveira, J.F. et al. Clustering of cardiometabolic risk factors and the continuous cardiometabolic risk score in children from Southern Brazil: a cross-sectional study. J Diabetes Metab Disord 20, 1221–1228 (2021). https://doi.org/10.1007/s40200-021-00845-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00845-9