Abstract
Objective
The present study aims to verify the odds of remaining with the clustering of 3 or more, 4 or more, and 5 or more risk factors across a 2-year time span.
Methods
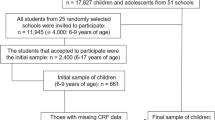
Observational longitudinal study that included 358 children and adolescents (10.96 ± 2.28 years of age at baseline). Cardiorespiratory fitness, glucose, systolic blood pressure, total cholesterol/high-density lipoprotein cholesterol ratio, triglycerides, and waist circumference were assessed. The number of children in whom the risk factors were not independently distributed was analyzed. Odds ratios of presenting n risk factors clustered at follow-up according to the number of risk factors observed at baseline were calculated.
Results
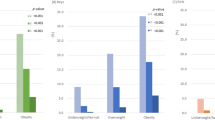
More participants than expected were found presenting clustering of 4 or more and 5 or more risk factors at both baseline (11.7% and 5.6%, respectively) and follow-up (9.5% and 5.6%, respectively). The odds ratios calculated demonstrated that the odds of presenting the same number of risk factors clustered or more at follow-up increased according to the number of risk factors clustered at baseline.
Conclusion
The higher the number of risk factors a child had at baseline, the higher the odds of presenting the same number of risk factors or more after two years of follow-up.



Similar content being viewed by others
Data availability
Data are available under reasonable request with the corresponding author.
References
WHO. Noncommunicable diseases progress monitor 2022. 2022. https://www.who.int/publications/i/item/9789240047761. Accessed 12 Sep 2022.
Chung ST, Onuzuruike AU, Magge SN. Cardiometabolic risk in obese children. Ann N Y Acad Sci. 2018;1411:166–83.
Martinez SM, Blanco E, Burrows R, Lozoff B, Gahagan S. Mechanisms linking childhood weight status to metabolic risk in adolescence. Pediatr Diabetes. 2020;21:203–9.
Reuter CP, Renner JDP, de Castro Silveira JF, da Silva PT, Lima RA, Pfeiffer KA, et al. Clustering of cardiometabolic risk factors and the continuous cardiometabolic risk score in children from southern Brazil: a cross-sectional study. J Diabetes Metab Disord. 2021;20:1221–8.
Welser L, Lima RA, Silveira JF de C, Andersen LB, Pfeiffer KA, Renner JDP, et al. Cardiometabolic risk factors in children and adolescents from southern Brazil: comparison to international reference values. J Pediatr Endocrinol Metab 2021;34:1237–1246.
Andersen LB, Lauersen JB, Brønd JC, Anderssen SA, Sardinha LB, Steene-Johannessen J, et al. A new approach to define and diagnose Cardiometabolic disorder in children. J Diabetes Res. 2015:1–10.
Delgado Floody P, Martínez Salazar C, Caamaño Navarrete F, Jerez Mayorga D, Osorio Poblete A, García Pinillos F, et al. Insatisfacción con la imagen corporal y su relación con el estado nutricional, riesgo cardiometabólico y capacidad cardiorrespiratoria en niños pertenecientes a centros educativos públicos. Nutr Hosp. 2017;34:1044–9.
Pogodina A, Rychkova L, Kravtzova O, Klimkina J, Kosovtzeva A. Cardiometabolic risk factors and health-related quality of life in adolescents with obesity. Child Obes. 2017;13:499–506.
Kelishadi R, Mirmoghtadaee P, Najafi H, Keikha M. Systematic review on the association of abdominal obesity in children and adolescents with cardio-metabolic risk factors. J Res Med Sci. 2015;20:294–307.
Palhares HM da C, da Silva AP, Resende DCS, Pereira G de A, Rodrigues-Júnior V, Borges M de F. Evaluation of clinical and laboratory markers of cardiometabolic risk in overweight and obese children and adolescents. Clinics. 2017;72:36–43.
Saldanha Filho N, Reuter CP, Renner JDP, Barbian CD, De Castro Silveira JF, De Borba SL, et al. Low levels of cardiorespiratory fitness and abdominal resistance are associated with metabolic risk in schoolchildren. J Pediatr Endocrinol Metab. 2019;32:455–60.
Saldanha Filho N, Reuter CP, Silveira JF de C, Borfe L, Renner JDP, Pohl HH. Low performance-related physical fitness levels are associated with clustered cardiometabolic risk score in schoolchildren: a cross-sectional study. Hum Mov 2022;23:113–119.
Bugge A, El-Naaman B, Mcmurray RG, Froberg K, Andersen LB. Tracking of clustered cardiovascular disease risk factors from childhood to adolescence. Pediatr Res. 2013;73:245–9.
Camhi SM, Katzmarzyk PT. Tracking of cardiometabolic risk factor clustering from childhood to adulthood. Int J Pediatr Obes. 2010;5:122–9.
Laitinen T, Laitinen TT, Pahkala K, Magnussen CG, Viikari JSA, Oikonen M, et al. Ideal cardiovascular health in childhood and cardiometabolic outcomes in adulthood: the cardiovascular risk in young finns study. Circulation. 2012;125:1971–8.
Silveira JF, Reuter CP, Welser L, Pfeiffer KA, Andersen LB, Pohl HH, et al. Tracking of cardiometabolic risk in a Brazilian schoolchildren cohort: a 3-year longitudinal study. J Sports Med Phys Fitness. 2021;61.
Daniels SR, Pratt CA, Hayman LL. Reduction of risk for cardiovascular disease in children and adolescents. Circulation. 2011;124:1673–86.
Tanrikulu MA, Agirbasli M, Berenson G. Primordial prevention of cardiometabolic risk in childhood. Adv Exp Med Biol. 2017;956:489–96.
Ruiz LD, Zuelch ML, Dimitratos SM, Scherr RE. Adolescent obesity: diet quality, psychosocial health, and cardiometabolic risk factors. Nutrients. 2020;12.
Halfon N, Verhoef PA, Kuo AA. Childhood antecedents to adult cardiovascular disease. Pediatr Rev. 2012;33:51–61.
SurveyMonkey. Sample size calculator. https://www.surveymonkey.com/mp/sample-size-calculator/.
Taylor RW, Jones IE, Williams SM, Goulding A. Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3–19 y. Am J Clin Nutr. 2000;72:490–5.
SBC, SBH, SBN. VI Diretrizes Brasileiras de Hipertensão. Arq Bras Cardiol 2010;1 Suppl. 1:1–51.
PROESP-BR. Manual de testes e avaliação. 2012. https://www.ufrgs.br/proesp/.
Altman DG. Theoretical distributions. In: Practical statistics for medical research. London: Chapman & Hall; 1991. p. 68–70.
Cumming G. Understanding the new statistics - effect sizes, confidence intervals, and meta-analysis. New York: Routledge; 2012.
Field A. Discovering statistics using IBM SPSS statistics. 5th ed. London: SAGE; 2017.
Buchan DS, Boddy LM, Young JD, Cooper SM, Noakes TD, Mahoney C, et al. Relationships between cardiorespiratory and muscular fitness with Cardiometabolic risk in adolescents. Res Sports Med. 2015;23:227–39.
Reuter CP, Burgos MS, Barbian CD, Renner JDP, Franke SIR, de Mello ED. Comparison between different criteria for metabolic syndrome in schoolchildren from southern Brazil. Eur J Pediatr. 2018;177:1471–7.
Lavie CJ, De Schutter A, Parto P, Jahangir E, Kokkinos P, Ortega FB, et al. Obesity and prevalence of cardiovascular diseases and prognosis-the obesity paradox updated. Prog Cardiovasc Dis. 2016;58:537–47.
García-Hermoso A, Ramírez-Vélez R, Garciá-Alonso Y, Alonso-Martínez AM, Izquierdo M. Association of Cardiorespiratory Fitness Levels during youth with health risk later in life: A systematic review and Meta-analysis. JAMA Pediatr. 2020;174:952–60.
Mintjens S, Menting MD, Daams JG, van Poppel MNM, Roseboom TJ, Gemke RJBJ. Cardiorespiratory fitness in childhood and adolescence affects future cardiovascular risk factors: A systematic review of longitudinal studies. Sports Med. 2018;48:2577–605.
Umer A, Kelley GA, Cottrell LE, Giacobbi P, Innes KE, Lilly CL. Childhood obesity and adult cardiovascular disease risk factors: A systematic review with meta-analysis. BMC Public Health. 2017;17.
Lima RA, Bugge A, Ersbøll AK, Stodden DF, Andersen LB. The longitudinal relationship between motor competence and measures of fatness and fitness from childhood into adolescence. J Pediatr. 2019;95:482–8.
Reuter CP, Brand C, Silveira JF de C, de Borba Schneiders L, Renner JDP, Borfe L, et al. Reciprocal longitudinal relationship between fitness, fatness, and metabolic syndrome in Brazilian children and adolescents: A 3-year longitudinal study. Pediatr Exerc Sci 2021;33:74–81.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. J Am Coll Cardiol. 2020;76:2982–3021.
Muka T, Imo D, Jaspers L, Colpani V, Chaker L, van der Lee SJ, et al. The global impact of non-communicable diseases on healthcare spending and national income: a systematic review. Eur J Epidemiol. 2015;30:251–77.
Andersen LB, Sardinha L, Froberg K, Riddoch CJ, Page AS, Anderssen SA. Fitness, fatness and clustering of cardiovascular risk factors in children from Denmark, Estonia and Portugal: the European youth heart study. Int J Pediatr Obes. 2008;3(Suppl.1):58–66.
Suglia SF, Koenen KC, Boynton-Jarrett R, Chan PS, Clark CJ, Danese A, et al. Childhood and adolescent adversity and Cardiometabolic outcomes: A scientific statement from the American Heart Association. Circulation. 2018;137:15–28.
Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas. 2011;70:266–84.
García-Hermoso A, Agostinis-Sobrinho C, Mota J, Santos RM, Correa-Bautista JE, Ramírez-Vélez R. Adiposity as a full mediator of the influence of cardiorespiratory fitness and inflammation in schoolchildren: the FUPRECOL study. Nutr Metab Cardiovasc Dis. 2017;27:525–33.
Sun C, Magnussen CG, Ponsonby AL, Schmidt MD, Carlin JB, Huynh Q, et al. The contribution of childhood cardiorespiratory fitness and adiposity to inflammation in young adults. Obesity. 2014;22:2598–605.
Wedell-Neergaard AS, Eriksen L, Grønbæk M, Pedersen BK, Krogh-Madsen R, Tolstrup J. Low fitness is associated with abdominal adiposity and low-grade inflammation independent of BMI. PLoS One. 2018;13.
Lima RA, Andersen LB, Soares FC, Kriemler S. The causal pathway effects of a physical activity intervention on adiposity in children: the KISS study cluster randomized clinical trial. Scand J Med Sci Sports. 2020;30:1685–91.
García-Hermoso A, Ramírez-Vélez R, Saavedra JM. Exercise, health outcomes, and pædiatric obesity: A systematic review of meta-analyses. J Sci Med Sport. 2019;22:76–84.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–62.
Chaput JP, Willumsen J, Bull F, Chou R, Ekelund U, Firth J, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: summary of the evidence. Int J Behav Nutr Phys Act. 2020;17:141.
AAP. American Academy of Pediatrics. Children, adolescents, and television. Pediatrics. 2001;107:423–6.
Quist JS, Sjödin A, Chaput JP, Hjorth MF. Sleep and cardiometabolic risk in children and adolescents. Sleep Med Rev. 2016;29:76–100.
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1:40–3.
Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA - Journal of the American Medical Association. 2014;311:1778–86.
Stavnsbo M, Resaland GK, Anderssen SA, Steene-Johannessen J, Domazet SL, Skrede T, et al. Reference values for cardiometabolic risk scores in children and adolescents: suggesting a common standard. Atherosclerosis. 2018;278:299–306.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Committee of Ethics in Research with Human Subjects of the University of Santa Cruz do Sul (UNISC), under number 714.216.
Consent to participate and for publication
All parents or guardians were informed about the study objectives and signed informed consent.
Competing interests
The authors state no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 225 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Castro Silveira, J.F., Sehn, A.P., da Silva, L. et al. The stability of cardiometabolic risk factors clustering in children and adolescents: a 2-year longitudinal study. J Diabetes Metab Disord 22, 529–538 (2023). https://doi.org/10.1007/s40200-022-01174-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-022-01174-1