Abstract
Introduction
This study was performed to compare the optical performance of a multizonal presbyopia-correcting intraocular lens (IOL) and a conventional trifocal model.
Methods
The optical quality and simulated visual acuity (VA) of 570 Precizon Presbyopic NVA (OPHTEC BV) and AcrySof IQ PanOptix (Alcon) were compared. The Precizon features a refractive design consisting of alternating optical zones that converge the incident light into two principal foci and a transitional zone for intermediate vision. By contrast, the PanOptix applies a diffractive (non-apodized) profile to achieve trifocality. Simulated VA was derived from the modulation transfer function. Chromatic aberration effects were also studied.
Results
The diffractive and multizonal-refractive lenses yielded comparable simulated VAs at far focus (0.00 logMAR). All curves showed a reduction in expected VA with an increase in negative defocus. At − 1.0 D, the multizonal-refractive IOL's VA dropped by 0.05 logMAR, but for the diffractive model, it was one line (0.11 logMAR). The multizonal-refractive lens's VA prediction at the secondary peak was 0.03 logMAR—minimally better than the 0.06 logMAR of the diffractive lens at − 2.5 D. The refractive lens exhibited a 24% decrease in polychromatic optical quality due to material dispersion. The performance of PanOptix was more substantially affected, showing a 44% loss at 50 lp/mm at far, with minimal effects at other distances.
Conclusion
The multizonal-refractive lens does not fall short of the established trifocal IOL, and it can be used to extend the visual range of pseudophakic patients. Although the multizonal-refractive lens has lower material dispersion, the diffractive model corrects chromatism beyond far focus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Multizonal-refractive intraocular lenses (IOLs) are reported to increase the postoperative visual range, especially when compared to bifocal devices. A multizonal-refractive lens might also be an effective substitute for a trifocal method, but this hypothesis has not yet been tested in a clinical or laboratory setting. |
It is essential to measure the effect of chromatic aberration on the imaging quality since it may vary between different types of IOLs. |
What was learned from the study? |
The multizonal-refractive design appears to produce a comparable optical performance to a standard trifocal lens at an extended range of focus. |
The chromatic aberration of the diffractive lens increased at the far point but was compensated for at other distances. By contrast, the multizonal IOL's optical performance was slightly impacted by longitudinal chromatic aberration over the measured defocus range. |
Introduction
Multifocal intraocular lens (IOL) design is continuously evolving in order to improve visual quality, achieve spectacle independence and increase patient satisfaction after cataract surgery [1, 2]. Typically, these IOLs have been developed using different optical principles; there are currently two main types of multifocal optics in IOLs: diffractive and refractive. Although good binocular vision is often achieved in patients following multifocal IOL implantations, some limitations have also been described for different models [3]. Photic phenomena are among the main complaints of patients with multifocal IOLs. Due to light scattering at diffractive steps, multifocal IOLs featuring diffractive optics appear to be more prone to inducing glare symptoms than refractive-multifocal IOLs [4]. On the other hand, near vision tends to depend more on pupil size when using refractive IOLs with a concentrically allocated near-focus zone [5]. Furthermore, the multizonal IOL design may lead to a loss of contrast sensitivity associated with the distribution of the total available light between several focal points [3]. While clinical studies have found better contrast sensitivity after the implantation of diffractive IOLs rather than refractive ones, some authors have disagreed with these findings and reached the opposite conclusions [6, 7]. The limitations of concentric-refractive technology may be addressed by the introduction of a multi-segmented approach with alternating focal zones. Laboratory research suggests that using segments instead of concentric rings ought to provide better optical quality [8] with minimal photic phenomena observed clinically [9].
In vivo studies have reported that diffractive-refractive trifocal IOLs expand the postoperative visual range, resulting in a high rate of spectacle freedom and patient satisfaction [10, 11]. Although the multizonal-refractive lens may also be a viable alternative to a trifocal approach, this conjecture has yet to be verified in both clinical and laboratory settings.
Benchtop measurements are often performed by evaluating image quality from the light distribution and efficiency of various foci [12]. The International Organization for Standardization (ISO-11979-2) recommends using monochromatic green light for the optical testing of multifocal IOLs [13]. However, this monochromatic light may be insufficient to extrapolate the visual performance since routine visual tasks are performed in light composed of various wavelengths. Therefore, polychromatic light testing appears more representative of real-life conditions and, as demonstrated recently, provides good agreement with clinical metrics [14].
The purpose of this study was to comprehensively evaluate the performance of the multizonal-refractive IOL and compare it to a conventional trifocal-lens model using optical-quality metrics derived from benchtop measurements in polychromatic light. The secondary objective was to quantify the impact of chromatic aberration on the IOLs’ imaging quality.
Methods
Intraocular Lenses
The following IOL models were investigated in this study: 570 Precizon Presbyopic NVA—a multizonal-refractive IOL, and AcrySof IQ PanOptix—a hybrid-diffractive trifocal IOL. Two lenses of each model were available for testing, each with the same refractive power of 20.0 diopters (D).
The 570 Precizon Presbyopic NVA (OPHTEC BV, Groningen, The Netherlands) is manufactured from hydroxyethyl methacrylate (HEMA) copolymerized with ethoxyethyl methacrylate (EOEMA). This hybrid hydrophobic-hydrophilic material has a refractive index of 1.46 and Abbe number of 47. It features an aspheric surface to compensate for positive spherical aberration (SA) of the cornea by 0.11 µm. The lens has a refractive design consisting of alternating optical zones, which converge the incident light into two principal foci, and 'continuous transitional focus' for intermediate vision. The Precizon's most prominent (central) zone is dedicated to far vision, and the near power is set at + 2.75 D (IOL plane). The lens deliberately lacks rotational symmetry as it has an uneven distribution of 11 refractive zones along the horizontal and vertical meridians.
The PanOptix (Alcon Inc., Fort Worth, TX, USA) is a refractive-diffractive trifocal lens made of hydrophobic AcrySof material with a refractive index of 1.55 and an Abbe number of 37. This lens has a 4.5-mm (non-apodized) diffractive structure in the lens center and a 1.5-mm refractive zone located at the lens periphery. The PanOptix converges half of the light to far and a quarter to each remaining focus. The lens has an intermediate and near ADD power of 2.17 D and 3.25 D (IOL plane), respectively, as well as an aspherical design yielding − 0.10 μm of SA.
Optical Setup and Metrics
The optical quality of the study IOLs was assessed using the OptiSpheric IOL PRO2 optical bench (Trioptics GmbH, Wedel, Germany), following the guidelines of the International Standard Organization using monochromatic (546 nm) light [13]. In addition, the optical quality was assessed in polychromatic light to study the impact of longitudinal chromatic aberration (LCA) on the optical quality. A model cornea with a positive SA of 0.28 m at 5.15 mm and 1 D of LCA was used for the measurements [15].
The LCA of the IOLs was obtained from the difference between the IOL's power measured in red (644 nm) and blue (480 nm) light without the corneal model and expressed in diopters according to the formula
The IOLs’ imaging performance was evaluated for an aperture size of 3 mm (photopic) and 4.5 mm (scotopic). The modulation transfer function (MTF) of each IOL placed in the model eye was measured at its best focus plane using a 50 lp/mm MTF criterion; the IOL's tolerance for defocus was then examined within the range of + 0.5 D to − 3.5 D at the spectacle plane. Since the multizonal lens lacks rotational symmetry, care was taken to ensure the reproducibility of the IOL position during testing. Figure S1 in the Supplementary Information visualizes the locations of the sagittal and tangential meridians and provides a schematic drawing of the IOL. The two meridians were, however, averaged for the analysis, given that all meridians, rather than a specific one, contribute to the retinal image formation. A comparison between the sagittal and tangential MTFs of the multizonal and diffractive IOL is presented in Fig. S2 in the Supplementary Information, which also confirms that there is good alignment of the meridians in the refractive-diffractive model.
Furthermore, the optical quality was also evaluated with the area under the MTF (MTFa), given its significance to visual quality [16]. The MTFa, which was obtained by integrating the corresponding MTF values at a range of spatial frequencies from 1 to 50 lp/mm, was converted to simulated visual acuity (simVA) as described by Alarcon et al. [16]. This article is based on bench evaluations and does not contain any studies with human participants or animals performed by any of the authors.
Results
Chromatic Aberration
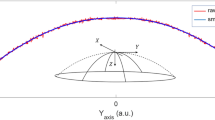
Figure 1 shows the chromatic focus shift centered at 546 nm for 3-mm and 4.5-mm apertures. The chromatic focus shift was measured at 480 nm and 644 nm, and the LCA results are presented in Table 1. The multizonal lens demonstrated lower far-point dispersion effects than the diffractive one at 3 mm (Fig. 1A). Aperture enlargement to 4.5 mm resulted in a − 0.03 D (multizonal) to 0.04 D (diffractive) LCA change (Fig. 1B) and increased the standard deviation, indicating a higher measurement uncertainty (Table 1).
The longitudinal chromatic aberration (LCA) of the multizonal-refractive (black line) and hybrid-diffractive (blue line) IOLs measured at 3-mm (A) and 4.5-mm (B) apertures. The solid line indicates the second-order polynomial fit. The multizonal-refractive and hybrid-diffractive IOLs used were 570 Precizon Presbyopic NVA and AcrySof IQ PanOptix IOLs, respectively
Monochromatic vs. Polychromatic Optical Quality
The MTF curves derived at the best focus for monochromatic and polychromatic conditions and with 3-mm and 4.5-mm apertures are compared in Fig. 2 and Table 2. With an aperture of 3 mm, the multizonal lens demonstrated a 24% MTF decrease at 50 lp/mm due to dispersion effects (Fig. 2A). However, the diffractive lens's performance was more substantially affected, with a loss of 44% (Fig. 2C). An aperture increase to 4.5 mm resulted in reduced MTFs for both models, but the impact of LCA on the optical quality remained comparable (Fig. 2B, D). The MTF loss was 18% for the multizonal lens and 42% for the diffractive one.
Modulation transfer function (MTF) levels of the studied IOLs at the best far focus compared for each measurement condition. The MTF of the multizonal-refractive lens was measured in monochromatic (545 nm, green line) and polychromatic (black line) light at 3 mm (A) and 4.5 mm (B). The MTF of the hybrid-diffractive lens was measured in monochromatic and polychromatic light at 3 mm (C) and 4.5 mm (D). Two samples per model were measured: the dotted lines show the values of each lens separately; the solid lines refer to the average of two samples of the same IOL model. The multizonal-refractive and hybrid-diffractive lenses used were 570 Precizon Presbyopic NVA and AcrySof IQ PanOptix IOLs, respectively. Poly polychromatic light
Figure 3 reports the MTFa comparison between the two spectral conditions at the studied defocus range for both models at 3-mm and 4.5-mm apertures. The MTFa, a multi-frequency metric, appeared less affected by LCA than the (single) 50 lp/mm MTF value. At 3 mm, the multizonal lens's MTF reduction was 7% at the far focus, close to the 8% recorded at −2 D, confirming that there were similar LCA effects across the defocus range (Fig. 3A). The diffractive lens demonstrated a loss of 16% at the far focus, but in the intermediate and near range, the monochromatic and polychromatic curves nearly overlapped, indicating an LCA correction due to diffractive optics at the secondary foci (Fig. 3C). Chromatic dispersion appears to minimally increase the MTFa at −1 D for both IOLs and to minimally expand the near range of the diffractive model. The analysis at 4.5 mm shown in Fig. 3B, D demonstrates a similar trend, with a marginal increase in the MTFa difference between the green and polychromatic conditions for the far (8.6%) and secondary (9.4%) foci of the multizonal model. For the diffractive lens, it was minimally lower than for the photopic pupil (i.e., MTFa loss = 14%), also showing the close correspondance between monochromatic and polychromatic perforamce at higher defocus values.
The area under the modulation transfer function (MTFa) values for the two IOL models measured at a spectacle defocus range of + 0.5 D to − 3.5 D. The MTFa of the multizonal-refractive lens was measured in monochromatic (545 nm, green line) and polychromatic (black line) light at 3 mm (A) and 4.5 mm (B). The MTFa of the hybrid-diffractive lens was measured in monochromatic and polychromatic light at 3 mm (C) and 4.5 mm (D). Two samples per model were measured: the dotted lines show each lens's values separately; the solid lines refer to the average of two samples. The multizonal-refractive and hybrid-diffractive lenses used were 570 Precizon Presbyopic NVA and AcrySof IQ PanOptix IOLs, respectively. Poly polychromatic light
Figure 4 presents USAF-target images recorded at the best (green) far focus for three wavelengths and in polychromatic light. The quality of the photographs taken with the diffractive lens at 644 nm (red) and 480 nm (blue) was clearly affected by optical blur compared to that at 546 nm (green), especially in red light due to the larger spectral difference. Chromatic effects were also observed with the multizonal lens; however, they were less pronounced, confirming that its material has a lower LCA level.
Resolution target photographs taken through the studied IOLs. A simulation of an RGB image and a direct camera recording of an unprocessed (polychromatic) test chart are presented for comparison. The multizonal and diffractive lenses used were 570 Precizon Presbyopic NVA and AcrySof IQ PanOptix IOLs, respectively
Multizonal vs. Diffractive Technology
The average MTF curves of the multizonal and diffractive IOLs measured for 3- and 4.5-mm apertures at best far, intermediate, and near foci are shown in Fig. 5. At the far point (Fig. 5A, D), the analysis shows comparable polychromatic performance of the two models at both pupil sizes, with minimally improved low-spatial-frequency levels (up to 20 lp/mm) of the diffractive lens. In the intermediate range (Fig. 5B, E), the MTF of the diffractive lens was slightly higher than that of the multizonal lens; however, this was reversed at near (Fig. 4C and 5F).
The polychromatic MTF levels at the far, intermediate, and near foci of the hybrid-diffractive (blue lines) and the multizonal-refractive (black lines) IOLs at 3 mm (A–C) and 4.5 mm (D–F). Two samples per model were measured: the dotted lines show the values of each lens separately; the solid lines refer to the average of two samples. The multizonal-refractive and hybrid-diffractive IOLs used were 570 Precizon Presbyopic NVA and AcrySof IQ PanOptix IOLs, respectively. IOL intraocular lens, MTF modulation transfer function
To investigate the simulated defocus curves of the two study lenses, we used the logMAR VA prediction (Fig. 6), which was derived from the MTFa according to the empirical model, as described in the “Methods” section. The diffractive and the multizonal-refractive IOLs yielded comparable VA at far focus (0.00 logMAR). All curves showed a reduction in VA with an increase in negative defocus. At − 1.0 D, the simulated VA of the refractive IOL dropped by 0.05 logMAR, but for the diffractive lens, it was one line (0.11 logMAR). The VA prediction for the multizonal lens at the secondary peak was 0.03 logMAR—minimally better than the 0.06 logMAR for the diffractive lens at − 2.5 D.
Simulated logMAR visual acuity (VA) of the hybrid-diffractive (blue lines) and multizonal-refractive (black lines) IOLs measured in the defocus range from + 0.5 D to − 3.5 D (spectacle plane). Two samples per model were measured: the dotted lines show each lens's values separately; the solid lines refer to the average of two samples. The multizonal-refractive and hybrid-diffractive IOLs used were 570 Precizon Presbyopic NVA and AcrySof IQ PanOptix IOLs, respectively
The resolution-test images shown in Fig. 7 agree, in general, with the numerical results. However, astigmatic-like image deterioration can be seen in the multizonal model photographs, with slightly different projections of the vertical and horizontal bars of the test, which is particularly evident at − 3 D and for the photopic (3 mm) pupil.
Discussion
This study demonstrates that, according to the MTF analysis, the multizonal-refractive approach does not fall short of the established trifocal IOL and can be used to extend the visual range of pseudophakic patients. Although the performance of both models was affected by LCA, the HEMA/EOEMA material had a lower LCA level than AcrySof. The diffractive model, however, showed a reduction in dispersion effects at its secondary foci.
The chromatic aberration of the phakic eye is caused by ocular-media light dispersion, with the cornea and the crystalline lens being the most significant contributors [17]. Following phacoemulsification and IOL implantation, the amount of chromatic aberration is reduced compared to a phakic eye [18], which shows variability between IOL models. One differentiating factor is the spectral dispersion of biomaterials, which show varying levels of wavelength dependency for their refractive indices [19]. Another important factor is lens design, as the effects of chromatic aberration can be corrected through the diffractive principle [15, 20]. Therefore, both the IOL material and the design may affect the pseudophakic eye's chromatic aberration, which, in turn, may compromise the polychromatic optical quality [15, 20].
The impact of chromatic aberration for different types of IOLs has been extensively studied, both in vivo and in vitro [18, 21,22,23]. Pérez-Merino et al. used a laser ray tracing aberrometer to measure the optical aberrations at wavelengths of 532 nm and 785 nm [21]. They measured the chromatic difference of focus in nine eyes with the Tecnis (Abbe value 55) IOLs and nine eyes with the Acrysof (Abbe value 37) IOL and reported a significantly lower chromatic difference of focus value for Tecnis than for Acrysof (0.46 D and 0.75 D, respectively) [21]. Siedlecki et al. measured the objective refraction at various wavelengths (470–660 nm) and used an adapted visual refractometer to evaluate the variation of the chromatic difference of refraction with the IOL material. That study reported that the properties of IOL biomaterials have a significant influence on the magnitude of the chromatic aberration of the pseudophakic eye [23], which was also seen in the current study. Loicq et al. presented a bench study comparing the through-focus MTFs of nine lenses at different wavelengths of 480 nm, 546 nm, and 650 nm. They found that for non-zero diffractive orders, the refractive LCA contributions may be compensated by the reversed LCA of a diffractive element, with the efficiency dependent on the material and optical design [22].
Our in vitro measurements of LCA for AcrySof IOL (0.91 ± 0.01 D) fall within the LCA range reported by Millan et al. using an autorefractor with a Scheiner disc illuminated by different wavelengths (0.96 ± 0.34 D) [18]. Additionally, that study showed that the Tecnis IOL had a lower level of LCA than the AcrySof IOL, which is consistent with the IOL material's dispersive characteristics, since lower LCA values have been reported for materials featuring higher Abbe numbers. This conclusion also holds for our result, since the multizone HEMA/EOEMA IOL (Abbe value 47) had lower LCA values (0.41 D) than the diffractive AcrySof IOL [18].
As a consequence of the LCA, the MTF values were significantly lower when measured under polychromatic illumination than those measured with monochromatic light. Our results show that the polychromatic MTF of the multizonal lens (24%) decreased less than that of the diffractive model (44%) at far. The material properties may be one factor, as the diffractive lens has a lower Abbe number and thus higher chromatic aberration than the multizonal lens [24]. However, at the secondary foci, chromatic effects were minimized by the lens's diffractive design at the intermediate and near foci [15, 20]. Therefore, as shown in Fig. 3, the LCA correction was more effective in the latter position. This finding agrees with the conclusions of Loicq et al. [22], who also demonstrated a nearly-zero LCA contribution of the diffractive lens at the intermediate focus. In addition, the negative LCA at the near focus reported by Loicq et al. reduces the eye's LCA, which may explain the minimal differences between the monochromatic and polychromatic performance of the diffractive lens at about − 2.5 D. This correction can take place because refractive and diffractive optical elements yield LCAs of opposite signs, but a similar effect is not feasible in the multizonal lens due to its refractive design. Still, the multizonal-refractive lens’s performance was not substantially affected by LCA, which results from its lower material dispersion, specified by a high Abbe number, as confirmed by the results of the current study.
The PanOptix lens has been extensively studied, both on an optical bench and in clinical trials. Using the same benchtop setup and spectral conditions as in our study, Naujokaitis et al. compared the laboratory-derived defocus curves of the PanOptix with a complementary (EDoF) system [25]. According to their findings, the trifocal lens had a simulated VA of 0.2 logMAR or better throughout the range of + 0.5 D to − 3.5 D, and they also identified three peaks at 0 D of focus (− 0.02 logMAR), − 1.75 D (0.03 logMAR), and − 2.5 D (0.02 logMAR) [25]. Our results show equal or better VA for the same defocus range, but we observed lower values of simulated VA for far vision (0.00 logMAR) and near focus (0.06 logMAR). These minute discrepancies can be attributed to differences in the metrics used to derive the simulated VA. Naujokaitis et al. used a weighted optical transfer function, while the MTFa was used in our study as the parameter for VA prediction. Despite differences in the approaches used to calculate both metrics, they appear to show comparable results, and both can be used to simulate postoperative performance, as indicated by their high correlation with clinical VA [16].
This agreement between predicted and clinical defocus curves can be found when comparing our data to those from the clinical literature [26, 27]. For instance, a 6-month prospective case series study reported significant improvements in uncorrected and corrected VA outcomes at 1 month after the diffractive lens implantation. The monocular defocus curves showed that a VA equal to or better than 0.30 logMAR was maintained between + 0.50 D to − 3.00 D, with the best VA occurring at 0.00 D and − 2.50 D, which corresponds well with the results of our study [27]. However, we also observed variations in reported defocus curves between clinical studies of the same model. Kohnen et al. reported the secondary VA peak of a diffractive lens at − 2.00 D in both monocular (0.01 logMAR) and binocular (− 0.02 logMAR) defocus curves, yielding weaker agreement with our in vitro results [26]. In a clinical setting, however, non-IOL-related factors, such as intersubjective variability or measurement error, may affect defocus-curve results, leading to disagreement when laboratory findings collected under strictly controlled conditions are compared against clinical ones.
Eom et al. enrolled 40 patients implanted with the Precizon and assessed IOL-induced astigmatism [28]. That study found an increase in astigmatism related to the IOL ranging from 0.68 ± 0.58 D to 1.05 ± 0.81 D, depending on the lens orientation. However, the authors concluded that it was not clinically significant given its low impact on manifest refraction. Still, this finding may support our observation of the astigmatic-like effect in the recorded USAF-target images. Secondary to the astigmatism assessment, Eom et al. reported a binocular defocus curve for their patients [28]. Alió et al. also evaluated the defocus curve of ten (Precizon 570 NVA) patients [29]. Despite differences in the intermediate VA level between the two studies, which may result from the small (10) study population analyzed by Alió's group, there are apparent similarities to the simulated VA in our study. Although zero-defocus VA was better than predicted from our optical measurements in those clinical studies, at − 1 D, the MTF-based prediction appears to overestimate VA. In our study, a VA value of 0.05 logMAR was predicted, but for Eom et al., it was 0.1 logMAR [28]. We noted a similar difference in the prediction for PanOptix, which, besides clinical factors, may also indicate the need for refinement of the applied VA-prediction formula. Although the findings of this in vitro study cannot be extrapolated one-to-one into a clinical outlook, valuable insight into the optical properties of multizonal-refractive designs can be gained, and good agreement with the average effect observed clinically is obtained.
Conclusions
A multizonal-refractive design appears to produce a comparable optical performance to a standard trifocal lens at an extended range of focus. This first optical-bench analysis in polychromatic light has shown that the multizonal IOL provides a high level of visual quality across all distances and may be considered an alternative to diffractive technology. Although the diffractive lens’s chromatic aberration was increased at the far point, it was compensated for at other distances. By contrast, the multizonal IOL showed a low level of LCA that minimally affected the optical performance across the studied defocus range. Still, the effect of chromatic aberration on visual quality and the depth of focus in pseudophakic eyes needs to be investigated.
References
Breyer DRH, Kaymak H, Ax T, Kretz FTA, Auffarth GU, Hagen PR. Multifocal intraocular lenses and extended depth of focus intraocular lenses. Asia Pac J Ophthalmol (Phila). 2017;6(4):339–49.
Alio JL, Plaza-Puche AB, Fernandez-Buenaga R, Pikkel J, Maldonado M. Multifocal intraocular lenses: an overview. Surv Ophthalmol. 2017;62(5):611–34.
de Vries NE, Nuijts RM. Multifocal intraocular lenses in cataract surgery: literature review of benefits and side effects. J Cataract Refract Surg. 2013;39(2):268–78.
Łabuz G, van den Berg TJ, Auffarth GU, Khoramnia R. Light scattering from a diffractive-refractive intraocular lens: a goniometer-based approach for individual zone assessment. Biomed Opt Express. 2022;13(12):6724–32.
Artigas JM, Menezo JL, Peris C, Felipe A, Diaz-Llopis M. Image quality with multifocal intraocular lenses and the effect of pupil size: comparison of refractive and hybrid refractive-diffractive designs. J Cataract Refract Surg. 2007;33(12):2111–7.
Dyrda A, Martinez-Palmer A, Martin-Moral D, et al. Clinical results of diffractive, refractive, hybrid multifocal, and monofocal intraocular lenses. J Ophthalmol. 2018;2018:8285637.
Yildirim Karabag R, Gunenc U, Aydin R, Arikan G, Aslankara H. Visual results following implantation of a refractive multifocal intraocular lens in one eye and a diffractive in the contralateral eye. Turk J Ophthalmol. 2018;48(1):6–14.
Vinas M, Dorronsoro C, Gonzalez V, Cortes D, Radhakrishnan A, Marcos S. Testing vision with angular and radial multifocal designs using adaptive optics. Vision Res. 2017;132:85–96.
Royo M, Jimenez A, Pinero DP. Clinical outcomes of cataract surgery with implantation of a continuous transitional focus intraocular lens. J Cataract Refract Surg. 2020;46(4):567–72.
Cochener B, Vryghem J, Rozot P, et al. Clinical outcomes with a trifocal intraocular lens: a multicenter study. J Refract Surg. 2014;30(11):762–8.
Alio JL, Montalban R, Pena-Garcia P, Soria FA, Vega-Estrada A. Visual outcomes of a trifocal aspheric diffractive intraocular lens with microincision cataract surgery. J Refract Surg. 2013;29(11):756–61.
María S, Millán FV. Through-focus energy effciency and longitudinal chromatic aberration of three presbyopia-correcting intraocular lenses. Transl Vis Sci Technol. 2020;9(12):13.
ISO. ISO-11979-2: Ophthalmic implants—intraocular lenses—part 2: optical properties and test methods. Geneva: The International Organization for Standardization; 2014.
Yan W, Łabuz G, Khoramnia R, Auffarth GU. Trifocal intraocular lens selection: predicting visual function from optical quality measurements. J Refract Surg. 2023;39(2):111–8.
Łabuz G, Papadatou E, Khoramnia R, Auffarth GU. Longitudinal chromatic aberration and polychromatic image quality metrics of intraocular lenses. J Refract Surg. 2018;34(12):832–8.
Alarcon A, Canovas C, Rosen R, et al. Preclinical metrics to predict through-focus visual acuity for pseudophakic patients. Biomed Opt Express. 2016;7(5):1877–88.
Atchison DA, Smith G. Chromatic dispersions of the ocular media of human eyes. J Opt Soc Am A. 2005;22(1):29–37.
Millan MS, Vega F, Poyales F, Garzon N. Clinical assessment of chromatic aberration in phakic and pseudophakic eyes using a simple autorefractor. Biomed Opt Express. 2019;10(8):4168–78.
Vinas M, Gonzalez-Ramos AM, Aissati S, et al. Longitudinal chromatic aberration in patients implanted with trifocal diffractive hydrophobic IOLs. J Refract Surg. 2020;36(12):804–10.
Lee Y, Łabuz G, Son HS, Yildirim TM, Khoramnia R, Auffarth GU. Assessment of the image quality of extended depth-of-focus intraocular lens models in polychromatic light. J Cataract Refract Surg. 2020;46(1):108–15.
Pablo Pérez-Merino CD, Llorente L, Durán S, Jiménez-Alfaro I, Marcos S. In vivo chromatic aberration in eyes implanted with intraocular lenses. Invest Ophthalmol Vis Sci. 2013;54(4):2654–61.
Loicq J, Willet N, Gatinel D. Topography and longitudinal chromatic aberration characterizations of refractive-diffractive multifocal intraocular lenses. J Cataract Refract Surg. 2019;45(11):1650–9.
Siedlecki D, Jóźwik A, Zając M, Hill-Bator A, Turno-Kręcicka A. In vivo longitudinal chromatic aberration of pseudophakic eyes. Optom Vis Sci. 2014;91(2):240–6.
Bradley A, Xu R, Wang H, et al. The impact of IOL Abbe number on polychromatic image quality of pseudophakic eyes. Clin Ophthalmol. 2020;14:2271–81.
Naujokaitis T, Auffarth GU, Khoramnia R, Łabuz G. Complementary system vs. conventional trifocal intraocular lens: comparison of optical-quality metrics and unwanted-light distribution. J Cataract Refract Surg. 2022;13:10–97.
Kohnen T, Herzog M, Hemkeppler E, et al. Visual performance of a quadrifocal (trifocal) intraocular lens following removal of the crystalline lens. Am J Ophthalmol. 2017;184:52–62.
Alio JL, Plaza-Puche AB, Alio Del Barrio JL, et al. Clinical outcomes with a diffractive trifocal intraocular lens. Eur J Ophthalmol. 2018;28(4):419–24.
Eom Y, Yang SK, Yoon EG, et al. Multizonal design multifocal intraocular lens-induced astigmatism according to orientation. J Refract Surg. 2020;36(11):740–8.
Alio JL, Yebana P, Canto M, et al. Clinical outcomes with a new design in multifocal intraocular lens: a pilot study. Eye Vis (Lond). 2020;7:38.
Acknowledgements
Donald J. Munro contributed to the review of the manuscript. Ethics committee approval was not required for this laboratory study.
Funding
This work was supported by unrestricted research grants from Klaus Tschira Stiftung and OPHTEC BV. The journal’s Rapid Service fee was funded by OPHTEC BV. The sponsors had no role in the design, execution, interpretation, or writing of the study.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization: Grzegorz Łabuz and Gerd Uwe Auffarth; investigation: Weijia Yan; data analysis: Weijia Yan, Grzegorz Łabuz; resources: Gerd Uwe Auffarth; draft preparation: Weijia Yan and Grzegorz Łabuz; review and editing: Grzegorz Łabuz, Ramin Khoramnia and Gerd Uwe Auffarth; supervision: Grzegorz Łabuz, Ramin Khoramnia and Gerd Uwe Auffarth; funding acquisition: Gerd Uwe Auffarth. All authors have read and agreed to the published version of the manuscript.
Disclosures
G.U. Auffarth and R. Khoramnia report grants, personal fees, nonfinancial support and consulting fees from Johnson & Johnson Vision Care, Inc. and Alcon Laboratories, Inc.; grants, personal fees, and nonfinancial support from Hoya Corp., Kowa Co. Ltd., Oculentis/Teleon, Carl Zeiss Meditec AG, Santen and SIFI; grants and personal fees from Bausch + Lomb, Biotech and OCULUS Optikgeräte GmbH; and grants from AcuFocus, Inc., Eyebright, Hanita, Ophtec, Ophthalmopro, Physiol, Rayner and VSY outside the submitted work. W. Yan and G. Łabuz declare no potential conflict of interest.
Compliance with Ethics Guidelines
This article is based on bench evaluations and does not contain any studies with human participants or animal performed by any of the authors.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yan, W., Auffarth, G.U., Khoramnia, R. et al. Spectral Effects and Range of Focus in a Multizonal-Refractive Intraocular Lens Compared with a Standard Trifocal Diffractive Design. Ophthalmol Ther 12, 1621–1634 (2023). https://doi.org/10.1007/s40123-023-00679-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00679-z