Abstract
Purpose
To evaluate the clinical and visual outcomes, quality of near vision and the influence of photic phenomena in patients bilaterally implanted with a new Precizon Presbyopic multifocal intraocular lens (IOL).
Methods
In this prospective consecutive case series, 20 eyes of 10 patients were included (mean age 63.80 ± 12.55 years). Uncorrected and corrected visual acuity (far, intermediate and near), subjective refraction, binocular defocus curve, contrast sensitivity (CSV-1000) and quality of vision and satisfaction questionnaires were measured. The follow-up was 12 months after surgery.
Results
At 12 months after surgery, uncorrected distance visual acuity (UDVA) improved with surgery (p = 0.001) with a value of 0.08 ± 0.08 logMAR. Uncorrected near visual acuity (UNVA) was 0.22 ± 0.12 logMAR and distance corrected near visual acuity (DCNVA) was 0.16 ± 0.13 logMAR. Intermediate distance visual acuity (UIVA) was 0.22 ± 0.10 logMAR. Contrast sensitivity outcomes were similar to normal population in photopic conditions and slightly reduced in mesopic conditions of lighting. Defocus curve showed that this multifocal IOL was able to provide a visual acuity (VA) equal or better to 0.16 logMAR between defocus levels of + 1.00 to − 2.50 D. Good patient satisfaction was obtained in quality of vision and satisfaction questionnaires outcomes.
Conclusions
The Precizon Presbyopic NVA IOL (OPHTEC BV) provides good visual outcomes. This multifocal IOL provides a high percentage of spectacle independence due to good VA at far, intermediate and near distances and satisfactory contrast sensitivity. High patient satisfaction was observed in quality of vision and satisfaction questionnaires with a low percentage of patients manifesting photic phenomena.
Similar content being viewed by others
Introduction
Nowadays, the demand for multifocal intraocular lenses (IOLs) has increased which can be attributed to the increase of younger patients that demand a solution for their presbyopia and look for spectacle independence. There are a lot of IOLs and designs to provide an excellent visual performance on various distances of sight. These IOLs look for satisfactory visual acuity (VA) and a suited quality of vision for near, intermediate and far vision [1,2,3,4].
The innovation of this Precizon Presbyopic NVA (OPHTEC BV) multifocal intraocular lens (IOL) lies in its new design, an aspherical segmented refractive optic, which conforms a continuous transitional focus (CTF) optic (Fig. 1). This is an optic with an anterior surface with multiple segments for far and near. A smooth transition from far to near is achieved between the segment. This transition offers a constant defocus between the two sharp focal points, delivering a good intermediate vision. Due to the design, patients benefit from good vision at difference distances independently from the size of the pupil diameter. The use of segments instead of concentric rings should provide better optical quality and reduce photic phenomena.
The aim of this study is to evaluate visual outcomes, quality of near vision and the influence of light distortion in patient bilaterally implanted with this multifocal Precizon Presbyopic IOL.
Methods
Study design
This is a monocentric clinical interim pilot study reporting data at 12 months, from one investigation site. This study is a pilot prospective consecutive non-comparative case series.
Patients
Twenty eyes of 10 patients were bilaterally implanted with the Precizon Presbyopic multifocal IOL. Mean age of the patients was 63.80 ± 12.55 years (range: 42 to 79 years). All patients agreed to participate and signed an informed consent. The study adhered to the tenets of the Declaration of Helsinki and was approved by the local ethical committee (Ethics Committee for Drug Research of Cádiz approved this study as an audit study and gave it the following reference number AP01000740).
Intraocular Lens
The Precizon Presbyopic IOL NVA model 570 (OPTHEC BV) is a one-piece IOL made of a hybrid material hydrophilic/hydrophobic acrylic material with ultraviolet filtering HEMA/EOEMA copolymer, with a refractive index of 1.46. The size of the clear optic diameter is 4.4 mm, with an overall diameter of 12.5 mm.
A multi-zonal design allows the lens to maintain the light distribution and exposure on the foci theoretically regardless of the tilt or decentering of the lens. This IOL provides the ability for a transition in focus between 11 distinct segments (five for distance and six for near vision) with the central segment dedicated for distance vision (Fig. 1). The rotated segments have a width of 0.75 mm and these segments are distributed in such a way that decentration or pupil size has a minimal effect on the ratio between near and far correction [5].
The IOL optic is designated as CTF and is divided into three concentric sectors: the central sector, of higher diameter, is dedicated to distance correction; two peripheral sectors present a bimodal (50–50%) distribution of distance and near correction, and this distribution changes along four segments in each sector. This new optic design with an anterior surface with multiple segments for far and near achieves a soft transition from far to near focus. This transition theoretically offers a constant progressive focus between the two sharp focal points to facilitate a sharp image on the retina delivering a good intermediate vision (Fig. 2) [6].
This IOL has a range optic power between + 1.0 and + 35.0 D (0.5 D increments) and has an addition of + 2.75 D for near focus.
Inclusion and exclusion criteria
The inclusion criteria of this study were candidates with early cataract and presbyopia looking for spectacle independence (cataract or clear lens extraction patients) who qualify for bilateral implantation and patients wishing to be spectacle independent. Exclusion criteria were the presence of any other ocular pathology which could compromise visual outcomes (amblyopia, anterior segment comorbidities, glaucoma, retinal disorders or neuro-ophthalmic disease) and preoperative astigmatism higher than 1.0 D measured with optical biometer or corneal topography.
Preoperative and postoperative examination
All patients were evaluated preoperatively and for each operated eye at day 1, week 1 and months 1, 3 and 12 after surgery.
All measurements were performed by two independent optometrists certified in Good Clinical Practice (ABP and PY) following the same investigational protocol according standard procedures.
The preoperative examination contained an extensive evaluation including: distance visual acuity (DVA) at 4 m with early treatment diabetic retinopathy study (ETDRS) logMAR charts, subjective refraction, contrast sensitivity in photopic and mesopic conditions with and without glare in binocular vision (CSV-1000, Vector Vision), biometry (IOL Master, Zeiss), pupillometry (Sirius, Costruzione Strumenti Oftalmici), slit-lamp examination, topography (Sirius, Costruzione Strumenti Oftalmici) and quality of vision questionnaire.
Postoperatively, patients were evaluated during the follow-up at 1 day, 1 month, 3 months and 12 months after surgery according the same protocol which included: DVA (ETDRS at 4 m), near visual acuity (NVA) (ETDRS reading chart calibrated at 40 cm), intermediate visual acuity (IVA) (ETDRS reading chart calibrated at 80 cm), subjective refraction, contrast sensitivity (in the same conditions to preoperative evaluation), defocus curve in binocular vision, slit-lamp examination, quality of vision [7] and satisfaction questionnaire (a questionnaire adapted for this study was used).
Defocus curve was performed in binocular conditions with the postoperative manifest refraction corrected following the protocol previously published [8,9,10]. The defocus curve was obtained using ETDRS charts at 4 m. Negative lenses were added in 0.50 D steps and the VA was recorded for each type of defocus level. Afterwards, the same procedure was repeated using positive lenses. The range of defocus curve evaluated was from − 5.00 to + 1.50 D. In the defocus curve, 0.00 D of defocus corresponds to far vision, − 1.50 D of defocus corresponds to intermediate vision and − 2.50 D of defocus to near vision.
Contrast sensitivity vision was performed in binocular conditions at a distance of 2.5 m for 4 frequencies in cycles per degree (cpd) (A: 3 cpd, B: 6 cpd, C: 12 cpd and D: 18 cpd) and patients were tested with the postoperative manifest refraction corrected. Four measurements have been performed for each patient, in photopic and mesopic conditions with and without glare. To measure contrast sensitivity in mesopic light condition we used specially designed mesopic (neutral density) filters to reduce the testing light level. The CSV-1000 test provides a glare option, this test incorporates a standardized halogen glare test so it can be used under glare conditions.
Statistical analysis
The statistical analysis was performed with the SPSS software for Windows (IBM SPSS Statistics, version 22.0). Due to small sample size (n < 30), our variables were considered non-normal, and thus we used non-parametric tests for data analysis.
For the continuous variables observed, the Wilcoxon test was used to assess the difference between preoperative and postoperative outcomes. Differences were considered statistically significant when the P value was less than 0.05.
Results
A total of 20 eyes of 10 patients (70% cataract; 30% clear lens extraction) were examined 12 months postoperatively.
Visual acuity and refractive status
Table 1 shows the monocular postoperative refraction and VA in logMAR results 3 and 12 months postoperatively. Uncorrected distance visual acuity (UDVA) improved with the surgery at 3 and 12 months (p < 0.001), it even had a significant improvement between the third and twelfth month (p = 0.015). Corrected distance visual acuity (CDVA) improved significantly after surgery (p < 0.05) and remained stable over time (p = 0.074). The outcomes at 12 months of uncorrected near visual acuity (UNVA) at 40 cm and distance corrected near visual acuity (DCNVA) at 4 m was 0.22 ± 0.12 logMAR and 0.16 ± 0.13 logMAR respectively, remaining stable over time between postoperative visits (p > 0.05). At 3 months, corrected near visual acuity (CNVA) was 0.08 ± 0.05 logMAR, and for intermediate vision the results showed an uncorrected intermediate visual acuity (UIVA) of 0.22 ± 0.10 logMAR.
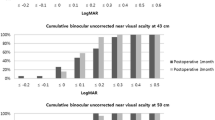
Table 2 shows the binocular VA and refractive results at 3 and 12 months after surgery. Binocularly, the outcomes of this IOL shows an improvement in UDVA after surgery at 3 and 12 months (p < 0.05), they even had a significant improvement between the third and twelfth month (p = 0.040). The uncorrected visual acuity outcomes of distance and near at 12 months after surgery were − 0.01 ± 0.05 logMAR and 0.13 ± 0.12 logMAR, respectively. Intermediate vision at 3 months was 0.16 ± 0.11 logMAR.
Figure 3 shows the distribution of the postoperative spherical equivalent for all eyes at 12 months, 65% of eyes obtained a spherical equivalent between ±0.50 D and 90% of eyes between ±1.00 D.
Defocus curve
The binocular defocus curve is shown in Fig. 4. At 12 months, the maximum value of VA obtained was − 0.08 ± 0.08 logMAR corresponding to the far defocus (0.00 D). A second peak was found at − 2.00 D with a VA of 0.08 ± 0.12 logMAR. Corresponding to near defocus (− 2.50 D) the VA obtained was 0.16 ± 0.15 logMAR while for intermediate vision (− 1.50 D) the VA was 0.12 ± 0.11 logMAR. As shown, this multifocal IOL was able to provide a VA equal or better to 0.16 LogMAR between defocus levels of + 1.00 to − 2.50D.
Contrast sensitivity
The outcomes of contrast sensitivity in photopic and mesopic conditions and measurement with and without glare in binocular vision at 3 months are shown in Fig. 5. This multifocal IOL provides contrast sensitivity values (in log units) similar to those observed in normal population, for an age group between 50 and 75 years of age (Table 3), in photopic lighting conditions (A: 1.68, B: 1.74, C: 1.53, D: 1.05) and slightly reduced in mesopic lighting conditions (A: 1.59, B: 1.68, C: 1.28, D: 0.78).
Contrast sensitivity outcomes 12 months postoperatively. a, Contrast sensitivity values (in log units) in photopic conditions. b, Contrast sensitivity values in photopic conditions with glare. c, Contrast sensitivity values in mesopic conditions. d, Contrast sensitivity values in mesopic conditions with glare. Green line shows the population norms
Questionnaires
Quality of vision questionnaire
Table 4 shows the subjective quality of vision reported by patients at 3 and 12 months postoperatively. At 12 months, 70% of patients reported that they “never” observed glare and 30% of patients said that they had seen glares “occasionally”. With respect to halos, 40% of patients reported that they “never” observed halos, 40% “occasionally”, 20% of patients reported that they “often” seen halos, and 0% of patients reported “usually” seeing halos.
Satisfaction questionnaire
Table 5 shows the subjective satisfaction reported by patients at 12 months postoperatively. The satisfaction questionnaire shows that overall, 90% of patients were satisfied with their visual results: 80% of patients were very satisfied, 10% of patients were quite satisfied with the surgery, and 10% of patients were dissatisfied with their visual outcomes.
Sixty percent of patients answered that they had not required the use of glasses after surgery, 20% had used spectacles for near vision “occasionally” and the other 20% had “often” used spectacles for near vision.
Discussion
Multifocal IOLs aim to provide a good distance, intermediate and near visual outcomes because more often, daily activities requires a high range of vision (for example, use of computers, tablets or car dashboard) [1, 2].
In agreement with previous studies with multifocal IOLs (better than 0.10 logMAR) [1], this IOL provides a good VA (0.08 ± 0.08 logMAR) for distance vision [2, 11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30]. Near vision outcomes achieved in this study (0.22 ± 0.12 logMAR) were compatible with other publications (better than 0.30 logMAR) with difference models of multifocal IOLs [1, 2, 11, 13, 14, 16, 17, 19,20,21, 24, 26,27,28,29,30,31,32,33]. The intermediate visual outcomes obtained in this study (0.22 ± 0.10 logMAR) were similar with other reports (better than 0.30 logMAR) [1, 2, 12, 13, 16, 17, 21, 22, 24, 25, 31,32,33].
The outcomes of the defocus curve binocular analysis show that this IOL provides an acceptable VA with a defocus range of + 1.00 to − 2.50 D (VA equal or better to 0.16 LogMAR), according to a previous study which defined 0.30 logMAR as the limit of good vision [9]. The outcomes of the defocus curve show good values of VA for far vision defocus (− 0.08 ± 0.08 logMAR), near defocus (0.16 ± 0.15 logMAR) and intermediate defocus (0.12 ± 0.11 logMAR). Outcomes in binocular defocus curve are similar to other IOLs [10, 34].
In this study, contrast sensitivity was measured with the CSV-1000 test in different conditions of light, photopic and mesopic conditions and with and without glare in binocular vision. Regarding contrast sensitivity outcomes, this multifocal IOL provides contrast sensitivity values similar to the normal population, for an age group between 50 and 75 years of age, in photopic lighting conditions and slightly reduced in mesopic conditions [35]. Another previous study reported lower contrast sensitivity in multifocal IOLs in mesopic lighting conditions [36].
The subjective quality of vision and patient’s satisfaction was evaluated with two questionnaires at 3 and 12 months after surgery. Outcomes in quality of vision questionnaire at 12 months show that a high percentage of patients reported that they had never seen glares (70%) and 80% of patients reported that they “never” or only “occasionally” seen halos (40% “never”; 40% “occasionally”), and 20% of patients reported that they had seen halos “often” and 0% of patients reported “usually” seeing halos.
The satisfaction questionnaire revealed that 90% of patients were satisfied in general with their visual results and 10% of patient reported that they were dissatisfied with visual outcomes. Only one patient reported was dissatisfied, the reason was a poor neuroadaptation and discomfort due to perception of photic phenomena, especially at night, and the fact that he was a demanding patient, despite having a good VA and not showing a postoperative refractive defect. 60% of patients answered that they had not required the use of glasses after surgery, 20% had used spectacles for near vision “occasionally” to perform near visual activities which require precise details or read small print letters and 20% of patient had used spectacles for near vision “often”.
The main limitation of the current work is its pilot nature, which includes only a several cases [37]. Recently, another study reporting clinical outcomes with this lens has been published [5]. In that study, Royo et al. [5] included both eyes for analysis of VA and refractive parameters. Regarding VA values, results were obtained 6 months after the operation, while in our study results were obtained at 12 months. The monocular and binocular UDVA values were similar (0.03 logMAR and 0.01 logMAR, respectively). The UNVA and UIVA values were slightly higher than those obtained in this study. This may be due to the value of SE mean (− 0.54 D) being slightly more myopic than our research. These previous results can be reflected by comparing the defocus curve; where it can be observed that our curve is displaced towards the top in far defocus, while we observed similar outcomes for intermediate vision, and our outcomes for near defocus were slightly reduced. In general, their defocus curve outcomes, same as our results, provides an acceptable VA with a defocus range of + 1.00 to − 2.50 D (0.30 logMAR as the limit of good vision) [9]. Values of contrast sensitivity and photic phenomena were similar. Nevertheless, further studies with larger samples and without this potential bias are required for confirming these outcomes. The difference compared with Royo et al. [5] study, is that they asked verbally about the perception of disturbing photic phenomena while in our study we measured subjectively the perception of photic phenomena through a validated questionnaire [7].
Conclusions
In conclusion, the Precizon Presbyopic NVA IOL provides good visual outcomes. This multifocal IOL provides a high percentage of spectacle independence after bilateral implantation. Patients reported satisfactory full range of vision with good values of VA at far, intermediate and near distances. Patients obtained good contrast sensitivity. Good patient satisfaction was shown in quality of vision and satisfaction questionnaires with a low percentage of patients manifesting photic phenomena. Future investigations are required to determine the long follow-up outcomes with this new multifocal IOL.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Alió JL, Plaza-Puche AB, Férnandez-Buenaga R, Pikkel J, Maldonado M. Multifocal intraocular lenses: an overview. Surv Ophthalmol. 2017;62(5):611–34.
Alió J, Plaza-Puche AB, Alió Del Barrio JL, Amat-Peral P, Ortuño V, Yébana P, et al. Clinical outcomes with a diffractive trifocal intraocular lens. Eur J Ophthalmol. 2018;28(4):419–24.
Breyer DRH, Kaymak H, Ax T, Kretz FTA, Auffarth GU, Hagen PR. Multifocal intraocular lenses and extended depth of focus intraocular lenses. Asia Pac J Ophthalmol (Phila). 2017;6(4):339–49.
Kohnen T, Titke C, Bohm M. Trifocal intraocular lens implantation to treat visual demands in various distances following lens removal. Am J Ophthalmol. 2016;161:71–7.e1.
Royo MM, Jiménez A, Piñero DP. Clinical outcomes of cataract surgery with implantation of a continuous transitional focus intraocular lens. J Cataract Refract Surg. 2020;46(4):567–72.
Mesa RR, Monteiro T. Continuous transitional focus (CTF): a new concept in ophthalmic surgery. Ophthalmol Ther. 2018;7:223–1.
McAlinden C, Pesudovs K, Moore JE. The development of an instrument to measure quality of vision: the Quality of Vision (QoV) questionnaire. Invest Ophthalmol Vis Sci. 2010;51(11):5537–45.
Vargas V, Radner W, Allan BD, Reinstein DZ, Burkhard Dick H, Alió JL. Methods for the study of near, intermediate vision, and accommodation: an overview of subjective and objective approaches. Surv Ophthalmol. 2019;64(1):90–100.
Buckhurst PJ, Wolffsohn JS, Naroo SA, Davies LN, Bhogal GK, Kipioti A, et al. Multifocal intraocular lens differentiation using defocus curves. Invest Ophthalmol Vis Sci. 2012;53(7):3920–6.
Plaza-Puche AB, Alió JL. Analysis of defocus curves of different modern multifocal intraocular lenses. Eur J Ophthalmol. 2016;26(5):412–7.
Zhao G, Zhang J, Zhou Y, Hu L, Che C, Jiang N. Visual function after monocular implantation of apodized diffractive multifocal or single-piece monofocal intraocular lens randomized prospective comparison. J Cataract Refract Surg. 2010;36(2):282–5.
Lane SS, Javitt JC, Nethery DA, Waycaster C. Improvements in patient reported outcomes and visual acuity after bilateral implantation of multifocal intraocular lenses with +3.0 diopter addition: multicenter clinical trial. J Cataract Refract Surg. 2010;36(11):1887–96.
Alió JL, Pinero DP, Plaza-Puche A, Amparo F, Jiménez R, Rodríguez-Prats JL, et al. Visual and optical performance with two different diffractive multifocal intraocular lenses compared to a monofocal lens. J Refract Surg. 2011;27(8):570–81.
Muñoz G, Albarrán-Diego C, Cerviño A, Ferrer-Blasco T, García-Lázaro S. Visual and optical performance with the ReZoom multifocal intraocular lens. Eur J Ophthalmol. 2012;22(3):356–62.
van der Linden JW, van Velthoven M, van der Meulen I, Nieuwendaal C, Mourits M, Lapid-Gortzak R. Comparison of a new-generation sectorial addition multifocal intraocular lens and a diffractive apodized multifocal intraocular lens. J Cataract Refract Surg. 2012;38(1):68–73.
Alió JL, Plaza-Puche AB, Javaloy J, Ayala MJ, Moreno LJ, Piñero DP. Comparison of a new refractive multifocal intraocular lens with an inferior segmental near add and a diffractive multifocal intraocular lens. Ophthalmology. 2012;119(3):555–63.
Sheppard AL, Shah S, Bhatt U, Bhogal G, Wolffsohn JS. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2013;39(3):343–9.
van der Linden JW, van der Meulen IJ, Mourits MP, Lapid-Gortzak R. Comparison of a hydrophilic and a hydrophobic apodized diffractive multifocal intraocular lens. Int Ophthalmol. 2013;33(5):493–500.
Venter J, Pelouskova M. Outcomes and complications of a multifocal toric intraocular lens with a surface-embedded near section. J Cataract Refract Surg. 2013;39(6):859–66.
Venter JA, Pelouskova M, Collins BM, Schallhorn SC, Hannan SJ. Visual outcomes and patient satisfaction in 9366 eyes using a refractive segmented multifocal intraocular lens. J Cataract Refract Surg. 2013;39(10):1477–84.
Rosa AM, Loureiro Silva MF, Lobo C, Mira JB, Farinha CL, Póvoa JA, et al. Comparison of visual function after bilateral implantation of inferior sector-shaped near-addition and diffractive-refractive multifocal IOLs. J Cataract Refract Surg. 2013;39(11):1653–9.
Alfonso JF, Knorz M, Fernández-Vega L, Rincón JL, Suarez E, Titke C, et al. Clinical outcomes after bilateral implantation of an apodized +3.0 D toric diffractive multifocal intraocular lens. J Cataract Refract Surg. 2014;40(1):51–9.
Cochener B, Vryghem J, Rozot P, Lesieur G, Chevalier JP, Henry JM, et al. Clinical outcomes with a trifocal intraocular lens: a multicenter study. J Refract Surg. 2014;30(11):762–8.
Kim JS, Jung JW, Lee JM, Seo KY, Kim EK, Kim TI. Clinical outcomes following implantation of diffractive multifocal intraocular lenses with varying add powers. Am J Ophthalmol. 2015;160(4):702–9.e1.
Kretz FT, Bastelica A, Carreras H, Ferreira T, Müller M, Gerl M, et al. Clinical outcomes and surgeon assessment after implantation of a new diffractive multifocal toric intraocular lens. Br J Ophthalmol. 2015;99(3):405–11.
Alió JL, Elkady B, Ortiz D, Bernabeu G. Clinical outcomes and intraocular optical quality of a diffractive multifocal intraocular lens with asymmetrical light distribution. J Cataract Refract Surg. 2008;34(6):942–8.
Alió JL, Piñero DP, Plaza-Puche AB, Chan MJ. Visual outcomes and optical performance of a monofocal intraocular lens and a new-generation multifocal intraocular lens. J Cataract Refract Surg. 2011;37(2):241–50.
Alió JL, Pinero DP, Tomas J, Plaza AB. Vector analysis of astigmatic changes after cataract surgery with implantation of a new toric multifocal intraocular lens. J Cataract Refract Surg. 2011;37(7):1217–29.
Alió JL, Plaza-Puche AB, Javaloy J, Ayala MJ. Comparison of the visual and intraocular optical performance of a refractive multifocal IOL with rotational asymmetry and an apodized diffractive multifocal IOL. J Refract Surg. 2012;28(2):100–5.
Alió JL, Plaza-Puche AB, Javaloy J, Ayala MJ, Vega-Estrada A. Clinical and optical intraocular performance of rotationally asymmetric multifocal IOL plate-haptic design versus C-loop haptic design. J Refract Surg. 2013;29(4):252–9.
Alió JL, Montalbán R, Peña-García P, Soria FA, Vega-Estrada A. Visual outcomes of a trifocal aspheric diffractive intraocular lens with microincision cataract surgery. J Refract Surg. 2013;29(11):756–61.
Alió JL, Plaza-Puche AB, Pinero DP, Javaloy J, Ayala MJ. Comparative analysis of the clinical outcomes with 2 multifocal intraocular lens models with rotational asymmetry. J Cataract Refract Surg. 2011;37(9):1605–14.
Alió JL, Plaza-Puche AB, Montalban R, Javaloy J. Visual outcomes with a single-optic accommodating intraocular lens and a low-addition-power rotational asymmetric multifocal intraocular lens. J Cataract Refract Surg. 2012;38(6):978–85.
Alfonso JF, Fernández-Vega Cueto L, Belda-Salmerón L, Montés-Micó R, Fernández-Vega L. Visual function after implantation of a diffractive aspheric trifocal intraocular lens. Eur J Ophthalmol. 2016;26(5):405–11.
Pomerance GN, Evans DW. Test-retest reliability of the CSV-1000 contrast test and its relationship to glaucoma therapy. Invest Ophthalmol Vis Sci. 1994;35(9):3357–61.
Alfonso JF, Puchades C, Fernandez-Vega L, Montés-Micó R, Valcárcel B, Ferrer-Blasco T. Visual acuity comparison of 2 models of bifocal aspheric intraocular lenses. J Cataract Refract Surg. 2009;35(4):672–6.
Ray WA, O'Day DM. Statistical analysis of multi-eye data in ophthalmic research. Invest Ophthalmol Vis Sci. 1985;26(8):1186–8.
Acknowledgements
Not applicable.
Funding
Network for Cooperative Research in Health “OFTARED” – Reference: RD16/0008/0012. Funded by Instituto de Salud Carlos III and co-funded by European Regional Development Fund (ERDF), “A way to make Europe”.
Author information
Authors and Affiliations
Contributions
JL performed medical operations and medical examinations of patients, written and approved the manuscript. PY performed optometrists examinations, data collection and written the manuscript. MC performed data collection, statistical analysis and written the manuscript. ABP performed optometrists examination and reviewed the manuscript. AV performed medical operations and reviewed the manuscript. JAB medical operations and medical examinations and reviewed the manuscript. FL performed medical operations and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients gave their informed consent for their anonymized data to be submitted for audit and publication. Ethics Committee for Drug Research of Cádiz approved this study as an audit study and gave it the following reference number AP01000740.
Consent for publication
Not applicable.
Competing interests
The authors have no proprietary or commercial interest in the medical devices that are involved in this manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alió, J.L., Yébana, P., Cantó, M. et al. Clinical outcomes with a new design in multifocal intraocular lens: a pilot study. Eye and Vis 7, 38 (2020). https://doi.org/10.1186/s40662-020-00205-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40662-020-00205-3