Abstract
Multidrug-resistant (MDR) and extensively drug-resistant (XDR) Pseudomonas aeruginosa isolates are frequent causes of serious nosocomial infections that may compromise the selection of antimicrobial therapy. The goal of this review is to summarize recent epidemiologic, microbiologic, and clinical data pertinent to the therapeutic management of patients with infections caused by MDR/XDR-P. aeruginosa. Historically, conventional antipseudomonal β-lactam antibiotics have been used for the empiric treatment of MDR/XDR-P. aeruginosa. Owing to the remarkable capacity of P. aeruginosa to confer resistance via multiple mechanisms, these traditional therapies are often rendered ineffective. To increase the likelihood of administering empiric antipseudomonal therapy with in vitro activity, a second agent from a different antibiotic class is often administered concomitantly with a traditional antipseudomonal β-lactam. However, combination therapy may pose an increased risk of antibiotic toxicity and secondary infection, notably, Clostridioides difficile. Multiple novel agents that demonstrate in vitro activity against MDR-P. aeruginosa (e.g., β-lactam/β-lactamase inhibitor combinations and cefiderocol) have been recently granted US Food and Drug Administration (FDA) approval and are promising additions to the antipseudomonal armamentarium. Even so, comparative clinical data pertaining to these novel agents is sparse, and concerns surrounding the scarcity of antibiotics active against refractory MDR/XDR-P. aeruginosa necessitates continued assessment of alternative therapies. This is particularly important in patients with cystic fibrosis (CF) who may be chronically colonized and suffer from recurrent infections and disease exacerbations due in part to limited efficacious antipseudomonal agents. Bacteriophages represent a promising candidate for combatting recurrent and refractory infections with their ability to target specific host bacteria and circumvent traditional mechanisms of antibiotic resistance seen in MDR/XDR-P. aeruginosa. Future goals for the management of these infections include increased comparator clinical data of novel agents to determine in what scenario certain agents may be preferred over others. Until then, appropriate treatment of these infections requires a thorough evaluation of patient- and infection-specific factors to guide empiric and definitive therapeutic decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Multidrug-resistant (MDR)-P. aeruginosa has been considered a serious threat by the Centers for Disease Control and Prevention (CDC) for the last decade, accounting for at least 32,600 cases, 2700 deaths, and US $767 million in attributable healthcare costs annually. |
Patient populations at greatest risk of acquiring infections caused by MDR- and extensively drug-resistant (XDR)-P. aeruginosa include those admitted to the intensive care unit (ICU) in the preceding year, immunocompromised patients, and those previously exposed to antipseudomonal carbapenems and fluoroquinolones. |
When the use of conventional β-lactams for empiric treatment of P. aeruginosa infections may be unreliable because of suspected multidrug resistance, monotherapy with novel β-lactam/β-lactamase inhibitors (e.g., ceftolozane–tazobactam, ceftazidime–avibactam, or imipenem–cilastatin–relebactam), or cefiderocol as an alternative, is preferred over combination therapy with conventional agents, followed by therapeutic escalation or de-escalation based on in vitro susceptibility results. |
P. aeruginosa is a major colonizing pathogen in the lungs of patients with cystic fibrosis (CF) and is extremely difficult to eradicate once chronically infected, leading to significant morbidity and mortality. Standard treatment for infections caused by MDR-P. aeruginosa in patients with CF often includes combination therapy of two intravenous antipseudomonal antibiotics with different mechanisms of action to reduce the chance of selecting for resistant organisms. |
Bacteriophages represent a promising candidate for combatting resistant and/or refractory infections caused by MDR/XDR-P. aeruginosa isolates as they target specific host bacteria, circumvent traditional mechanisms of antibiotic resistance, and can restore antibiotic susceptibility by way of evolutionary trade-offs. |
Introduction
Multidrug-resistant (MDR) and extensively drug-resistant (XDR) Pseudomonas aeruginosa represents a frequent and challenging nosocomial pathogen with consistently high rates that range from 11.5% to 24.7% and 9.0% to 11.2%, respectively, according to the INFORM database [1, 2]. The World Health Organization (WHO) designated carbapenem-resistant P. aeruginosa a priority 1 or “critical” pathogen in substantial need of new therapies to counteract this imminent public health crisis of resistance [3]. Additionally, MDR-P. aeruginosa has been considered a serious threat by the Centers for Disease Control and Prevention (CDC) for the last decade, accounting for at least 32,600 cases, 2700 deaths, and US $767 million in attributable healthcare costs annually [4, 5]. In a US national database study, patients with MDR-P. aeruginosa respiratory infections had higher mortality, approximately 7 days longer hospital length of stay (LOS), higher readmission rates, and US $20,000 excess cost per infection relative to those with non-MDR-P. aeruginosa infections [5].
MDR-P. aeruginosa definitions have changed over recent years. According to the CDC in 2008, it was defined as nonsusceptibility to at least one antibiotic in at least three classes for which P. aeruginosa susceptibility is generally expected (i.e., antipseudomonal penicillins [e.g., piperacillin–tazobactam], cephalosporins [ceftazidime, cefepime], fluoroquinolones, aminoglycosides, and carbapenems [meropenem, imipenem]). XDR-P. aeruginosa isolates were defined as nonsusceptibility to at least one agent in all but two or fewer classes of antibiotics [6]. Standardized definitions for MDR, XDR, and pandrug-resistant (PDR) were proposed for infections in 2012, including P. aeruginosa, with the main update including an expanded set of categories from the 2008 CDC definition that included monobactams (aztreonam), phosphonic acids (fosfomycin), and polymyxins [6]. P. aeruginosa with difficult-to-treat resistance (DTR) was proposed in 2018 and defined as nonsusceptibility to all of the following: piperacillin–tazobactam, ceftazidime, cefepime, aztreonam, meropenem, imipenem–cilastatin, ciprofloxacin, and levofloxacin [7, 8].
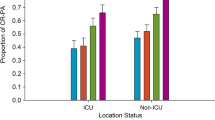
Patient populations at greatest risk of acquiring MDR/XDR-P. aeruginosa infections include those admitted to the ICU in the preceding year, immunocompromised patients, those with chronic pulmonary disease, and patients who received a carbapenem or fluoroquinolone within the previous 3 months [9,10,11,12,13]. Independent factors associated with 14- and 30-day mortality in patients with MDR/XDR-P. aeruginosa infection include those with high-risk source (e.g., intra-abdominal (IAI), pneumonia (PNA), skin and soft tissue (SSTI)), septic shock, high Pitt bacteremia score, and inappropriate definitive antibiotic therapy [14,15,16].
Additionally, in patients with MDR/XDR-P. aeruginosa infections, delayed administration of appropriate antimicrobial therapy with in vitro susceptibility for at least 52 h from index culture collection resulted in a twofold increase in 30-day mortality compared to patients who received appropriate therapy within 52 h [17]. Furthermore, the proportion of patients who received delayed appropriate therapy increased as the number of resistant classes increased. Specifically, antibiotic resistance to at least three antibiotic classes was significantly associated with delayed appropriate therapy.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Mechanisms of Resistance
Pseudomonas aeruginosa has an extraordinary capacity to confer resistance via multiple mechanisms, often at the same time, resulting in resistance to nearly all available antibiotics. Major P. aeruginosa resistance mechanisms are often classified into intrinsic and acquired, which counter most antibiotics, as well as adaptive, which includes biofilm-mediated resistance and the formation of multidrug-tolerant persister cells [18, 19]. P. aeruginosa's high level of intrinsic resistance occurs through restricted outer membrane permeability (approximately 12–100-fold lower than that of Escherichia coli), presence of antibiotic efflux systems, and the production of endogenous antibiotic-inactivating enzymes [20, 21]. Acquired resistance mechanisms result from either horizontal gene transfer (acquisition of aminoglycoside-modifying enzymes and β-lactamases) or mutational events that result in the overexpression of efflux pumps or β-lactamases or the decreased expression or modification of target sites and porins [20, 22, 23]. Adaptive resistance mechanisms are induced by external stimuli (e.g., antibiotic exposure) and become inactive upon removal of the stimulus [24, 25].
Certain antibiotics (e.g., β-lactams, fluoroquinolones) transverse P. aeruginosa’s outer membrane through porin channels, but not surprisingly, decreased antibiotic susceptibility is demonstrated with the loss of specific porin channels. OprD is one of the major and well-characterized porin proteins in P. aeruginosa as it contains a binding site for carbapenems and serves as their preferred route of cellular entry. When OprD is absent, P. aeruginosa exhibits carbapenem resistance, impacting imipenem and meropenem [26].
While the loss of porins such as OprD represents an effective barrier for drug entry into the cell, a reduction in drug accumulation in the periplasmic space can also be achieved through active export by membrane-bound efflux pumps. P. aeruginosa efflux pumps are classified into five families with the resistance-nodulation division (RND) family playing a key role in antibiotic resistance via MexAB-OprM, MexCD-OprJ, MexEF-OprN, and MexXY-OprM [27]. MexAB-OprM, the most described efflux pump in P. aeruginosa, is able to export drugs from several different classes (e.g., fluoroquinolones, tetracyclines, macrolides, trimethoprim, sulfonamides, β-lactamase inhibitors) and has the broadest substrate profile for the β-lactam class being able to export carboxypenicillins, aztreonam, extended-spectrum cephalosporins (e.g., ceftazidime and cefotaxime), and carbapenems (e.g., meropenem but not imipenem) [27,28,29]. Other pumps including MexCD-OprJ, MexEF-OprN, and MexXY-OprM expel β-lactams, fluoroquinolones, and aminoglycosides, respectively [30, 31]. Additionally, overexpression of multiple efflux pumps with concomitant porin downregulation has been identified in clinical strains of P. aeruginosa, expanding bacterial antibiotic resistance and contributing to the development of multidrug resistance [21, 32, 33].
Pseudomonas aeruginosa produces multiple β-lactamases classified via Ambler class A–D. Most common are penicillinases belonging to the molecular class A serine β-lactamases (Pseudomonas-specific enzymes (PSE), carbenicillinases (CARB), TEM families) with PSE being the most prevalent. Class A also encompasses the less common extended-spectrum β-lactamases (ESBL) including TEM, SHV, CTX-M, PER, GES, and IBC in addition to Klebsiella pneumoniae carbapenemase (KPC) [34]. Class B are defined by metallo-β-lactamases (MBLs), which hydrolyze all currently available β-lactams and consist of four major families: IMP, VIM, SPM, and GIM. The most notorious MBL is New Delhi metallo-β-lactamase (NDM) [35]. β-Lactamase inhibitors variably inhibit these enzymes, with no commercially available inhibitor being available against MBL producers. Notably, aztreonam maintains activity against NDM and the addition of avibactam to aztreonam has been shown to provide some improvement in activity when NDM is expressed with other mechanisms of resistance that render aztreonam ineffective (e.g., AmpC derepression) [36]. Class C β-lactamases include chromosomally encoded AmpC. Although intrinsically produced at low levels, overproduction of AmpC β-lactamase in P. aeruginosa can occur either by induction of the ampC gene or through a process of derepression leading to constitutive high-level expression [37, 38]. AmpC derepression in P. aeruginosa often leads to cefepime, ceftazidime, and tazobactam resistance, but has little impact on carbapenem susceptibility unless accompanied by additional resistance mechanisms (e.g., efflux pump overproduction, decreased OprD, and/or production of a class A/class B carbapenemase). AmpC-mediated resistance poses an additional challenge as it can emerge during therapy in a patient receiving an antipseudomonal penicillin, penicillin–inhibitor combination, aztreonam, or extended-spectrum cephalosporin [39]. Class D enzymes have a wide range of substrates and include OXA enzymes, which in general are not inhibited by traditional β-lactamase inhibitors (e.g., tazobactam) and may not be inhibited by new agents (e.g., vaborbactam, relebactam). OXA-10 exhibits ESBL activity and confers ceftazidime and aztreonam resistance, while OXA-31 confers resistance to cefepime [40].
In addition to genome-encoded intrinsic resistance mechanisms, P. aeruginosa can gain resistance via nonhydrolytic antibiotic modification or target binding site alterations [23, 41]. Aminoglycoside resistance can occur via aminoglycoside-modifying enzymes (e.g., N-acetyltransferases, O-nucleotidyltransferases, and O-phosphotransferases), which affect the structural integrity of aminoglycosides to varying degrees via catalytic changes, or through 16S ribosomal RNA target site alteration by RNA methyltransferases [42]. Target site alternations can also confer fluoroquinolone resistance through genome changes in gyrA and parC, which are components of DNA gyrase and topoisomerase IV, respectively [43].
Adaptive resistance increases the ability of P. aeruginosa to survive antibiotic attack owing to transient changes in gene expression in response to an environmental stimulus [24]. In P. aeruginosa, the best characterized mechanisms of adaptive resistance are the formation of biofilm and the generation of persister cells, which result in persistent infection and poor prognosis in patients with cystic fibrosis (CF) [25]. Complex communication pathways called quorum sensing (QS) directly lead to coordinated biofilm formation and the production or reduction in virulence factors through gene expression based on colony population size [44, 45]. Three main systems—Las, Rhl, and pseudomonas quinolone signal (PQS)—have been found to be responsible for the regulation of these virulence factors and rely on the production and detection of the QS autoinducers N-3-oxo-dodecanoyl-homoserine lactone and N-butanoyl-homoserine lactone for activation. As the proportion of cells grow within the population so too does the concentration of signaling molecules which leads to the transcription of multiple virulence factors including elastase, pyocyanin, exotoxin A, and the formation of biofilm. General mechanisms of biofilm-mediated resistance protecting bacteria from antibiotic attack involve prevention of antibiotic penetration, altered microenvironment inducing slow growth of biofilm cells, induction of an adaptive stress response, and persister cell differentiation [46, 47].
Pharmacotherapy
Conventional, antipseudomonal β-lactam antibiotics (i.e., cefepime, ceftazidime, piperacillin–tazobactam, and carbapenems) are commonly prescribed for the empiric treatment of P. aeruginosa, sometimes in combination with a second agent from a different antibiotic class (i.e., aminoglycoside, fluoroquinolone, polymyxin) when there is concern for MDR to increase the chance of administering early, appropriate therapy with in vitro susceptibility [48, 49]. While empiric combination therapy increases the likelihood of administering at least one active in vitro agent for isolates suspected to be MDR, data has yet to validate that continued combination therapy, once the conventional β-lactam has demonstrated in vitro activity, offers any benefit over conventional β-lactam monotherapy [50]. Additionally, P. aeruginosa isolates that demonstrate in vitro susceptibility may have elevated minimum inhibitory concentrations (MICs) at or near the breakpoint for conventional β-lactams, and thus require high-dose, extended infusions to achieve exposures for pharmacokinetic/pharmacodynamic (PK/PD) target attainment. Unfortunately, data suggest that resistance to one antipseudomonal β-lactam is commonly associated with resistance to other conventional β-lactams. This was demonstrated in a study of 290 nonduplicate meropenem-nonsusceptible P. aeruginosa isolates examined at 34 US hospitals. Of those isolates, 36% demonstrated resistance to all other β-lactams tested (cefepime, ceftazidime, piperacillin–tazobactam, and aztreonam). Furthermore, and what has yet to be determined, is whether the use of an antipseudomonal β-lactam with in vitro susceptibility harbors cross-resistance to other antipseudomonal β-lactams and impacts clinical outcomes.
When the use of conventional β-lactams for empiric treatment of P. aeruginosa infections may be unreliable because of suspected MDR, monotherapy with novel β-lactam/β-lactamase inhibitors (e.g., ceftolozane–tazobactam, ceftazidime–avibactam, or imipenem–cilastatin–relebactam) over combination therapy with conventional agents is preferred followed by therapeutic escalation or de-escalation based on in vitro susceptibility results (Table 1) [8]. If β-lactam/β-lactamase inhibitors are unavailable, not tolerated, or demonstrate in vitro resistance, cefiderocol is recommended therapy for serious MDR-P. aeruginosa infections over combination therapy with conventional agents [8].
Ceftolozane–Tazobactam
Ceftolozane–tazobactam (C/T) is an advanced-generation cephalosporin (ceftolozane) combined in a fixed (2:1) combination with a β-lactamase inhibitor (tazobactam), designed to overcome P. aeruginosa resistance mechanisms [54]. Ceftolozane, a novel oxyimino-cephalosporin with more potent penicillin binding protein (PBP) 3 inhibition and higher affinity for PBP1b compared to other β-lactam agents, has less affinity for hydrolysis by P. aeruginosa AmpC cephalosporinases [55,56,57]. Additionally, it is a weak substrate for drug efflux systems, is not impacted by OprD loss, and has independent activity against DTR-P. aeruginosa since it does not rely on tazobactam to restore susceptibility to an otherwise inactive drug [58].
Following the results of the ASPECT-cIAI and ASPECT-cUTI trials, C/T was FDA-approved in 2014 for complicated intra-abdominal infections (cIAI) and complicated urinary tract infections (cUTI), including pyelonephritis, in adult patients at a dosage of 1.5 g every 8 h via intermittent 30-min infusion [59, 60]. C/T was later granted FDA approval for nosocomial pneumonia (NP) including hospital-acquired bacterial pneumonia (HABP) and ventilator-associated bacterial pneumonia (VABP) in adult patients at a dosage of 3 g every 8 h on the basis of results from the ASPECT-NP trial, which evaluated C/T compared with meropenem for NP and demonstrated similar clinical cure (57.1% vs 60%) and 28-day mortality (25.4% vs 18.5%) between groups [61].
In a multicenter, retrospective, observational study assessing C/T for the treatment of serious P. aeruginosa infections in 95 critically ill patients of which 83.3% of isolates were carbapenem-resistant and classified as MDR/XDR, C/T demonstrated favorable clinical response in 71.6% of patients, which was defined as the resolution of presenting signs and symptoms of infection by the end of therapy [62]. Notably, 94.8% of patients had sepsis or septic shock and needed life-supporting therapies such as vasopressors or mechanical ventilation. Forty-six episodes were treated with high-dose C/T (3 g every 8 h) and 38 episodes were treated with standard dose (1.5 g every 8 h). Almost one-half (44.2%) of patients were treated with C/T monotherapy, and the remaining group received combination therapy with standard of care antibiotics. Severe adverse events including thrombocytopenia and seizure occurred in 3.1% (3/95) of patients [62].
Puzniak and colleagues conducted a systematic literature review of 83 studies of C/T for Gram-negative infections comprising 3701 patients, of which 90.7% (N = 2184) had infections caused by P. aeruginosa, and of those, 72.3% and 14% of which were MDR and XDR, respectively [63]. The most common infections were PNA (52.9%), cUTI (14.9%), and cIAI (10.1%), and most patients 47.3% were admitted to the ICU. C/T was used at doses of either 1.5 g or 3 g every 8 h for a median duration of 7–56 days (varying between studies). Of the large studies (those that included more than 50 patients) that included patients with P. aeruginosa infections, positive outcome rates were comparable with clinical success ranging from 56.7% to 83.2% and mortality from 5% to 29% [64,65,66,67,68,69,70,71,72]. Whether P. aeruginosa resistance was a factor in clinical outcome was analyzed by two studies, one of which demonstrated similar proportions of survivors and non-survivors in patients with XDR-P. aeruginosa while the other found a significantly different proportion of MDR vs XDR P. aeruginosa infections between patients with clinical success or failure [64, 65]. Of the studies that compared C/T to other treatment regimens (aminoglycoside-/polymyxin-based regimens or standard of care) in patients with resistant P. aeruginosa infections, C/T was associated with increased clinical cure rates, but no significant difference was identified for all-hospital mortality [66, 67, 73].
Data from the ERACE-PA Global Surveillance Program showed that of the clinical isolates collected from 17 centers in 12 countries from 2019 to 2021, C/T demonstrated activity against a majority of the carbapenemase-negative and carbapenem-resistant P. aeruginosa clinical isolates with 88% and 63% being susceptible according to Clinical and Laboratory Standards Institute (CLSI) breakpoints, respectively (Table 2) [74]. Notably, regional differences in susceptibility patterns for carbapenem-resistant P. aeruginosa were noted for C/T and ranged from 32% to 85%. Additionally, only 15% of isolates that tested carbapenemase-positive phenotypically (VIM, GES, IMP, NDM, or KPC identified) were susceptible, of which 12.5% had KPC. Varying susceptibility among C/T isolates has led to investigations of underlying resistance mechanisms. While common mechanisms of resistance in P. aeruginosa including efflux pump upregulation and porin channel changes have not been shown to significantly impact P. aeruginosa susceptibility to C/T, production and/or overexpression of β-lactamases not inhibited by tazobactam (e.g., metallo-β-lactamases, GES β-lactamases, OXA β-lactamases, and carbapenemases) may result in ceftolozane hydrolysis. Additionally, mutations in chromosomal ampC and ampR genes have been identified, which is of great significance as the omega loop of AmpC is the substrate-binding site for ceftolozane and these mutations have been associated with treatment-emergent C/T resistance [39, 58, 75,76,77].
Ceftazidime–Avibactam
Ceftazidime–avibactam (CZA) combines an anti-pseudomonal cephalosporin, ceftazidime, with the novel diazabicyclooctane non-β-lactam/β-lactamase inhibitor, avibactam. It was FDA-approved in 2015 for the treatment of cUTI, including pyelonephritis, and cIAI in combination with metronidazole followed by approval for the treatment of HABP/VABP in 2018 [81]. While avibactam alone has no intrinsic activity, it extends the in vitro activity of ceftazidime to include P. aeruginosa resistance mechanisms including ESBL-, AmpC-, serine carbapenemase-producing P. aeruginosa, and some class D (OXA-48) enzymes [82, 83]. Like C/T, CZA is not active against MBL-producing strains, but unlike C/T, CZA appears to be active against isolates producing class A carbapenemases such as GES enzymes [84]. On the other hand, CZA may be more affected by the overexpression of efflux pumps compared to C/T [85].
Few studies have examined the effectiveness of CZA against infections caused by MDR-P. aeruginosa isolates. In the largest real-world study examining 203 patients receiving CZA for various MDR Gram-negative infections, 63 (31.0%) had infections due to P. aeruginosa and the most common infection source was respiratory tract (60.3%). Of those patients, clinical failure, 30-day mortality, and 30-day recurrence were reported in 19 (30.2%), 11 (17.5%), and 4 (6.3%) of patients, respectively [86].
Stone and colleagues analyzed the activity of CZA against MDR-P. aeruginosa isolates pooled from the adult phase III clinical trials in patients with cIAI, cUTI, or NP including VABP [87]. Microbiological and clinical responses for patients with one or more MDR-P. aeruginosa isolates were assessed at the test-of-cure (TOC) visit. In the pooled microbiologically modified intention-to-treat (mITT) population, 95 patients with MDR-P. aeruginosa were identified. Favorable microbiological response rates at TOC were 57.1% for CZA compared to 53.8% for comparators, predominantly carbapenems. On the basis of the results of these studies, CZA may be a suitable alternative to carbapenem-based therapies for infections caused by MDR-P. aeruginosa [87].
Similar to C/T, the ERACE-PA Global Study Group found that CZA was also active against a majority of carbapenemase-negative and carbapenem-resistant P. aeruginosa isolates with 91% and 72% susceptibility according to CLSI breakpoints, respectively [74]. CZA, like C/T, demonstrated highly varied susceptibilities based on region, ranging from 34% to 87%. Compared to C/T, more isolates that were phenotypically positive for carbapenemase tested susceptible to CZA including 90% and 100% of GES and KPC, respectively, although only 4% of VIM-producing isolates and none of the IMP- or NDM-producing isolates were CZA susceptible.
In general, of the resistance mechanisms involved in the development of CZA-resistant P. aeruginosa isolates, enzymatic inactivation appears to be the most common with reported class C (AmpC) and class D (OXA) β-lactamase mutations. Like C/T, mutations in the omega loop region of AmpC widen the enzyme’s binding pocket, increasing the catalysis of both ceftazidime and ceftolozane. Interestingly, mutations in the AmpC omega loop also result in reduced affinity for avibactam. Membrane impermeability due to porin mutations and high rates of OprD loss have also been shown to contribute to resistance in individual CZA-resistant strains [88]. Efflux pumps do not appear to play a major role in CZA resistance, although addition of efflux pump inhibitors CCCP and PaβN have been shown to significantly reduce the P. aeruginosa MIC from > 32 to < 0.06 [89].
Combination therapy of CZA with other antimicrobials may have potential in treating these pathogens. An in vitro study by Mikhail and colleagues assessed combinations of CZA with meropenem, amikacin, aztreonam, colistin, or fosfomycin against 21 strains of MDR-P. aeruginosa. MIC combination evaluation and time-kill assays identified an at least twofold decrease for most P. aeruginosa isolates in the majority of combinations tested with amikacin- or aztreonam-containing combinations demonstrating synergy (> 2.15-log10 CFU/mL decrease) [90]. In a separate study, Papp-Wallace and colleagues observed CZA MICs decrease from > 32 mg/L to < 8 mg/L and < 16 with the addition of fosfomycin or colistin, respectively, against CZA-resistant isolates [91].
Imipenem–Relebactam
Another recently developed novel treatment of MDR/XDR-P. aeruginosa infections is the combination of imipenem, a carbapenem, and cilastatin, a renal dehydropeptidase 1 inhibitor, with relebactam. It was approved by the FDA in July 2019 for patients with cUTIs and cIAIs, and more recently approved in June 2020 for HABP and VABP [92, 93]. Relebactam is a bicyclic diazabicyclooctane β-lactamase inhibitor of many class A and class C β-lactamases. This novel antibiotic retains activity against P. aeruginosa with efflux pump and porin loss mutations as well [94]. As a result of relebactam’s pronounced inhibition of these β-lactamases, strains of P. aeruginosa that are imipenem nonsusceptible can be made susceptible to imipenem–relebactam (I-R) [95, 96].
Clinical data for the use of I-R against infections caused by MDR-P. aeruginosa were evaluated in RESTORE-IMI [96]. In this randomized controlled trial, I-R was compared to imipenem + colistin (IMI + CST) in 47 adults with carbapenem-resistant cIAIs, cUTIs, HABP, or VABP of which P. aeruginosa was the most commonly isolated organism at 77% of infections (36/47). Patients included in the study had primary VABP (29%), cUTI, or pyelonephritis (each 25.8%). The overall rate of favorable clinical response at day 28 was significantly higher in the I-R group compared to IMI + CST (71% vs 40%; 90% confidence interval (CI) 1.3–51.5). This favorable response was also seen in a subset of patients with P. aeruginosa infections with 13/16 (81%) of I-R and 5/8 (63%) of IMI + CST having a favorable response. Day 28 all-cause mortality occurred in 2 of 21 patients in the I-R group compared to 3 of 10 patients in the IMI + CST group. Additionally, although this was a 20% lower mortality rate in the I-R group compared to the IMI + CST group (10% vs 30%; 90% CI − 46.4 to 6.7), it was not statistically significant. Serious adverse events occurred more frequently in the IMI + CST group at 31.3% compared to the I-R group at 9.7%. Treatment-emergent nephrotoxicity occurred at a rate of 10% in the I-R group and 56% in the IMI + CST group (p = 0.002). The results of RESTORE-IMI 1 support the conclusion that I-R is an effective and well-tolerated option for the treatment of carbapenem-nonsusceptible infections.
Imipenem–relebactam was shown to be active against MDR-P. aeruginosa in a susceptibility analysis from 490 P. aeruginosa isolates in a surveillance study in New York City. Imipenem was susceptible for 70% of isolates at a susceptibility breakpoint of ≤ 2 mg/L and for 98% of P. aeruginosa isolates when relebactam was added at a fixed concentration of 4 mg/L (consistent with current CLSI breakpoints) [97]. Imipenem MIC50 and MIC90 values decreased fourfold with the addition of relebactam, noted for isolates with depressed OprD expression and variable AmpC expression. A lack of activity was also noted for isolates with OXA (Class D) β-lactamase enzymes, especially those of Acinetobacter baumannii [98].
In more recent data comparing I-R activity to that of C/T and CZA against MDR/XDR-P. aeruginosa, 1445 isolates with known MICs from 51 Spanish hospitals were analyzed. Overall, isolates were found to have low MICs to I-R with MIC50/90 of 0.5 mg/L and 1 mg/L, respectively, 4- and 16-fold lower than that of imipenem alone. I-R also had the highest susceptibility rate (97.3%) followed by CST (94.6%), C/T (94.6%), and CZA (94.2%) when using EUCAST clinical breakpoints. Interestingly, patients that developed C/T and/or CZA resistance during therapy had increased susceptibility to I-R. Most often, C/T and CZA resistance development was due to mutations in the omega loop of AmpC that increased susceptibility to imipenem [99]. Thus, I-R may be a reasonable option for rescue therapy in the setting of treatment-emergent C/T and CZA resistance secondary to AmpC mutations. For imipenem-resistant strains, I-R susceptibility was 80.5% compared to 86.4% for XDR strains. Notably, all of the 37 strains that exhibited I-R resistance (2.6%) produced an acquired carbapenemase, which were not present in any of the I-R-susceptible isolates. Hence, there was a near-perfect correlation between I-R resistance and carbapenemase production, which means metallo-β-lactamase production remains a challenge for new drug development.
Cefiderocol
Cefiderocol (FDC), a novel siderophore cephalosporin, demonstrates broad-spectrum Gram-negative coverage and was developed to combat MDR Gram-negatives such as carbapenem-resistant P. aeruginosa and A. baumannii [100]. Cefiderocol is currently FDA-approved for complicated cUTI in adult patients with susceptible Gram-negative bacteria as a last-line treatment option. Its novel mechanism of action involves chelating with ferric iron to utilize bacterial iron transport systems, increasing periplasmic concentrations in Gram-negative bacteria. The resultant higher periplasmic concentrations facilitate the PBP3 saturation causing cell wall synthesis breakdown.
CREDIBLE-CR, a phase 3, randomized, international study trial, examined the safety and efficacy of FDC against best available treatment (BAT) for the treatment of carbapenem-resistant Gram-negative infections [8]. This open-label trial included 118 patients from 100 centers, with P. aeruginosa making up 19% (22/118) of all infections in the mITT analysis and 45% of patients having NP. Clinical cure rates at TOC were similar in the FDC group [50% (95% CI 33.8–66.2)] compared to the BAT group, which consisted primarily of CST-based regimens, [53% (95% CI 28.90–75.60)] for NP. However, all-cause mortality differences were noted between the two groups with 25% for the FDC group compared to 11% for the BAT group at day 14. This mortality difference was sustained until day 28 and was primarily seen in patients with concomitant Acinetobacter spp. infections. Upon further data stratification, all-cause mortality in patients with infections that were caused by monomicrobial P. aeruginosa, or Acinetobacter spp. were 18% (2/11) and 50% (21/42), respectively. When comparing monomicrobial P. aeruginosa infections between FDC and BAT, all-cause mortality remained at 18% (2/11). On the basis of these results, infections caused by carbapenem-resistant Acinetobacter spp. may have been driving the higher mortality rates. Furthermore, patients in the FDC group had higher rates of shock, ICU admission, and prior antibiotic exposure than their BAT-treated counterparts, which may have confounded results. In general, the CREDIBLE-CR study highlighted that FDC performs as well as combinations containing extended-infusion meropenem, polymyxins, and/or aminoglycosides for the treatment of infections caused by carbapenem-resistant P. aeruginosa.
Cefiderocol resistance in P. aeruginosa is a complex topic not yet well understood and in need of continued exploration. Surveillance studies investigating the in vitro activity of FDC against MDR-P. aeruginosa are limited. Combined data of 1500 carbapenem-nonsusceptible P. aeruginosa isolates indicate that more than 97% had FDC MICs of ≤ 4 mg/L or less. Notably, most if not all isolates were obtained from patients without previous exposure to FDC. Cefiderocol has demonstrated high activity against C/T-resistant P. aeruginosa strains in surveillance studies with FDC MIC50/90 at 0.25 and 2 mg/mL for 199 isolates, respectively, although none of the strains were collected after FDC or C/T exposure [101, 102]. While FDC-resistant P. aeruginosa isolates are rare and usually attributed to the production of metallo-β-lactamases, emerging data demonstrate the potential for P. aeruginosa nonsusceptibility to FDC without previous FDC exposure [100]. A recent case report detailed the emergence of an FDC-resistant P. aeruginosa isolate with single nucleotide polymorphisms (SNPs) in TonB-dependent iron transporter receptor and chromosomal AmpC β-lactamase genes without prior FDC exposure [103]. While these mutations may have occurred during disk diffusion susceptibility testing, it is plausible that they were present before testing since there were 29 additional SNPs in a separate strain isolated from the same culture source. Thus, FDC MIC testing of P. aeruginosa isolates prior to FDC use is warranted [104].
Special Population: Cystic Fibrosis
Pseudomonas aeruginosa is a major colonizing pathogen in the lungs of patients with cystic fibrosis (CF) and is extremely difficult to eradicate once chronically infected, leading to significant morbidity and mortality [105]. This is theorized to be caused by numerous factors including patients’ pathological inability to clear respiratory secretions, impaired innate production of antibacterial peptides, reduced phagocytosis by CF cells, impaired host defenses from low levels of nitric oxide and glutathione, and genetic adaptations of P. aeruginosa [106]. Young patients with CF are often colonized with multiple wild-type non-mucoid P. aeruginosa strains until eventual conversion to mucoid and biofilm-producing strains, which occur in over 80% of patients with CF aged 25 years or older [107]. Mucoid conversion is thought to be caused in large part by mutations in the mucA gene, which leads to alginate hyperproduction and increased resistance to innate host defenses in the lungs [108, 109]. Upwards of 84–93% of clinical P. aeruginosa mucoid isolates in patients with CF have mucA mutations [110, 111]. An overproduction of the alginate matrix allows anchoring for biofilm formation, which further increases resistance to host phagocytosis, decreases antibiotic penetration, and allows for planktonic formation of new infection sites [109]. These new infections often induce CF exacerbations leading to hospital admissions and subsequent antibiotic exposure, further selecting for resistance in both mucoid and non-mucoid P. aeruginosa strains.
Standard treatment for infections caused by MDR-P. aeruginosa in patients with CF often includes combination therapy consisting of two intravenous antipseudomonal antibiotics (e.g., piperacillin/tazobactam, ceftolozane/tazobactam, ceftazidime/avibactam, cefepime, or a carbapenem plus a second antipseudomonal agent such as a fluoroquinolone, aminoglycoside, or colistin) with synergistic mechanisms of action to reduce selection of resistant organisms [112,113,114,115,116]. Additionally, inhaled antibiotics are often used to decrease the risk of exacerbations from P. aeruginosa colonization. Multiple in vitro studies have evaluated the antimicrobial susceptibility patterns of P. aeruginosa isolates collected from the lower respiratory tract of patients with CF for novel β-lactam/β-lactamase inhibitor combinations and cefiderocol. A retrospective review was conducted comparing the in vitro activities of C/T, CZA, and CST against 42 P. aeruginosa isolates from the respiratory tract of 32 adults with CF. In general, isolates were more susceptible to C/T than CZA (60% versus 43%) and of the 38 (90%) isolates considered highly drug resistant, more were susceptible to C/T than CZA (55% versus 45%) [117]. Another in vitro study tested 273 P. aeruginosa isolates from 39 hospitals in 17 countries against CZA, C/T, ceftazidime, piperacillin–tazobactam, and tobramycin [118]. Both CZA (MIC50/90, 2/8 mg/L; 96.0% susceptible) and C/T (MIC50/90, 1/4 mg/L; 90.5% S) exhibited potent activity against the P. aeruginosa isolates. Against isolates resistant to meropenem, 78.9% were CZA-susceptible while 47.4% were C/T-susceptible. Among MDR isolates (36.3% of isolates), 88.9% and 73.7% of isolates were susceptible to CZA and C/T, respectively. In total, 65.4% of C/T-nonsusceptible isolates were susceptible to CZA and 18.2% of CZA-resistant isolates were susceptible to C/T. Results of these in vitro studies suggest C/T and CZA may be valuable options to consider for the treatment of CF pulmonary exacerbations caused by P. aeruginosa, with in-house susceptibilities guiding choice of empiric therapy between the two. Currently, there are no clinical trials for the use of FDC in patients with CF. Future research investigating the lung PK penetration, safety concerns, and synergistic antibiotic concentrations is warranted to guide clinical use of FDC.
Bacteriophage Therapy
Continued development of novel treatment approaches against MDR/XDR-P. aeruginosa, including planktonic, mucoid, and biofilm-producing strains, remain a top priority to reduce associated morbidity and mortality. One strategy is the use of bacteriophage (phage) therapy. Lytic phages are viruses that infect a host bacterium and utilize the bacteria’s biological machinery for replication, ultimately leading to host cell lysis [119]. Phage therapy is an emerging anti-infective treatment option for refractory, MDR, and biofilm-mediated infections. While phage therapy has been used to treat bacterial infection for over 100 years, it has gained slow adoption in western medicine because of the advent of antibiotics and large knowledge gaps contributing to heterogeneity in approach [120, 121].
Phage dosing, route of administration, and frequency remain poorly understood. Single doses of 1 × 106 to 1 × 109 PFU/mL (plaque forming units per milliliter) have been used for topical application; however, current data is lacking to make definitive recommendations for dosing frequency [122, 123]. Moreover, multiple doses may be favored for adequate phage concentrations at the infection site. Unlike antibiotics, phages can increase their concentration exponentially at the site of infection as a result of replication. This may complicate dosing parameters depending on the type of infection but may prove beneficial for eradication of deep-seated infections. Multiplicity of infection (MOI) or the ratio of phage to bacteria is another key parameter used for determining optimal concentrations of phage for bactericidal activity. Adjustments in this ratio may be specific to patient and/or phage products to maximize activity. In a case series where a patient with a ventricular assist device (VAD) had an infection caused by MDR/XDR-P. aeruginosa, the patient developed fever and wheezing that were likely the result of high concentration phage (1 × 1011 PFU/mL) administration [124]. When this concentration was diluted to 1 × 1010 and re-administered, the fever and wheezing subsided. It was determined that the reaction was due to pyrogens acquired through the propagation process, though the concentration of pyrogens in the initial preparation was below the FDA limit [125]. This reaction suggests a possible threshold in which the risk of hypersensitivity reactions outweighs the efficacy of phage therapy, which has yet to be delineated for the treatment of MDR/XDR-P. aeruginosa or any other bacteria regardless of route of administration or infection type. In one of the few clinical trials that looked at treating MDR-P. aeruginosa with phage, phage therapy (PP1311 at 1 × 109 PFU/mL) was compared with standard of care (1% sulfadiazine silver emulsion cream) for the treatment of burn wound infections [126]. The trial was stopped early because of topical preparation stability issues, reduced phage concentrations, and subsequent efficacy concerns. This may suggest that there are potential issues related to manufacturing, drug stability, and selection of phage concentrations based on bacterial density at the site of infection. Further PK/PD studies are needed to address phage titers, susceptibility, phage resistance, and the generation of neutralizing antibodies when dosing. Phages and antibiotics have some overlapping PD principles. As with antibiotics, the PD goal of phage therapy is to maximize the number of phages that reach the infection site and kill as many bacteria as possible. However, there are PD differences between antibiotics and phages, which include host density and their growth rates at the site of infection, number of phages present, infectivity rate of phages, phage replication time within bacterial cells (latency period), phage burst size (number of phage progeny), and clearance of phage, among others [127].
One of the most important attributes phage therapy can provide is the ability to circumvent traditional mechanisms of antibiotic resistance seen in MDR/XDR-P. aeruginosa. This principle was demonstrated in a study examining the efficacy of phage ØA392 against an imipenem-resistant P. aeruginosa isolate in a mouse model where phage demonstrated microbiological eradication [128]. Against P. aeruginosa isolates obtained from patients with CF, phage produces enzymes to break up biofilms and alginate associated with mucoid P. aeruginosa strains [129]. In one such case, a patient with CF and active P. aeruginosa respiratory infection experienced refractory respiratory failure and CST-induced renal failure prior to receiving 8 weeks of phage cocktail administration (AB-PA01). After completion of therapy, the patient experienced clinical resolution and did not have an exacerbation within the 100 days following phage therapy [130].
Another important advantage of phage therapy is the ability to restore antibiotic susceptibility by way of evolutionary trade-offs, or mutations that enable bacteria to resist phage infection causing changes in the genes that code for antibiotic resistance mechanisms. Chan et al. demonstrated that use of a lytic phage (OMKO1) targeting MDR-P. aeruginosa’s outer membrane porin M (OprM) of the multidrug efflux system MexAB and MexXY resulted in changes to the efflux pump mechanism through phage selection [131]. In this case, phage selection resulted in MDR bacteria that became more susceptible to ciprofloxacin, ceftazidime, tetracycline, and erythromycin.
Other than the clinical trial previously mentioned, experience with phage for the treatment of MDR/XDR-P. aeruginosa is limited primarily to case reports with phage obtained via expanded access for compassionate use. These case reports have varied widely in approach, methodology, clinical indications, dosing, route of administration, and outcomes. Large gaps in knowledge contribute to the heterogeneity in approach and lack of clear consensus in many important clinical areas, underscoring the need for additional research that is very much warranted.
Conclusion
Multidrug-resistant Gram-negative infections continue to challenge the healthcare community and complicate antimicrobial decisions. P. aeruginosa remains a public health threat despite ongoing antibiotic stewardship and drug development efforts. This is due in large part to P. aeruginosa’s ability to evade host defenses and render multiple antibiotic classes ineffective via rapid development of complex resistance mechanisms. Prompt initiation of appropriate antipseudomonal therapy with in vitro susceptibility is essential to treat P. aeruginosa infections and prevent detrimental impacts associated with delayed therapy (e.g., significant increases in morbidity, mortality, need for surgical intervention, length of hospital stay, and overall cost of treatment). The recent FDA approval of multiple novel agents adds to the antipseudomonal armamentarium and may help to ensure early administration of appropriate therapy while minimizing development of resistance. However, while these agents have demonstrated high activity in vitro against MDR/XDR-P. aeruginosa isolates in large surveillance studies, variability among agents exists, likely because of regional variation of resistance mechanisms and phenotypes. Additionally, there is a need for comparative clinical evaluations of these agents to determine whether there is a benefit to the use of certain agents over others in different clinical scenarios.
Variable in vitro data and sparse clinical comparative data between novel antipseudomonal agents highlight the importance of thoroughly evaluating regional and local susceptibility patterns as well as patient-specific information when selecting empiric and definitive antimicrobial therapy for patients with infections caused by MDR/XDR-P. aeruginosa. Continued monitoring of evolving antibiotic resistance patterns and research focused on novel approaches including phage therapy are key to minimizing the impact MDR/XDR-P. aeruginosa infections have on patients and the healthcare system.
References
Recio R, Mancheño M, Viedma E, et al. Predictors of mortality in bloodstream infections caused by Pseudomonas aeruginosa and impact of antimicrobial resistance and bacterial virulence. Antimicrob Agents Chemother. 2020;64(2):e01759–e1819. https://doi.org/10.1128/AAC.01759-19.
Sader HS, Castanheira M, Duncan LR, Flamm RK. Antimicrobial susceptibility of Enterobacteriaceae and Pseudomonas aeruginosa isolates from United States medical centers stratified by infection type: results from the International Network for Optimal Resistance monitoring (INFORM) surveillance program, 2015–2016. Diagn Microbiol Infect Dis. 2018;92(1):69–74. https://doi.org/10.1016/j.diagmicrobio.2018.04.012.
Tacconelli E, Carrara E, Savoldi A, Harbarth S, Mendelson M, Monnet DL, Pulcini C, Kahlmeter G, Kluytmans J, Carmeli Y, Ouellette M, Outterson K, Patel J, Cavaleri M, Cox EM, Houchens CR, Grayson ML, Hansen P, Singh N, Theuretzbacher U, Magrini N; WHO Pathogens Priority List Working Group. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018 Mar;18(3):318–327. https://doi.org/10.1016/S1473-3099(17)30753-3.
CDC. Antibiotic resistance threats in the United States. Atlanta: CDC; 2019.
Tabak YP, Merchant S, Ye G, et al. Incremental clinical and economic burden of suspected respiratory infections due to multi-drug-resistant Pseudomonas aeruginosa in the United States. J Hosp Infect. 2019;103(2):134–41. https://doi.org/10.1016/j.jhin.2019.06.005.
Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–81. https://doi.org/10.1111/j.1469-0691.2011.03570.x.
Kadri SS, Adjemian J, Lai YL, et al. Difficult-to-treat resistance in gram-negative bacteremia at 173 US hospitals: retrospective cohort analysis of prevalence, predictors, and outcome of resistance to all first-line agents. Clin Infect Dis. 2018;67(12):1803–14. https://doi.org/10.1093/cid/ciy378.
Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America guidance on the treatment of extended-spectrum β-lactamase producing Enterobacterales (ESBL-E), carbapenem-resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat resistance (DTR-P. aeruginosa). Clin Infect Dis. 2021;72(7):e169–83. https://doi.org/10.1093/cid/ciaa1478.
Raman G, Avendano EE, Chan J, Merchant S, Puzniak L. Risk factors for hospitalized patients with resistant or multidrug-resistant Pseudomonas aeruginosa infections: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2018;7(1):79. https://doi.org/10.1186/s13756-018-0370-9.
Montero M, Sala M, Riu M, et al. Risk factors for multidrug-resistant Pseudomonas aeruginosa acquisition. Impact of antibiotic use in a double case-control study. Eur J Clin Microbiol Infect. 2010;29(3):335–9. https://doi.org/10.1007/s10096-009-0850-1.
Micek ST, Reichley RM, Kollef MH. Health care-associated pneumonia (HCAP): empiric antibiotics targeting methicillin-resistant Staphylococcus aureus (MRSA) and Pseudomonas aeruginosa predict optimal outcome. Medicine (Baltimore). 2011;90(6):390–5. https://doi.org/10.1097/MD.0b013e318239cf0a.
Lodise TP, Miller CD, Graves J, et al. Clinical prediction tool to identify patients with Pseudomonas aeruginosa respiratory tract infections at greatest risk for multidrug resistance. Antimicrob Agents Chemother. 2007;51(2):417–22. https://doi.org/10.1128/AAC.00851-06.
Joo EJ, Kang CI, Ha YE, et al. Impact of inappropriate empiric antimicrobial therapy on outcome in Pseudomonas aeruginosa bacteraemia: a stratified analysis according to sites of infection. Infection. 2011;39(4):309–18. https://doi.org/10.1007/s15010-011-0124-6.
Evans SR, Tran TTT, Hujer AM, et al. Rapid molecular diagnostics to inform empiric use of ceftazidime/avibactam and ceftolozane/tazobactam against Pseudomonas aeruginosa: PRIMERS IV. Clin Infect Dis. 2019;68(11):1823–30. https://doi.org/10.1093/cid/ciy801.
Torres A, Chalmers JD, Dela Cruz CS, et al. Challenges in severe community-acquired pneumonia: a point-of-view review. Intensive Care Med. 2019;45(2):159–71. https://doi.org/10.1007/s00134-019-05519-y.
Di Pasquale MF, Sotgiu G, Gramegna A, et al. Prevalence and etiology of community-acquired pneumonia in immunocompromised patients. Clin Infect Dis. 2019;68(9):1482–93. https://doi.org/10.1093/cid/ciy723.
Lodise TP, Patel N, Kwa A, et al. Predictors of 30-day mortality among patients with Pseudomonas aeruginosa bloodstream infections: impact of delayed appropriate antibiotic selection. Antimicrob Agents Chemother. 2007;51(10):3510–5. https://doi.org/10.1128/AAC.00338-07.
Drenkard E. Antimicrobial resistance of Pseudomonas aeruginosa biofilms. Microbes Infect. 2003;5(13):1213–9. https://doi.org/10.1016/j.micinf.2003.08.009.
Mulcahy LR, Burns JL, Lory S, Lewis K. Emergence of Pseudomonas aeruginosa strains producing high levels of persister cells in patients with cystic fibrosis. J Bacteriol. 2010;192(23):6191–9. https://doi.org/10.1128/JB.01651-09.
Breidenstein EBM, de la Fuente-Núñez C, Hancock REW. Pseudomonas aeruginosa: all roads lead to resistance. Trends Microbiol. 2011;19(8):419–26. https://doi.org/10.1016/j.tim.2011.04.005.
Chevalier S, Bouffartigues E, Bodilis J, et al. Structure, function and regulation of Pseudomonas aeruginosa porins. FEMS Microbiol Rev. 2017;41(5):698–722. https://doi.org/10.1093/femsre/fux020.
Meletis G, Bagkeri M. Pseudomonas aeruginosa: multi-drug-resistance development and treatment options. In: Basak S, editor. Infection control. London: InTech; 2013. https://doi.org/10.5772/55616.
Munita JM, Arias CA. Mechanisms of antibiotic resistance. Microbiol Spectr. 2016;4(2):15. https://doi.org/10.1128/microbiolspec.VMBF-0016-2015.
Sandoval-Motta S, Aldana M. Adaptive resistance to antibiotics in bacteria: a systems biology perspective. WIREs Syst Biol Med. 2016;8(3):253–67. https://doi.org/10.1002/wsbm.1335.
Taylor PK, Yeung ATY, Hancock REW. Antibiotic resistance in Pseudomonas aeruginosa biofilms: towards the development of novel anti-biofilm therapies. J Biotechnol. 2014;191:121–30. https://doi.org/10.1016/j.jbiotec.2014.09.003.
Fang ZL, Zhang LY, Huang YM, et al. OprD mutations and inactivation in imipenem-resistant Pseudomonas aeruginosa isolates from China. Infect Genet Evol. 2014;21:124–8. https://doi.org/10.1016/j.meegid.2013.10.027.
Dreier J, Ruggerone P. Interaction of antibacterial compounds with RND efflux pumps in Pseudomonas aeruginosa. Front Microbiol. 2015;6:660. https://doi.org/10.3389/fmicb.2015.00660.
Li H, Luo YF, Williams BJ, Blackwell TS, Xie CM. Structure and function of OprD protein in Pseudomonas aeruginosa: from antibiotic resistance to novel therapies. Int J Med Microbiol. 2012;302(2):63–8. https://doi.org/10.1016/j.ijmm.2011.10.001.
Dupont P, Hocquet D, Jeannot K, Chavanet P, Plésiat P. Bacteriostatic and bactericidal activities of eight fluoroquinolones against MexAB-OprM-overproducing clinical strains of Pseudomonas aeruginosa. J Antimicrob Chemother. 2005;55(4):518–22. https://doi.org/10.1093/jac/dki030.
Goli HR, Nahaei MR, Rezaee MA, et al. Contribution of mexAB-oprM and mexXY (-oprA) efflux operons in antibiotic resistance of clinical Pseudomonas aeruginosa isolates in Tabriz, Iran. Infect Genet Evol. 2016;45:75–82. https://doi.org/10.1016/j.meegid.2016.08.022.
Alcalde-Rico M, Olivares-Pacheco J, Alvarez-Ortega C, Cámara M, Martínez JL. Role of the multidrug resistance efflux pump MexCD-OprJ in the Pseudomonas aeruginosa quorum sensing response. Front Microbiol. 2018;9:2752. https://doi.org/10.3389/fmicb.2018.02752.
Fernández L, Hancock REW. Adaptive and mutational resistance: role of porins and efflux pumps in drug resistance. Clin Microbiol Rev. 2012;25(4):661–81. https://doi.org/10.1128/CMR.00043-12.
Tam VH, Chang KT, Zhou J, et al. Determining β-lactam exposure threshold to suppress resistance development in Gram-negative bacteria. J Antimicrob Chemother. 2017;72(5):1421–8. https://doi.org/10.1093/jac/dkx001.
Ortiz de la Rosa JM, Nordmann P, Poirel L. ESBLs and resistance to ceftazidime/avibactam and ceftolozane/tazobactam combinations in Escherichia coli and Pseudomonas aeruginosa. J Antimicrob Chemother. 2019;74(7):1934–9. https://doi.org/10.1093/jac/dkz149.
Hong DJ, Bae IK, Jang IH, Jeong SH, Kang HK, Lee K. Epidemiology and characteristics of metallo-β-lactamase-producing Pseudomonas aeruginosa. Infect Chemother. 2015;47(2):81–97. https://doi.org/10.3947/ic.2015.47.2.81.
Lee M, Abbey T, Biagi M, Wenzler E. Activity of aztreonam in combination with ceftazidime–avibactam against serine- and metallo-β-lactamase-producing Pseudomonas aeruginosa. Diagn Microbiol Infect Dis. 2021;99(1): 115227. https://doi.org/10.1016/j.diagmicrobio.2020.115227.
Berrazeg M, Jeannot K, Ntsogo Enguéné VY, et al. Mutations in β-lactamase AmpC increase resistance of Pseudomonas aeruginosa isolates to antipseudomonal cephalosporins. Antimicrob Agents Chemother. 2015;59(10):6248–55. https://doi.org/10.1128/AAC.00825-15.
Pang Z, Raudonis R, Glick BR, Lin TJ, Cheng Z. Antibiotic resistance in Pseudomonas aeruginosa: mechanisms and alternative therapeutic strategies. Biotechnol Adv. 2019;37(1):177–92. https://doi.org/10.1016/j.biotechadv.2018.11.013.
Rubio AM, Kline EG, Jones CE, et al. In vitro susceptibility of multidrug-resistant Pseudomonas aeruginosa following treatment-emergent resistance to ceftolozane-tazobactam. Antimicrob Agents Chemother. 2021;65(6):e00084-21. https://doi.org/10.1128/AAC.00084-21.
Bush K, Jacoby GA. Updated functional classification of β-lactamases. Antimicrob Agents Chemother. 2010;54(3):969–76. https://doi.org/10.1128/AAC.01009-09.
Henrichfreise B, Wiegand I, Pfister W, Wiedemann B. Resistance mechanisms of multiresistant Pseudomonas aeruginosa strains from Germany and correlation with hypermutation. Antimicrob Agents Chemother. 2007;51(11):4062–70. https://doi.org/10.1128/AAC.00148-07.
Ramirez MS, Tolmasky ME. Aminoglycoside modifying enzymes. Drug Resist Updat. 2010;13(6):151–71. https://doi.org/10.1016/j.drup.2010.08.003.
Yang X, Xing B, Liang C, Ye Z, Zhang Y. Prevalence and fluoroquinolone resistance of Pseudomonas aeruginosa in a hospital of South China. Int J Clin Exp Med. 2015;8(1):1386–90.
Rutherford ST, Bassler BL. Bacterial quorum sensing: its role in virulence and possibilities for its control. Cold Spring Harb Perspect Med. 2012;2(11):a012427. https://doi.org/10.1101/cshperspect.a012427.
Mukherjee S, Moustafa DA, Stergioula V, Smith CD, Goldberg JB, Bassler BL. The PqsE and RhlR proteins are an autoinducer synthase–receptor pair that control virulence and biofilm development in Pseudomonas aeruginosa. Proc Natl Acad Sci USA. 2018;115(40):E9411–8. https://doi.org/10.1073/pnas.1814023115.
Lewis K. Persister cells. Annu Rev Microbiol. 2010;64(1):357–72. https://doi.org/10.1146/annurev.micro.112408.134306.
Wood TK, Knabel SJ, Kwan BW. Bacterial persister cell formation and dormancy. Appl Environ Microbiol. 2013;79(23):7116–21. https://doi.org/10.1128/AEM.02636-13.
Mensa J, Barberán J, Soriano A, et al. Antibiotic selection in the treatment of acute invasive infections by Pseudomonas aeruginosa: guidelines by the Spanish Society of Chemotherapy. Rev Esp Quimioter. 2018;31(1):78–100.
Tamma PD, Cosgrove SE, Maragakis LL. Combination therapy for treatment of infections with gram-negative bacteria. Clin Microbiol Rev. 2012;25(3):450–70. https://doi.org/10.1128/CMR.05041-11.
Bassetti M, Vena A, Croxatto A, Righi E, Guery B. How to manage Pseudomonas aeruginosa infections. Drugs Context. 2018;7: 212527. https://doi.org/10.7573/dic.212527.
m100ed30_sample.pdf. https://clsi.org/media/3481/m100ed30_sample.pdf. Accessed 10 Nov 2021.
EUCAST: Clinical breakpoints and dosing of antibiotics. Published May 13, 2021. https://www.eucast.org/clinical_breakpoints/. Accessed 12 May 2021.
Antibacterial Susceptibility Test Interpretive Criteria. FDA. Published online October 14, 2021. https://www.fda.gov/drugs/development-resources/antibacterial-susceptibility-test-interpretive-criteria. Accessed 10 Nov 2021.
zerbaxa_pi.pdf. 2021. https://www.merck.com/product/usa/pi_circulars/z/zerbaxa/zerbaxa_pi.pdf. Accessed 01 Sep 2021.
Cho JC, Fiorenza MA, Estrada SJ. Ceftolozane/tazobactam: a novel cephalosporin/β-lactamase inhibitor combination. Pharmacotherapy. 2015;35(7):701–15. https://doi.org/10.1002/phar.1609.
Giancola SE, Mahoney MV, Bias TE, Hirsch EB. Critical evaluation of ceftolozane–tazobactam for complicated urinary tract and intra-abdominal infections. Ther Clin Risk Manag. 2016;12:787–97. https://doi.org/10.2147/TCRM.S83844.
Zhanel GG, Chung P, Adam H, et al. Ceftolozane/tazobactam: a novel cephalosporin/β-lactamase inhibitor combination with activity against multidrug-resistant gram-negative bacilli. Drugs. 2014;74(1):31–51. https://doi.org/10.1007/s40265-013-0168-2.
Haidar G, Philips NJ, Shields RK, et al. Ceftolozane-tazobactam for the treatment of multidrug-resistant Pseudomonas aeruginosa infections: clinical effectiveness and evolution of resistance. Clin Infect Dis. 2017;65(1):110–20. https://doi.org/10.1093/cid/cix182.
Solomkin J, Hershberger E, Miller B, et al. Ceftolozane/tazobactam plus metronidazole for complicated intra-abdominal infections in an era of multidrug resistance: results from a randomized, double-blind, phase 3 trial (ASPECT-cIAI). Clin Infect Dis. 2015;60(10):1462–71. https://doi.org/10.1093/cid/civ097.
Wagenlehner FM, Umeh O, Steenbergen J, Yuan G, Darouiche RO. Ceftolozane-tazobactam compared with levofloxacin in the treatment of complicated urinary-tract infections, including pyelonephritis: a randomised, double-blind, phase 3 trial (ASPECT-cUTI). Lancet Lond Engl. 2015;385(9981):1949–56. https://doi.org/10.1016/S0140-6736(14)62220-0.
Kollef MH, Nováček M, Kivistik Ü, et al. Ceftolozane-tazobactam versus meropenem for treatment of nosocomial pneumonia (ASPECT-NP): a randomised, controlled, double-blind, phase 3, non-inferiority trial. Lancet Infect Dis. 2019;19(12):1299–311. https://doi.org/10.1016/S1473-3099(19)30403-7.
Balandin B, Ballesteros D, Ruiz de Luna R, et al. Multicenter study of ceftolozane/tazobactam for treatment of Pseudomonas aeruginosa infections in critically ill patients. Int J Antimicrob Agents. 2021;57(3):106270. https://doi.org/10.1016/j.ijantimicag.2020.106270.
Puzniak L, Dillon R, Palmer T, Collings H, Enstone A. Real-world use of ceftolozane/tazobactam: a systematic literature review. Antimicrob Resist Infect Control. 2021;10(1):68. https://doi.org/10.1186/s13756-021-00933-8.
Rodríguez-Núñez O, Periañez-Parraga L, Oliver A, et al. Higher MICs (>2 mg/L) predict 30-day mortality in patients with lower respiratory tract infections caused by multidrug- and extensively drug-resistant Pseudomonas aeruginosa treated with ceftolozane/tazobactam. Open Forum Infect Dis. 2019;6(10): ofz416. https://doi.org/10.1093/ofid/ofz416.
Díaz-Cañestro M, Periañez L, Mulet X, et al. Ceftolozane/tazobactam for the treatment of multidrug resistant Pseudomonas aeruginosa: experience from the Balearic Islands. Eur J Clin Microbiol Infect Dis. 2018;37(11):2191–200. https://doi.org/10.1007/s10096-018-3361-0.
Pogue JM, Kaye KS, Veve MP, et al. Ceftolozane/tazobactam vs polymyxin or aminoglycoside-based regimens for the treatment of drug-resistant Pseudomonas aeruginosa. Clin Infect Dis. 2020;71(2):304–10. https://doi.org/10.1093/cid/ciz816.
Mills M, MacWhinnie A, Do T. 2286. Evaluating the impact of ceftolozane/tazobactam on clinical outcomes in patients with multi-drug-resistant Pseudomonas aeruginosa pneumonia. Open Forum Infect Dis. 2019;6(Suppl 2):S783–4. https://doi.org/10.1093/ofid/ofz360.1964.
Jorgensen SCJ, Trinh TD, Zasowski EJ, et al. Real-world experience with ceftolozane-tazobactam for multidrug-resistant gram-negative bacterial infections. Antimicrob Agents Chemother. 2020;64(4):e02291-e2319. https://doi.org/10.1128/AAC.02291-19.
Bassetti M, Castaldo N, Cattelan A, et al. Ceftolozane/tazobactam for the treatment of serious Pseudomonas aeruginosa infections: a multicentre nationwide clinical experience. Int J Antimicrob Agents. 2019;53(4):408–15. https://doi.org/10.1016/j.ijantimicag.2018.11.001.
Escolà-Vergé L, Pigrau C, Los-Arcos I, et al. Ceftolozane/tazobactam for the treatment of XDR Pseudomonas aeruginosa infections. Infection. 2018;46(4):461–8. https://doi.org/10.1007/s15010-018-1133-5.
Gallagher JC, Satlin MJ, Elabor A, et al. Ceftolozane-tazobactam for the treatment of multidrug-resistant Pseudomonas aeruginosa infections: a multicenter study. Open Forum Infect Dis. 2018;5(11): ofy280. https://doi.org/10.1093/ofid/ofy280.
Hart DE, Gallagher JC, Puzniak L, Hirsch EB. 2281. Ceftolozane–tazobactam (C/T) treatment outcomes in immunocompromised (IC) patients with multidrug-resistant (MDR) Pseudomonas aeruginosa (PA) infections. Open Forum Infect Dis. 2019. https://doi.org/10.1093/ofid/ofz360.1959.
Vena A, Giacobbe DR, Mussini C, Cattelan A, Bassetti M, Ceftabuse Study Group. Clinical efficacy of ceftolozane-tazobactam versus other active agents for the treatment of bacteremia and nosocomial pneumonia due to drug-resistant Pseudomonas aeruginosa. Clin Infect Dis. 2020;71(7):1799–801. https://doi.org/10.1093/cid/ciaa003.
Gill CM, Aktaþ E, Alfouzan W, et al. The ERACE-PA Global Surveillance Program: ceftolozane/tazobactam and ceftazidime/avibactam in vitro activity against a global collection of carbapenem-resistant Pseudomonas aeruginosa. Eur J Clin Microbiol Infect Dis. 2021. https://doi.org/10.1007/s10096-021-04308-0.
Livermore DM, Mushtaq S, Meunier D, et al. Activity of ceftolozane/tazobactam against surveillance and “problem” Enterobacteriaceae, Pseudomonas aeruginosa and non-fermenters from the British Isles. J Antimicrob Chemother. 2017;72(8):2278–89. https://doi.org/10.1093/jac/dkx136.
Fraile-Ribot PA, Cabot G, Mulet X, et al. Mechanisms leading to in vivo ceftolozane/tazobactam resistance development during the treatment of infections caused by MDR Pseudomonas aeruginosa. J Antimicrob Chemother. 2018;73(3):658–63. https://doi.org/10.1093/jac/dkx424.
Lahiri SD, Walkup GK, Whiteaker JD, et al. Selection and molecular characterization of ceftazidime/avibactam-resistant mutants in Pseudomonas aeruginosa strains containing derepressed AmpC. J Antimicrob Chemother. 2015;70(6):1650–8. https://doi.org/10.1093/jac/dkv004.
Karlowsky JA, Lob SH, Kazmierczak KM, Young K, Motyl MR, Sahm DF. In vitro activity of imipenem/relebactam against Enterobacteriaceae and Pseudomonas aeruginosa isolated from intraabdominal and urinary tract infection samples: SMART Surveillance United States 2015–2017. J Glob Antimicrob Resist. 2020;21:223–8. https://doi.org/10.1016/j.jgar.2019.10.028.
Lob SH, Karlowsky JA, Young K, et al. In vitro activity of imipenem-relebactam against resistant phenotypes of Enterobacteriaceae and Pseudomonas aeruginosa isolated from intraabdominal and urinary tract infection samples SMART Surveillance Europe 2015–2017. J Med Microbiol. 2020;69(2):207–17. https://doi.org/10.1099/jmm.0.001142.
Iregui A, Khan Z, Landman D, Quale J. Activity of cefiderocol against Enterobacterales, Pseudomonas aeruginosa, and Acinetobacter baumannii endemic to medical centers in New York City. Microb Drug Resist. 2020;26(7):722–6. https://doi.org/10.1089/mdr.2019.0298.
Hidalgo JA, Vinluan CM, Antony N. Ceftazidime/avibactam: a novel cephalosporin/nonbeta-lactam beta-lactamase inhibitor for the treatment of complicated urinary tract infections and complicated intra-abdominal infections. Drug Des Devel Ther. 2016;10:2379–86. https://doi.org/10.2147/DDDT.S110946.
Ehmann DE, Jahić H, Ross PL, et al. Avibactam is a covalent, reversible, non-β-lactam β-lactamase inhibitor. Proc Natl Acad Sci. 2012;109(29):11663–8. https://doi.org/10.1073/pnas.1205073109.
Stachyra T, Péchereau MC, Bruneau JM, et al. Mechanistic studies of the inactivation of TEM-1 and P99 by NXL104, a novel non-β-lactam β-lactamase inhibitor. Antimicrob Agents Chemother. 2010;54(12):5132–8. https://doi.org/10.1128/AAC.00568-10.
Poirel L, Ortiz De La Rosa JM, Kieffer N, Dubois V, Jayol A, Nordmann P. Acquisition of extended-spectrum β-lactamase GES-6 leading to resistance to ceftolozane-tazobactam combination in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2018;63(1):18. https://doi.org/10.1128/AAC.01809-18.
Criscuolo M, Trecarichi EM. Ceftazidime/avibactam and ceftolozane/tazobactam for multidrug-resistant gram negatives in patients with hematological malignancies: current experiences. Antibiotics. 2020;9(2):58. https://doi.org/10.3390/antibiotics9020058.
Jorgensen SCJ, Trinh TD, Zasowski EJ, et al. Real-world experience with ceftazidime-avibactam for multidrug-resistant gram-negative bacterial infections. Open Forum Infect Dis. 2019. https://doi.org/10.1093/ofid/ofz522.
Stone GG, Newell P, Gasink LB, et al. Clinical activity of ceftazidime/avibactam against MDR Enterobacteriaceae and Pseudomonas aeruginosa: pooled data from the ceftazidime/avibactam phase III clinical trial programme. J Antimicrob Chemother. 2018;73(9):2519–23. https://doi.org/10.1093/jac/dky204.
Wang Y, Wang J, Wang R, Cai Y. Resistance to ceftazidime–avibactam and underlying mechanisms. J Glob Antimicrob Resist. 2020;22:18–27. https://doi.org/10.1016/j.jgar.2019.12.009.
Winkler ML, Papp-Wallace KM, Hujer AM, et al. Unexpected challenges in treating multidrug-resistant gram-negative bacteria: resistance to ceftazidime-avibactam in archived isolates of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2015;59(2):1020–9. https://doi.org/10.1128/AAC.04238-14.
Mikhail S, Singh NB, Kebriaei R, et al. Evaluation of the synergy of ceftazidime-avibactam in combination with meropenem, amikacin, aztreonam, colistin, or fosfomycin against well-characterized multidrug-resistant Klebsiella pneumoniae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2019;63(8):e00779-e819. https://doi.org/10.1128/AAC.00779-19.
Papp-Wallace KM, Zeiser ET, Becka SA, et al. Ceftazidime-avibactam in combination with fosfomycin: a novel therapeutic strategy against multidrug-resistant Pseudomonas aeruginosa. J Infect Dis. 2019;220(4):666–76. https://doi.org/10.1093/infdis/jiz149.
FDA. FDA approves new treatment for complicated urinary tract and complicated intra-abdominal infections. FDA. Published July 17, 2019. https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-complicated-urinary-tract-and-complicated-intra-abdominal-infections. Accessed 23 Sep 2021.
FDA. FDA approves antibiotic to treat hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia. FDA. Published June 5, 2020. https://www.fda.gov/news-events/press-announcements/fda-approves-antibiotic-treat-hospital-acquired-bacterial-pneumonia-and-ventilator-associated. Accessed 23 Sep 2021.
Zhanel GG, Lawrence CK, Adam H, et al. Imipenem-relebactam and meropenem-vaborbactam: two novel carbapenem-β-lactamase inhibitor combinations. Drugs. 2018;78(1):65–98. https://doi.org/10.1007/s40265-017-0851-9.
Young K, Painter RE, Raghoobar SL, et al. In vitro studies evaluating the activity of imipenem in combination with relebactam against Pseudomonas aeruginosa. BMC Microbiol. 2019;19(1):150. https://doi.org/10.1186/s12866-019-1522-7.
Motsch J, Murta Oliveira C, Stus V, et al. RESTORE-IMI 1: a multicenter, randomized, double-blind trial comparing efficacy and safety of imipenem/relebactam vs colistin plus imipenem in patients with imipenem-nonsusceptible bacterial infections. Clin Infect Dis. 2020;70(9):1799–808. https://doi.org/10.1093/cid/ciz530.
Clinical and Laboratory Standards Institute. M100: performance standards for antimicrobial susceptibility testing. 31st ed. Washington: CLSI; 2021.
Lapuebla A, Abdallah M, Olafisoye O, et al. Activity of imipenem with relebactam against gram-negative pathogens from New York City. Antimicrob Agents Chemother. 2015;59(8):5029–31. https://doi.org/10.1128/AAC.00830-15.
Fraile-Ribot PA, Zamorano L, Orellana R, et al. Activity of imipenem-relebactam against a large collection of Pseudomonas aeruginosa clinical isolates and isogenic β-lactam-resistant mutants. Antimicrob Agents Chemother. 2020;64(2):e02165-e2219. https://doi.org/10.1128/AAC.02165-19.
In vitro activity of cefiderocol, a siderophore cephalosporin, against a recent collection of clinically relevant carbapenem-non-susceptible Gram-negative bacilli, including serine carbapenemase- and metallo-β-lactamase-producing isolates (SIDERO-WT-2014 Study) - ClinicalKey. 2021. https://www.clinicalkey.com/#!/content/playContent/1-s2.0-S0924857918302991?returnurl=https:%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0924857918302991%3Fshowall%3Dtrue&referrer=https:%2F%2Fpubmed.ncbi.nlm.nih.gov%2F. Accessed 30 Aug 2021.
Yamano Y. In vitro activity of cefiderocol against a broad range of clinically important gram-negative bacteria. Clin Infect Dis. 2019;69(Supplement_7):S544–51. https://doi.org/10.1093/cid/ciz827.
Hackel MA, Tsuji M, Yamano Y, Echols R, Karlowsky JA, Sahm DF. In vitro activity of the siderophore cephalosporin, cefiderocol, against carbapenem-nonsusceptible and multidrug-resistant isolates of gram-negative bacilli collected worldwide in 2014 to 2016. Antimicrob Agents Chemother. 2018;62(2):e01968-17. https://doi.org/10.1128/AAC.01968-17.
Streling AP, Al Obaidi MM, Lainhart WD, et al. Evolution of cefiderocol non-susceptibility in Pseudomonas aeruginosa in a patient without previous exposure to the antibiotic. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciaa1909.
Ito A, Nishikawa T, Ishii R, et al. 696. Mechanism of cefiderocol high MIC mutants obtained in non-clinical FoR studies. Open Forum Infect Dis. 2018;5(1):S251. https://doi.org/10.1093/ofid/ofy210.703.
Lyczak JB, Cannon CL, Pier GB. Lung infections associated with cystic fibrosis. Clin Microbiol Rev. 2002;15(2):194–222. https://doi.org/10.1128/CMR.15.2.194-222.2002.
Davies JC. Pseudomonas aeruginosa in cystic fibrosis: pathogenesis and persistence. Paediatr Respir Rev. 2002;3(2):128–34. https://doi.org/10.1016/s1526-0550(02)00003-3.
Gibson RL, Burns JL, Ramsey BW. Pathophysiology and management of pulmonary infections in cystic fibrosis. Am J Respir Crit Care Med. 2003;168(8):918–51. https://doi.org/10.1164/rccm.200304-505SO.
Colbert B, Kumari H, Piñon A, Frey L, Pandey S, Mathee K. Alginate-regulating genes are identified in the clinical cystic fibrosis isolate of Pseudomonas aeruginosa PA2192. bioRxiv. 2018;5:319004. https://doi.org/10.1101/319004.
Pier GB, Coleman F, Grout M, Franklin M, Ohman DE. Role of alginate O acetylation in resistance of mucoid Pseudomonas aeruginosa to opsonic phagocytosis. Infect Immun. 2001;69(3):1895–901. https://doi.org/10.1128/IAI.69.3.1895-1901.2001.
Boucher JC, Yu H, Mudd MH, Deretic V. Mucoid Pseudomonas aeruginosa in cystic fibrosis: characterization of muc mutations in clinical isolates and analysis of clearance in a mouse model of respiratory infection. Infect Immun. 1997;65(9):3838–46.
Pulcrano G, Iula DV, Raia V, Rossano F, Catania MR. Different mutations in mucA gene of Pseudomonas aeruginosa mucoid strains in cystic fibrosis patients and their effect on algU gene expression. New Microbiol. 2012;35(3):295–305.
American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416. https://doi.org/10.1164/rccm.200405-644ST.
Saiman L, Mehar F, Niu WW, et al. Antibiotic susceptibility of multiply resistant Pseudomonas aeruginosa isolated from patients with cystic fibrosis, including candidates for transplantation. Clin Infect Dis. 1996;23(3):532–7. https://doi.org/10.1093/clinids/23.3.532.
Weiss K, Lapointe JR. Routine susceptibility testing of four antibiotic combinations for improvement of laboratory guide to therapy of cystic fibrosis infections caused by Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1995;39(11):2411–4.
Watkins J, Francis J, Kuzemko JA. Does monotherapy of pulmonary infections in cystic fibrosis lead to early development of resistant strains of Pseudomonas aeruginosa! Scand J Gastroenterol. 1988;23(sup143):81–5. https://doi.org/10.3109/00365528809090223.
Döring G, Conway SP, Heijerman HGM, et al. Antibiotic therapy against Pseudomonas aeruginosa in cystic fibrosis: a European consensus. Eur Respir J. 2000;16(4):749. https://doi.org/10.1034/j.1399-3003.2000.16d30.x.
Nolan PJ, Jain R, Cohen L, Finklea JD, Smith TT. In vitro activity of ceftolozane-tazobactam and ceftazidime-avibactam against Pseudomonas aeruginosa isolated from patients with cystic fibrosis. Diagn Microbiol Infect Dis. 2021;99(2): 115204. https://doi.org/10.1016/j.diagmicrobio.2020.115204.
Sader HS, Duncan LR, Doyle TB, Castanheira M. Antimicrobial activity of ceftazidime/avibactam, ceftolozane/tazobactam and comparator agents against Pseudomonas aeruginosa from cystic fibrosis patients. JAC Antimicrob Resist. 2021;4(3):dlab126. https://doi.org/10.1093/jacamr/dlab126.
Kutter E, Sulakvelidze A, editors. Bacteriophages: biology and applications. London: CRC; 2005.
Duckworth DH. Who discovered bacteriophage? Bacteriol Rev. 1976;40(4):793–802.
Kutter E, De Vos D, Gvasalia G, et al. Phage therapy in clinical practice: treatment of human infections. Curr Pharm Biotechnol. 2010;11(1):69–86. https://doi.org/10.2174/138920110790725401.
Gupta P, Singh HS, Shukla VK, Nath G, Bhartiya SK. Bacteriophage therapy of chronic nonhealing wound: clinical study. Int J Low Extrem Wounds. 2019;18(2):171–5. https://doi.org/10.1177/1534734619835115.
Markoishvili K, Tsitlanadze G, Katsarava R, Glenn J, Sulakvelidze A. A novel sustained-release matrix based on biodegradable poly(ester amide)s and impregnated with bacteriophages and an antibiotic shows promise in management of infected venous stasis ulcers and other poorly healing wounds. Int J Dermatol. 2002;41(7):453–8. https://doi.org/10.1046/j.1365-4362.2002.01451.x.
Aslam S, Lampley E, Wooten D, et al. Lessons learned from the first 10 consecutive cases of intravenous bacteriophage therapy to treat multidrug-resistant bacterial infections at a single center in the United States. Open Forum Infect Dis. 2022. https://academic.oup.com/ofid/article/7/9/ofaa389/5898206. Accessed 04 Jan 2022.
Levin BR, Bull JJ. Population and evolutionary dynamics of phage therapy. Nat Rev Microbiol. 2004;2(2):166–73.
Jault P, Leclerc T, Jennes S, et al. Efficacy and tolerability of a cocktail of bacteriophages to treat burn wounds infected by Pseudomonas aeruginosa (PhagoBurn): a randomised, controlled, double-blind phase 1/2 trial. Lancet Infect Dis. 2019;19:35–45.
Payne RJ, Phil D, Jansen VA. Phage therapy: the peculiar kinetics of self-replicating pharmaceuticals. Clin Pharmacol Ther. 2000;68(3):225–30. https://doi.org/10.1067/mcp.2000.109520.
Antoine C, Laforêt F, Blasdel B, et al. Efficacy assessment of PEV2 phage on Galleria mellonella larvae infected with a Pseudomonas aeruginosa dog otitis isolate. Res Vet Sci. 2021;136:598–601. https://doi.org/10.1016/j.rvsc.2021.04.010.
Chang RYK, Das T, Manos J, Kutter E, Morales S, Chan HK. Bacteriophage PEV20 and ciprofloxacin combination treatment enhances removal of Pseudomonas aeruginosa biofilm isolated from cystic fibrosis and wound patients. AAPS J. 2019;21(3):49. https://doi.org/10.1208/s12248-019-0315-0.
Law N, Logan C, Yung G, et al. Successful adjunctive use of bacteriophage therapy for treatment of multidrug-resistant Pseudomonas aeruginosa infection in a cystic fibrosis patient. Infection. 2019;47(4):665–8. https://doi.org/10.1007/s15010-019-01319-0.
Chan BK, Sistrom M, Wertz JE, Kortright KE, Narayan D, Turner PE. Phage selection restores antibiotic sensitivity in MDR Pseudomonas aeruginosa. Sci Rep. 2016;6:26717. https://doi.org/10.1038/srep26717.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work, and have given their approval for this version to be published.
Author Contributions
Ashlan J. Kunz Coyne drafted the main portion of the manuscript, Amer El Ghali, Dana Holger, and Nicholas Rebold contributed to parts of the manuscript, Michael J. Rybak provided support and conceptual advice at all stages of manuscript preparation. All authors commented on and revised previous versions of the manuscript. All authors read and approve the final manuscript.
Disclosures
Michael J. Rybak has received research support, consulted, or has spoken on behalf of Merck, Shionogi, and AbbVie. Ashlan J. Kunz Coyne, Amer El Ghali, Dana Holger, and Nicholas Rebold declare that they have no conflict of interest.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kunz Coyne, A.J., El Ghali, A., Holger, D. et al. Therapeutic Strategies for Emerging Multidrug-Resistant Pseudomonas aeruginosa. Infect Dis Ther 11, 661–682 (2022). https://doi.org/10.1007/s40121-022-00591-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00591-2