Abstract
Introduction
AKCEA-TTR-LRx is a ligand-conjugated antisense (LICA) drug in development for the treatment of hereditary transthyretin amyloidosis (hATTR), a fatal disease caused by mutations in the transthyretin (TTR) gene. AKCEA-TTR-LRx shares the same nucleotide sequence as inotersen, an antisense medicine approved for use in hATTR polyneuropathy (hATTR-PN). Unlike inotersen, AKCEA-TTR-LRx is conjugated to a triantennary N-acetylgalactosamine moiety that supports receptor-mediated uptake by hepatocytes, the primary source of circulating TTR. This advanced design increases drug potency to allow for lower and less frequent dosing. The NEURO-TTRansform study will investigate whether AKCEA-TTR-LRx is safe and efficacious, with the aim of improving neurologic function and quality of life in hATTR-PN patients.
Methods/Design
Approximately 140 adults with stage 1 (independent ambulation) or 2 (requires ambulatory support) hATTR-PN are anticipated to enroll in this multicenter, open-label, randomized, phase 3 study. Patients will be assigned 6:1 to AKCEA-TTR-LRx 45 mg subcutaneously every 4 weeks or inotersen 300 mg once weekly until the prespecified week 35 interim efficacy analysis, after which patients receiving inotersen will receive AKCEA-TTR-LRx 45 mg subcutaneously every 4 weeks. All patients will then receive AKCEA-TTR-LRx through the remainder of the study treatment period. The final efficacy analysis at week 66 will compare the AKCEA-TTR-LRx arm with the historical placebo arm from the phase 3 trial of inotersen (NEURO-TTR). The primary outcome measures are between-group differences in the change from baseline in serum TTR, modified Neuropathy Impairment Score + 7, and Norfolk Quality of Life—Diabetic Neuropathy questionnaire.
Conclusion
NEURO-TTRansform is designed to determine whether targeted delivery of AKCEA-TTR-LRx to hepatocytes with lower and less frequent doses will translate into clinical and quality-of-life benefits for patients with hATTR-PN.
Trial Registration
The study is registered at ClinicalTrials.gov (NCT04136184) and EudraCT (2019-001698-10).
Plain Language Summary
-
Hereditary transthyretin amyloidosis with peripheral neuropathy (hATTR-PN for short) is a rare inherited condition.
-
In hATTR-PN, a protein called transthyretin (TTR for short) builds up and damages nerves throughout the body.
-
This neuropathy causes symptoms such as weakness, loss of sensation, and pain.
-
-
Currently available medicines can slow disease progression, but researchers are looking for more effective treatments with fewer side effects.
-
AKCEA-TTR-LRx is an investigational treatment for hATTR-PN.
-
AKCEA-TTR-LRx prevents the liver from making TTR, reducing the amount that causes disease progression.
-
It is similar to an existing treatment called inotersen, but designed for better delivery to the liver and is more potent.
-
-
This article describes the NEURO-TTRansform study that will evaluate how effective AKCEA-TTR-LRx is for treating hATTR-PN.
-
Around 140 adults with hATTR-PN from the USA, Canada, and Europe will be able to take part in this study.
-
The study treatment period will be 85 weeks long. People will receive injections underneath the skin of either:
-
AKCEA-TTR-LRx every 4 weeks, or
-
Inotersen once a week for 35 weeks, followed by a switch to AKCEA-TTR-LRx every 4 weeks.
-
-
People may continue to receive AKCEA-TTR-LRx after the study treatment period ends.
-
-
In this study, researchers will compare results from people who received AKCEA-TTR-LRx to results from people who received no active ingredients (called placebo) in a similar study (called NEURO-TTR).
-
Researchers will measure the differences in peoples’:
-
Neuropathy symptoms.
-
Quality of life.
-
TTR protein levels in the blood.
-
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Hereditary transthyretin amyloidosis (hATTR) is a fatal disease caused by mutations in the transthyretin (TTR) gene that result in the synthesis of unstable TTR tetramers and consequent systemic deposition of insoluble amyloid fibrils, which most often manifest as cardiomyopathy or polyneuropathy (hATTR-PN). |
Although existing treatments can slow or halt neurologic impairment associated with hATTR-PN, there remains a need for other disease-modifying agents that offer improved efficacy, safety, and convenience of use. |
AKCEA-TTR-LRx is a novel antisense oligonucleotide (ASO) designed for enhanced delivery to hepatocytes, the primary site of TTR protein production, for increased potency and convenience of use to potentially translate into clinical and quality-of-life benefits for patients with hATTR-PN. |
This paper describes the design and rationale of the NEURO-TTRansform trial, a multicenter, open-label, randomized, phase 3 study that aims to assess the efficacy and safety of AKCEA-TTR-LRx in approximately 140 adult patients with stage 1 (independent ambulation) or 2 (requiring ambulatory support) hATTR-PN. |
Digital Features
This article is published with digital features, including a summary slide and a plain language summary, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13677805.
Introduction
Hereditary transthyretin amyloidosis (hATTR) is a progressive, irreversible, and fatal autosomal dominant disorder that manifests most commonly as peripheral sensorimotor and autonomic axonal neuropathy or infiltrative cardiomyopathy [1,2,3,4]. hATTR is caused by transthyretin (TTR) gene mutations that result in the synthesis of unstable TTR tetramers [5, 6]. TTR tetramers consisting of mutant TTR monomers are more susceptible to tetramer dissociation and consequent misfolding of the monomer, resulting in aggregation into soluble oligomeric structures and insoluble TTR-derived amyloid deposits [7, 8]. The accumulation of TTR-derived amyloid fibrils in multiple organ systems results in a wide spectrum of clinical manifestations [1, 2]. TTR genotype–phenotype correlations have been reported for a predominant clinical phenotype; for example, pV142I mutation carriers manifest preferentially with hATTR cardiomyopathy, whereas pV50M mutation carriers manifest preferentially with hATTR polyneuropathy (hATTR-PN) [9,10,11,12]. Additionally, factors that contribute to the rate of progression, such as geographic location, sex of transmitting parent, genetic anticipation, and genetic modifiers, are associated with the variability of the clinical presentation [11,12,13]. Estimates suggest that the global prevalence of hATTR-PN is approximately 10,000 patients, although many individuals may be undiagnosed [14]. The median age of onset of hATTR-PN varies geographically (from 33 years in Japan and Portugal to 56 years in Sweden), and patients progress to death 6–12 years after symptom onset [1, 2, 15, 16].
Clinical staging of hATTR-PN is often based on ambulatory status, which assesses the progression of sensorimotor axonal peripheral neuropathy severity. Disease metrics include the Familial Amyloid Polyneuropathy or Coutinho stage scoring system, and the Polyneuropathy Disability (PND) Score [1]. For the Coutinho scoring system, stage 1 is characterized by independent ambulation, stage 2 is characterized by the need for unilateral or bilateral support for ambulation, and stage 3 is characterized by being wheelchair-bound or bedridden [1].
Since the TTR protein is primarily produced by the liver, liver transplant has been the historical standard of care, acting to slow or halt disease progression by replacing a liver that produces mutant TTR protein with one that expresses only wild-type TTR [1]. Owing to donor shortages and progressive end-organ amyloid disease following liver transplantation, medical therapies have been pursued [1]. Over the past 13 years, several pharmacologic therapies have been developed, including TTR-stabilizing agents that preserve the tetrameric structure and ribonucleic acid (RNA)-targeting therapeutics that suppress TTR messenger RNA (mRNA) expression (Table 1). Oral tafamidis meglumine is a TTR-stabilizing agent that was approved for the treatment of familial amyloid polyneuropathy (FAP) stage 1 ATTR-PN in 2011 by the European Union, with subsequent approvals in Japan and other countries [17,18,19]. Diflunisal, a nonsteroidal anti-inflammatory drug, has been shown to significantly reduce the progression of neurological impairment among patients with hATTR-PN but is not approved for the treatment of hATTR-PN [20, 21]. With regard to RNA-targeting therapeutics, two treatments have recently been approved in the United States, the European Union, and other countries for patients with hATTR-PN: inotersen and patisiran [22,23,24,25]. Inotersen is an antisense oligonucleotide (ASO) inhibitor of TTR production, which is administered at a dosage of 300 mg by subcutaneous (SC) injection once weekly [24, 25]. Patisiran is a small interfering RNA (siRNA) inhibitor of TTR production, which is formulated in a lipid nanoparticle for administration at a dosage of 0.3 mg/kg by intravenous infusion every 3 weeks and requires premedication with a corticosteroid [22, 23].
Inotersen is approved for the treatment of adult patients with hATTR-PN [24, 25]. Inotersen binds to and induces ribonuclease H1-mediated degradation of TTR mRNA (wild-type and all known mutations), thereby lowering TTR protein production [21]. NEURO-TTR was a pivotal randomized, double-blind, placebo-controlled phase 2/3 study of inotersen 300 mg/week over 15 months in adult patients with stage 1 or stage 2 hATTR-PN [26]. Compared with placebo, inotersen significantly improved outcomes on the modified Neuropathy Impairment Score + 7 (mNIS + 7) and patient-reported Norfolk Quality of Life—Diabetic Neuropathy (Norfolk QOL-DN) questionnaire [26]. The maximum mean reduction from baseline in serum TTR was 74% [26]. The safety profile of inotersen was considered acceptable with regular safety laboratory assessments for thrombocytopenia and glomerulonephritis [24,25,26]. Although the approved treatments can slow or halt the neurologic impairment associated with hATTR-PN, there remains a need for more efficacious disease-modifying agents that offer a higher degree of TTR silencing, greater convenience of use, and a more favorable safety profile [26].
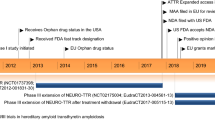
AKCEA-TTR-LRx (ION-682884) is a ligand-conjugated antisense (LICA) drug designed for preferential delivery to hepatocytes, the primary source of systemically circulating TTR (Fig. 1). This advanced antisense design utilizes a triantennary N-acetylgalactosamine (GalNAc) moiety to support productive receptor-mediated uptake by the high-capacity asialoglycoprotein receptors (ASGPR) expressed by hepatocytes [27, 28]. An integrated analysis of eight GalNAc-conjugated ASOs tested in phase 1 randomized placebo-controlled studies of healthy human volunteers showed a 20–30-fold increase in potency compared with the parent unconjugated ASOs [27]. Notably, these GalNAc-conjugated ASOs were well tolerated, with no discontinuations due to adverse events (AEs) [27].
ASGPR mediates the uptake of the GalNAc3-conjugated ASO AKCEA-TTR-LRx by hepatocytes, where it binds to the TTR mRNA through Watson–Crick hybridization and prevents production of TTR protein via RNase H1-mediated degradation of the target TTR mRNA. ASGPR asialoglycoprotein receptor, ASO antisense oligonucleotide, DNA deoxyribonucleic acid, mRNA messenger ribonucleic acid, RNase ribonuclease, TTR transthyretin
AKCEA-TTR-LRx is a GalNAc-conjugated ASO with a nucleotide sequence identical to inotersen, but with fewer phosphorothioate-modified internucleotide linkages, which is expected to improve its safety profile. Results from a first-in-human phase 1 study of AKCEA-TTR-LRx in healthy volunteers demonstrated that AKCEA-TTR-LRx 45 mg SC once every 4 weeks produced sustained decreases in serum TTR levels within 30 days of treatment initiation, achieving a mean reduction from baseline of 86% after four doses of treatment [29]. No treatment-related safety or tolerability issues were identified under this dosing regimen. Consequently, AKCEA-TTR-LRx requires a lower dose and less frequent administration (45 mg SC every 4 weeks, a 27-fold reduction in monthly exposure) than the unconjugated ASO, inotersen, to achieve a similar (if not better) pharmacological effect [26, 29, 30].
NEURO-TTRansform is a global, open-label, randomized phase 3 study that aims to evaluate the efficacy and safety of AKCEA-TTR-LRx in patients with hATTR-PN. This paper describes the rationale and the design of the trial.
Methods
Study Design
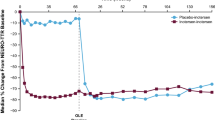
NEURO-TTRansform (EudraCT: 2019-001698-10; ClinicalTrials.gov: NCT04136184; ION-682884-CS3) is a phase 3 multicenter, open-label, randomized study of patients with stage 1 or stage 2 hATTR-PN assigned to receive AKCEA-TTR-LRx or an active reference arm (inotersen; Fig. 2). The primary aim is to evaluate the efficacy of AKCEA-TTR-LRx in patients with hATTR-PN relative to the historical placebo control arm of the NEURO-TTR trial [26]. The primary endpoints include the percentage change from baseline in serum TTR, change from baseline in mNIS + 7, and Norfolk QOL-DN score (Fig. 3). Key efficacy endpoints will be assessed at week 35 (interim analysis), week 66 (final efficacy analysis), and week 85. The secondary aims are to evaluate the efficacy of AKCEA-TTR-LRx relative to the historical placebo group with respect to the Neuropathy Symptom and Change (NSC) score, Physical Component Summary (PCS) score of the 36-Item Short-Form Health Survey (SF-36), PND score, and modified body mass index (mBMI; Fig. 3). AE monitoring and safety laboratory assessment will be performed throughout the trial. Discontinuation of study drug will occur immediately if the patient becomes pregnant, receives a major organ transplantation, or presents with predefined laboratory test abnormalities.
NEURO-TTRansform study design. EOT end of treatment, hATTR-PN hereditary transthyretin-mediated amyloid polyneuropathy, SC subcutaneously. aThe screening period is ≤ 6 weeks (or ≤ 10 weeks if genetic testing is required). bConcomitant therapy with tafamidis or off-label use of diflunisal is not allowed. Doxycycline use for the indication of infection (< 15 days) is allowed. cPatients not participating in the open-label extension will enter a 20-week post-treatment evaluation after completing EOT assessments. dPlacebo arm of the NEURO-TTR study (NCT01737398)
NEURO-TTRansform study endpoints. 10MWT 10-min walk test, COMPASS-31 Composite Autonomic Symptom Score-31, ECHO echocardiogram, EQ-5D-5L 5-level EuroQol 5-dimension, EOT end of treatment, mBMI modified body mass index, mNIS + 7 modified Neuropathy Impairment Score + 7, Norfolk QOL-DN Norfolk Quality of Life Questionnaire—Diabetic Neuropathy, NSC Neuropathy Symptom and Change, NT-proBNP N-terminal pro-brain natriuretic peptide, PCS Physical Component Summary, PND Polyneuropathy Disability Score, R-ODS Rasch-built Overall Disability Score, SC subcutaneously, SF-36 36-Item Short-Form Health Survey, TTR transthyretin. aPercentage change. bThe mNIS + 7 assessment procedure includes: Neuropathy Impairment Score, quantitative sensory testing, heart rate response to deep breathing, and predetermined sensory and nerve conduction testing. Additional clinical evaluations done during mNIS + 7 assessment include: lower limbs function test and NSC. cweeks 35 and 66. dweek 65. eweek 37. fweek 35. gweek 81. hVital signs, body weight, physical examination, clinical laboratory tests, electrocardiogram, use of concomitant medication, thyroid panel, inflammatory panel, coagulation, immunogenicity test
Patients will be randomized 6:1 to receive SC injections of either AKCEA-TTR-LRx (n ≈ 120) 45 mg every 4 weeks or inotersen (n ≈ 20) 300 mg once per week. As the analyses will utilize comparisons to the external placebo control arm of the NEURO-TTR trial, the inotersen reference arm is intended to ensure that no gross differences in patient population and response exist between the NEURO-TTR and the current study. Patients in the reference inotersen arm will be switched to receive AKCEA-TTR-LRx at week 37. All patients will then continue receiving treatment with AKCEA-TTR-LRx through week 81, with end-of-treatment (EOT) assessments at week 85, 4 weeks after the last dose. Following treatment and EOT assessments, patients will be eligible to enter an open-label extension study to continue receiving AKCEA-TTR-LRx once every 4 weeks or enter a 20-week post-treatment evaluation period.
The distribution of patients according to the disease stage will mirror the NEURO-TTR trial. Patients will also take supplemental doses of the recommended daily allowance of vitamin A to ensure adequate delivery of vitamin A to tissues in a setting of low serum TTR.
The study protocol and amendments have been approved by the relevant local institutional review boards (IRBs) or ethics committees (ECs) for currently activated clinical study sites. Activation of additional clinical study sites is ongoing, and the study protocol and amendments will be approved by the relevant local IRBs/ECs before participants are allowed to enroll in the study. The full list of IRB/EC names and approval numbers is available upon request. The study is being conducted according to the International Conference on Harmonisation guidelines and relevant country-specific laws. All participants must provide written informed consent prior to study inclusion. A data and safety monitoring board will periodically review safety, tolerability, and efficacy data relating to AKCEA-TTR-LRx and inotersen, including the results of the prespecified interim analysis at week 35.
Study Population
NEURO-TTRansform will enroll approximately 140 patients from ~ 70 clinical research sites in 15 countries. Adults aged 18–82 years are eligible for enrollment if they have stage 1 or stage 2 hATTR-PN, a documented TTR mutation, and signs and symptoms consistent with polyneuropathy (including an NIS ≥ 10 and ≤ 130). Key inclusion and exclusion criteria are shown in Fig. 4, and a complete list can be found in Table S1 in the supplementary material. Patients who have had a liver or heart transplant are ineligible. Any medications deemed necessary by the investigator are allowed, although concomitant tafamidis, inotersen, patisiran, or off-label use of diflunisal or doxycycline are not permitted. Patients who have received prior treatment with inotersen or patisiran are not eligible; patients previously treated with tafamidis, diflunisal, or doxycycline are eligible as long as these medications were discontinued at least 2 weeks prior to initiation of study treatment (day 1).
Key inclusion and exclusion criteria for the NEURO-TTRansform study. ASO antisense oligonucleotide, eGFR estimated glomerular filtration rate, FAP familial amyloid polyneuropathy, hATTR-PN hereditary transthyretin-mediated amyloid polyneuropathy, NIS Neuropathy Impairment Score, NYHA New York Heart Association, siRNA small interfering ribonucleic acid, TTR transthyretin, UPCR urine protein/creatinine ratio. aStage 1 (ambulatory without assistance) or stage 2 (ambulatory with assistance). bIn the event of UPCR ≥ 1000 mg/g, eligibility may be confirmed by a repeat random urine test with UPCR < 1000 mg/g or a quantitative total urine protein measurement of < 1000 mg/24 h. cChronic Kidney Disease Epidemiology Collaboration equation 1 formula
Planned Outcomes
Co-primary endpoints at the week 35 interim analysis include percentage change from baseline to week 35 in serum TTR levels and change from baseline in mNIS + 7 (Fig. 3). Co-primary endpoints at the week 66 final analysis are the same as those for the week 35 interim analysis, but also include change from baseline in Norfolk QOL-DN score.
Secondary efficacy, safety, and exploratory endpoints measured at weeks 35, 66, and 85 (EOT) are shown in Fig. 3. The week 35 interim analysis key secondary endpoint is change from baseline to week 35 in the Norfolk QOL-DN score. The final analysis secondary endpoints will include NSC score at weeks 35 and 66, and SF-36 PCS score, PND score, and mBMI at week 65. Non-compartmental pharmacokinetic analysis of AKCEA-TTR-LRx or inotersen will be carried out on each individual patient data set in the pharmacokinetic subgroup, where plasma samples are collected following drug administration on days 1, 225, and 449.
All treatment-emergent AEs, serious AEs, and reasons for any withdrawals will be summarized for each treatment group using the Medical Dictionary for Regulatory Activities coding system, by system organ class, preferred term, relationship to AKCEA-TTR-LRx or inotersen, and severity. AEs of special interest (including serious or nonserious events) are severe reductions in platelet count (< 50 × 109/L) accompanied by major bleeding or a clinically relevant non-major bleeding event, or a platelet count of < 25 × 109/L independent of such bleeding events [31].
Statistical Analysis
The primary population for efficacy analyses will be the full analysis set, defined as all randomly assigned patients who receive ≥ 1 dose of AKCEA-TTR-LRx and who have one baseline and at least one post-baseline efficacy assessment for mNIS + 7 score or Norfolk QOL-DN questionnaire total score.
Power calculations for this study are based on the assumption that TTR reduction will be 80%. Approximately 140 patients (120 administered AKCEA-TTR-LRx) will be enrolled in NEURO-TTRansform to account for a 10% dropout rate. In the NEURO-TTR trial, there were 52 evaluable completers in the placebo arm [26]. A sample size of 108 evaluable patients in the AKCEA-TTR-LRx arm will provide ≥ 95% power to detect a 70.3% difference in the percentage change from baseline in serum TTR, ≥ 90% power to detect a 19.6-point difference in the change from baseline of mNIS + 7, and ≥ 80% power to detect a 10.7-point difference in the change from baseline of the Norfolk QOL-DN score between AKCEA-TTR-LRx–treated patients and the historical NEURO-TTR placebo arm (two-sided alpha level, 0.025).
A sequential multiple testing procedure will be used to control the overall type 1 error rate at 0.05. If both co-primary endpoints of the interim analysis (TTR and mNIS + 7) are significant at an alpha level of 0.025, then the secondary endpoint (Norfolk QOL-DN score) will be tested at the interim analysis at an alpha level of 0.025. Regardless of the interim analysis results, the study will proceed as planned and the data will be collected from week 66 onwards at all study endpoints. For endpoints that are statistically significant at the week 35 interim analysis, the corresponding tests at the week 66 final analysis will not be conducted. The nonsignificant endpoint(s) (TTR and/or mNIS + 7) and the co-primary endpoint Norfolk QOL-DN score will be tested at the final analysis. If all the co-primary endpoints are significant, the secondary endpoints will be tested with the multiplicity controlled by the ranking strategy. Testing of the statistical significance of subsequent endpoints is contingent upon the attainment of statistical significance by the previous endpoint analyzed.
The percentage change in TTR will be assessed with a mixed-effects model for repeated measures (MMRM) adjusted by propensity score weights. The MMRM assumes that missing data are at random and that patients who discontinue prematurely would have behaved similarly to other patients in the same treatment group. The MMRM will include the effects of treatment, time, disease stage, pV50M mutation, previous treatment, treatment-by-time interaction, baseline value of the endpoint, and baseline-by-time interaction. The propensity score will be calculated for each patient in the AKCEA-TTR-LRx or historical placebo arm using a logistic regression model with baseline value of the endpoint and covariates including disease stage, pV50M mutation, and previous treatment. For mNIS + 7 and Norfolk QOL-DN score, the treatment comparison at week 35 will be based on the analysis of covariance model adjusted by propensity score. In the week 66 final analysis, the aforementioned MMRM adjusted by propensity score weights will be used for the treatment comparison for the percentage change from baseline in serum TTR, change from baseline in mNIS + 7, and Norfolk QOL-DN score.
Discussion
hATTR-PN is a rare, progressive, and fatal disease caused by mutations in the TTR gene that result in the synthesis of a destabilized TTR protein structure and lead to the formation of amyloid deposits in multiple organ systems [2, 7]. Although two TTR gene silencing treatments for hATTR-PN are available that reduce TTR and slow or halt the progression of the disease, there is an unmet need for an effective treatment with a more favorable risk–benefit profile and greater convenience of use. Inotersen requires weekly SC administration and regular monitoring for thrombocytopenia and glomerulonephritis, while patisiran requires intravenous infusion every 3 weeks and premedication with a corticosteroid to prevent infusion-related reactions [26]. The ligand-conjugated antisense technology is a significant advancement in the selective delivery to hepatocytes, yielding an approximate 20–30-fold increase in potency that permits substantial reduction in systemic exposure and an improved safety and tolerability profile [27, 32,33,34]. Similar to other ASO conjugates in this class, preclinical and phase 1 data on AKCEA-TTR-LRx demonstrated an increase in pharmacological potency compared with inotersen, a currently approved antisense medicine for the treatment of hATTR-PN. On the basis of the pathogenesis of ATTR, it is likely that preventing TTR from being synthesized would eliminate the origin of misfolded protein and subsequent amyloid fibril deposition, thus leading to the improvement of symptoms of ATTR, including polyneuropathy and cardiomyopathy.
NEURO-TTRansform is a phase 3 multicenter, open-label study of patients with stage 1 or stage 2 hATTR-PN randomly assigned to the AKCEA-TTR-LRx arm or an inotersen reference arm. Efficacy and safety data from participants enrolled in the AKCEA-TTR-LRx treatment arm will be compared with results from the historical placebo group in the NEURO-TTR trial [26]. The open-label design was selected because of the availability of approved treatments for hATTR-PN in some countries, rendering inclusion of a placebo control arm unethical [1, 17, 22,23,24,25]. This was not the case while the NEURO-TTR study was conducted, when the only standard of care was liver transplantation and tafamidis (which was only available at the time for stage 1 ATTR-PN in some European countries [26]). Patient eligibility criteria and the distribution of stage 1 and 2 hATTR-PN in the NEURO-TTRansform study are similar to those in the NEURO-TTR study, with identical endpoints and assessment times [26]. This provides an opportunity to adequately compare outcomes between patients who received AKCEA-TTR-LRx in NEURO-TTRansform and those who received placebo in NEURO-TTR. The lack of blinding in NEURO-TTRansform means that many sources of conscious and unconscious bias could be introduced. However, these limitations can be assessed to an extent by comparing the performance of inotersen up until week 35 in NEURO-TTRansform and the NEURO-TTR study, as inotersen represents a common denominator between the two studies.
One of the primary endpoints assessed in this study, change from baseline in mNIS + 7, was also assessed as a primary endpoint in the NEURO-TTR study [26]. The mNIS + 7 scoring procedure utilizes highly standardized, quantitative, and referenced assessments that are specifically designed to assess hATTR-PN impairment [35]. Assessments include the NIS, sensory and motor nerve conduction testing, quantitative sensory testing, and measurement of heart rate variation with deep breathing. The nerve conduction test is an objective and quantitative assessment, thereby providing a highly validated measure of neuropathy [35]. In the NEURO-TTR study, the mNIS + 7 scoring approach showed highly significant improvement in global scores and essentially all sub-scores with inotersen treatment, including quantitative measures and potentially objective measures in scored neuropathy signs [26, 35]. The favorable outcome is a result of utilizing previously validated scores, using the same specially trained mNIS + 7 evaluator throughout the study for each individual participant, and surveillance by a central expert reading center [35].
The AKCEA-TTR-LRx dosage regimen under investigation in phase 3 was selected on the basis of the pharmacodynamics and safety analyses of the phase 1 randomized placebo-controlled study in 47 healthy volunteers. AKCEA-TTR-LRx dosed at 45 mg every 4 weeks produced a mean reduction from baseline in serum TTR of 86% after four doses and an absence of potential tolerability or safety issues, such as the increases in liver transaminase levels observed in the upper dose range of this study [29]. The GalNAc-mediated delivery of AKCEA-TTR-LRx to hepatocytes supports low-dose therapy and a more convenient dosage regimen (i.e., monthly administration) relative to the unconjugated ASO therapy used for the treatment of hATTR-PN [22,23,24,25]. Since no placebo group will be utilized in this trial, enrolled participants will receive either an approved drug, inotersen, or AKCEA-TTR-LRx at a much lower dose to achieve a similar pharmacological effect. Eligible participants will have the option to enroll into a long-term extension trial after the completion of this study. As a targeted therapy, AKCEA-TTR-LRx has the potential to reduce the disease burden of hATTR-PN with lower and less frequent dose than the parent compound. The NEURO-TTRansform trial will determine whether a more effective and efficient reduction of TTR by AKCEA-TTR-LRx yields both an improved safety and tolerability profile and clinical benefit in terms of disease stability or regression.
Change history
15 March 2021
The article has been revised to include the corresponding author details and to include the affiliation of co-author, S. Tsimikas.
References
Ando Y, Coelho T, Berk JL, et al. Guideline of transthyretin-related hereditary amyloidosis for clinicians. Orphanet J Rare Dis. 2013;8:31.
Planté-Bordeneuve V, Said G. Familial amyloid polyneuropathy. Lancet Neurol. 2011;10:1086–97.
Gonzalez-Duarte A, Valdés-Ferrer SI, Cantú-Brito C. Characteristics and natural history of autonomic involvement in hereditary ATTR amyloidosis: a systematic review. Clin Auton Res. 2019;29(Suppl 1):1–9.
Yarlas A, Gertz MA, Dasgupta NR, et al. Burden of hereditary transthyretin amyloidosis on quality of life. Muscle Nerve. 2019;60:169–75.
Quintas A, Vaz DC, Cardoso I, Saraiva MJ, Brito RM. Tetramer dissociation and monomer partial unfolding precedes protofibril formation in amyloidogenic transthyretin variants. J Biol Chem. 2001;276:27207–13.
Hammarström P, Jiang X, Hurshman AR, Powers ET, Kelly JW. Sequence-dependent denaturation energetics: a major determinant in amyloid disease diversity. Proc Natl Acad Sci USA. 2002;99(Suppl 4):16427–32.
Johnson SM, Connelly S, Fearns C, Powers ET, Kelly JW. The transthyretin amyloidoses: from delineating the molecular mechanism of aggregation linked to pathology to a regulatory-agency-approved drug. J Mol Biol. 2012;421:185–203.
Foss TR, Wiseman RL, Kelly JW. The pathway by which the tetrameric protein transthyretin dissociates. Biochemistry. 2005;44:15525–33.
Mariani LL, Lozeron P, Théaudin M, et al. Genotype-phenotype correlation and course of transthyretin familial amyloid polyneuropathies in France. Ann Neurol. 2015;78:901–16.
Santos D, Coelho T, Alves-Ferreira M, et al. Large normal alleles of ATXN2 decrease age at onset in transthyretin familial amyloid polyneuropathy Val30Met patients. Ann Neurol. 2019;85:251–8.
Waddington-Cruz M, Schmidt H, Botteman MF, et al. Epidemiological and clinical characteristics of symptomatic hereditary transthyretin amyloid polyneuropathy: a global case series. Orphanet J Rare Dis. 2019;14:34.
Adams D, Cauquil C, Labeyrie C. Familial amyloid polyneuropathy. Curr Opin Neurol. 2017;30:481–9.
Lemos C, Coelho T, Alves-Ferreira M, et al. Overcoming artefact: anticipation in 284 Portuguese kindreds with familial amyloid polyneuropathy (FAP) ATTRV30M. J Neurol Neurosurg Psychiatry. 2014;85:326–30.
Schmidt HH, Waddington-Cruz M, Botteman MF, et al. Estimating the global prevalence of transthyretin familial amyloid polyneuropathy. Muscle Nerve. 2018;57:829–37.
Adams D, Ando Y, Beirão JM, et al. Expert consensus recommendations to improve diagnosis of ATTR amyloidosis with polyneuropathy. J Neurol. 2020. https://doi.org/10.1007/s00415-019-09688-0.
Coelho T, Inês M, Conceição I, Soares M, de Carvalho M, Costa J. Natural history and survival in stage 1 Val30Met transthyretin familial amyloid polyneuropathy. Neurology. 2018;91:e1999–2009.
European Medicines Agency. Vyndaqel (tafamidis) 20 mg soft capsules. Summary of product characteristics. 2020. https://www.ema.europa.eu/en/documents/product-information/vyndaqel-epar-product-information_en.pdf. Accessed 30 Mar 2020.
Pharmaceuticals and Medical Devices Agency. Vyndaqel (tafamidis) capsules 20 mg. Review report. 2019. https://www.pmda.go.jp/files/000231029.pdf. Accessed 8 Jun 2020.
Coelho T, Maia LF, Martins da Silva A, et al. Tafamidis for transthyretin familial amyloid polyneuropathy: a randomized, controlled trial. Neurology. 2012;79:785–92.
Berk JL, Suhr OB, Obici L, et al. Repurposing diflunisal for familial amyloid polyneuropathy: a randomized clinical trial. JAMA. 2013;310:2658–67.
Mathew V, Wang AK. Inotersen: new promise for the treatment of hereditary transthyretin amyloidosis. Drug Des Devel Ther. 2019;13:1515–25.
European Medicines Agency. Onpattro (patisiran) 2 mg/mL concentrate for solution for infusion. Summary of product characteristics. 2019. https://www.ema.europa.eu/en/documents/product-information/onpattro-epar-product-information_en.pdf. Accessed 30 Mar 2020.
Alnylam Pharmaceuticals Inc. Onpattro (patisiran) lipid complex injection for intravenous use. Full prescribing information. 2018. https://www.alnylam.com/wp-content/uploads/pdfs/ONPATTRO-Prescribing-Information.pdf. Accessed 30 Mar 2020.
European Medicines Agency. Tegsedi (inotersen) 284 mg solution for injection in pre-filled syringe. Summary of product characteristics. 2020. https://www.ema.europa.eu/en/documents/product-information/tegsedi-epar-product-information_en.pdf. Accessed 30 Mar 2020.
Akcea Therapeutics Inc. Tegsedi (inotersen) injection for subcutaneous use. Full prescribing information. 2018. https://tegsedihcp.com/wp-content/uploads/2018/10/prescribing-information.pdf. Accessed 30 Mar 2020.
Benson MD, Waddington-Cruz M, Berk JL, et al. Inotersen treatment for patients with hereditary transthyretin amyloidosis. N Engl J Med. 2018;379:22–31.
Crooke ST, Baker BF, Xia S, et al. Integrated assessment of the clinical performance of GalNAc3-conjugated 2’-O-methoxyethyl chimeric antisense oligonucleotides: I. Human volunteer experience. Nucleic Acid Ther. 2019;29:16–32.
Prakash TP, Graham MJ, Yu J, et al. Targeted delivery of antisense oligonucleotides to hepatocytes using triantennary N-acetyl galactosamine improves potency 10-fold in mice. Nucleic Acids Res. 2014;42:8796–807.
Viney NJ, Guo S, Tai L-J, et al. Ligand conjugated antisense oligonucleotide for the treatment of transthyretin amyloidosis: preclinical and phase 1 data. ESC Heart Fail. 2020;8(1):652–61.
Ackermann EJ, Guo S, Benson MD, et al. Suppressing transthyretin production in mice, monkeys and humans using 2nd-Generation antisense oligonucleotides. Amyloid. 2016;23:148–57.
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3:692–4.
Cohn DM, Viney NJ, Fijen LM, et al. Antisense inhibition of prekallikrein to control hereditary angioedema. N Engl J Med. 2020;383:1242–7.
Tsimikas S, Karwatowska-Prokopczuk E, Gouni-Berthold I, et al. Lipoprotein(a) reduction in persons with cardiovascular disease. N Engl J Med. 2020;382:244–55.
Viney NJ, van Capelleveen JC, Geary RS, et al. Antisense oligonucleotides targeting apolipoprotein(a) in people with raised lipoprotein(a): two randomised, double-blind, placebo-controlled, dose-ranging trials. Lancet. 2016;388:2239–53.
Dyck PJB, González-Duarte A, Obici L, et al. Development of measures of polyneuropathy impairment in hATTR amyloidosis: from NIS to mNIS + 7. J Neurol Sci. 2019;405:116424.
US Food and Drug Administration. Dolobid (diflunisal). Prescribing information. 2007. https://www.accessdata.fda.gov/drugsatfda_docs/label/2007/018445s058lbl.pdf. Accessed 8 Jun 2020.
Acknowledgements
Funding
This study and Rapid Service Publication Fee is supported by Ionis Pharmaceuticals, Inc. (Carlsbad, CA, USA) and Akcea Therapeutics (Boston, MA, USA).
Medical Writing, Editorial, and Other Assistance
Medical writing support was provided by Nancy Niguidula and Malcom Darkes of Excel Scientific Solutions (Fairfield, CT, USA) and funded by Ionis Pharmaceuticals. Critical review was provided by Sanjay Bhanot, MD, PhD, Brenda F. Baker, PhD, and Lisa Hannan, PhD, of Ionis Pharmaceuticals.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Teresa Coelho has received honoraria to attend scientific meetings from Akcea, Alnylam, Biogen, Ionis, and Pfizer and participates as a consultant in meetings promoted by Akcea, Alnylam, Biogen, Ionis, and Pfizer without financial compensation. Yukio Ando has received research funding from the Japan Society for the Promotion of Science Grants-in-Aid for Scientific Research (KAKENHI grant numbers 19H03565 and 16H0567). Merrill D. Benson has received grant support from the Veterans Administration Merit Review Program. John L. Berk participates as a consultant for Akcea, Alnylam, Corino, Intellia, and Ionis. Márcia Waddington-Cruz has received honoraria for consultancy and travel, and has been a principal investigator in clinical trials for Alnylam, FoldRx, Genzyme, Ionis, NHI, Pfizer, Prothena, and PTC. Peter J. Dyck has received honoraria for teaching and quality assurance of therapeutic trials in transthyretin amyloidosis from Alnylam and Ionis. Julian D. Gillmore has received honoraria for serving on scientific advisory boards from Alnylam, Eidos, Ionis/Akcea, and Pfizer. Sami L. Khella has received honoraria for consultancy from Akcea, Alnylam, Eidos, Ionis, and Pfizer. William J. Litchy had institutional contracts to train investigators and for quality control of data from Alnylam and Ionis. Laura Obici has received honoraria for speaking and consultancy from Akcea, Alnylam, and Pfizer. Nicholas J. Viney, Gustavo Buchele, Michela Brambatti, Shiangtung W. Jung, Sotirios Tsimikas, Eugene Schneider, Richard S. Geary, and Brett P. Monia are employees of and hold stock/stock options in Ionis. Cecilia Monteiro and Li-Jung Tai were employees of Ionis at the time the analysis was conducted and holds stock/stock options at Ionis. Louis St. L. O’Dea is an employee of and holds stock/stock options in Akcea. Morie Gertz has received honoraria from Alnylam, Amgen, Annexon, Apellis, Ionis/Akcea, Janssen, Medscape, Physicians Education Resource, and Prothena; workforce training from Sanofi; grants and personal fees from Spectrum; honoraria for speaking from DAVA Oncology, Johnson & Johnson, Medscape, and Teva; honoraria for serving on scientific advisory boards from Pharmacyclics and Proclara; honoraria for the development of educational materials from i3 Health; royalties from Springer; grant funding from the Amyloidosis Foundation, International Waldenstrom’s Macroglobulinemia Foundation, and The National Cancer Institute Specialized Programs for Research Excellence MM SPORE 5P50 CA186781-04; has served on the data safety monitoring boards for AbbVie, Celgene, and Research to Practice; and holds stock options from Aurora Bio.
Compliance with Ethics Guidelines
The study protocol and amendments have been approved by the relevant local IRBs or ECs for currently activated clinical study sites. Activation of additional clinical study sites is ongoing, and the study protocol and amendments will be approved by the relevant local IRBs/ECs before participants are allowed to enroll in the study. The full list of IRB/EC names and approval numbers is available upon request. The study is being conducted according to the International Conference on Harmonisation guidelines and relevant country-specific laws. All participants must provide written informed consent prior to study inclusion. A data and safety monitoring board will periodically review safety, tolerability, and efficacy data relating to AKCEA-TTR-LRx and inotersen, including the results of the predetermined interim analysis at week 35.
Data Availability
The study is registered at ClinicalTrials.gov (NCT04136184) and EudraCT (2019-001698-10).
Author information
Authors and Affiliations
Corresponding author
Additional information
C. Monteiro and L.-J. Tai were employees of Ionis Pharmaceuticals Inc. at the time of this work. L. St. L. O'Dea was an employee of Akcea Therapeutics at the time of this work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Coelho, T., Ando, Y., Benson, M.D. et al. Design and Rationale of the Global Phase 3 NEURO-TTRansform Study of Antisense Oligonucleotide AKCEA-TTR-LRx (ION-682884-CS3) in Hereditary Transthyretin-Mediated Amyloid Polyneuropathy. Neurol Ther 10, 375–389 (2021). https://doi.org/10.1007/s40120-021-00235-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-021-00235-6