Abstract
Purpose of Review
Previous literature reviews summarized the associations between individual foods or food groups and lung cancer risk, but the relationship between dietary patterns and lung cancer risk has received less attention. We conducted a systematic review and meta-analyses of observational studies on the associations between dietary patterns and lung cancer risk.
Recent Findings
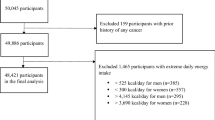
PubMed, Embase, and Web of Science were systematically searched from inception to February 2023. Random-effects models were used to pool relative risks (RR) on associations with at least two studies. Twelve studies reported on data-driven dietary patterns, and 17 studies reported on a priori dietary patterns. A prudent dietary pattern (high in vegetables, fruit, fish, and white meat) tended to be associated with a lower risk of lung cancer (RR = 0.81, 95% confidence interval [CI] = 0.66–1.01, n = 5). In contrast, Western dietary patterns, characterized by higher intakes of refined grains and red and processed meat, were significantly positively associated with lung cancer (RR = 1.32, 95% CI = 1.08–1.60, n = 6). Healthy dietary scores were consistently associated with a lower risk of lung cancer (Healthy Eating Index [HEI]: RR = 0.87, 95% CI = 0.80–0.95, n = 4; Alternate HEI: RR = 0.88, 95% CI = 0.81–0.95, n = 4; Dietary Approaches to Stop Hypertension: RR = 0.87, 95% CI = 0.77–0.98, n = 4; Mediterranean diet: RR = 0.87, 95% CI = 0.81–0.93, n = 10) while the dietary inflammatory index was associated with a higher risk of lung cancer (RR = 1.14, 95% CI = 1.07–1.22, n = 6).
Summary
Our systematic review indicates dietary patterns characterized by a higher intake of vegetables and fruits, a lower intake of animal products, and anti-inflammation may be associated with a reduced risk of lung cancer.




Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- AHEI:
-
Alternate Healthy Eating Index
- CI:
-
Confidence intervals
- DASH:
-
Dietary Approaches to Stop Hypertension
- DII:
-
Dietary Inflammatory Index
- EDIP:
-
Empirical Dietary Inflammation Pattern
- HEI:
-
Healthy Eating Index
- NOS:
-
Newcastle-Ottawa scale
- RR:
-
Relative risk
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Howlader N NA, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z,. SEER cancer statistics review, 1975–2018. site. Available at https://seer.cancer.gov/csr/1975_2018/.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30. https://doi.org/10.3322/caac.21590.
U.S. Department of Health and Human Services. The health consequences of smoking: a report of the surgeon general. In.; 2004.
Parkin DM, Bray F, Ferlay J, et al. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55(2):74–108. https://doi.org/10.3322/canjclin.55.2.74.
World Cancer Research Fund International. Diet, nutrition, physical activity and cancer: a global perspective: a summary of the Third Expert Report. In.: World Cancer Research Fund International; 2018.
•• Steck SE, Murphy EA. Dietary patterns and cancer risk. Nat Rev Cancer. 2020;20(2):125–38. https://doi.org/10.1038/s41568-019-0227-4. The review summarized the evidence on associations between dietary patterns and cancer risk and pointed out directions for future research.
Krebs-Smith SM, Subar AF, Reedy J. Examining dietary patterns in relation to chronic disease: matching measures and methods to questions of interest. Circulation. 2015;132(9):790–3. https://doi.org/10.1161/CIRCULATIONAHA.115.018010.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13(1):3–9. https://doi.org/10.1097/00041433-200202000-00002.
Guenther PM, Casavale KO, Reedy J, et al. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013;113(4):569–80. https://doi.org/10.1016/j.jand.2012.12.016.
Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10. https://doi.org/10.1056/NEJM200101043440101
Trichopoulou A, Costacou T, Bamia C, et al. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–608. https://doi.org/10.1056/NEJMoa025039.
Shivappa N, Steck SE, Hurley TG, et al. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17(8):1689–96. https://doi.org/10.1017/S1368980013002115.
Tabung FK, Smith-Warner SA, Chavarro JE, et al. Development and validation of an empirical dietary inflammatory index. J Nutr. 2016;146(8):1560–70. https://doi.org/10.3945/jn.115.228718.
Sun Y, Li Z, Li J, et al. A healthy dietary pattern reduces lung cancer risk: a systematic review and meta-analysis. Nutrients. 2016;8(3):134. https://doi.org/10.3390/nu8030134.
• Bahrami A, Khalesi S, Makiabadi E, et al. Adherence to the Mediterranean diet and the risk of lung cancer: a systematic review and dose-response meta-analysis of observational studies. Nutr Rev. 2022;80(5):1118–28. https://doi.org/10.1093/nutrit/nuab117. The study reviewed the evidence on Mediterranean diet and risk of lung cancer, and results were consistent with our main findings.
Schulpen M, van den Brandt PA. Adherence to the Mediterranean diet and risk of lung cancer in the Netherlands Cohort Study. Br J Nutr. 2018;119(6):674–84. https://doi.org/10.1017/S0007114517003737.
Boden S, Myte R, Wennberg M, et al. The inflammatory potential of diet in determining cancer risk; a prospective investigation of two dietary pattern scores. PLoS One. 2019;14(4):e0214551. https://doi.org/10.1371/journal.pone.0214551
Shivappa N, Wang R, Hebert JR, et al. Association between inflammatory potential of diet and risk of lung cancer among smokers in a prospective study in Singapore. Eur J Nutr. 2019;58(7):2755–66. https://doi.org/10.1007/s00394-018-1825-8.
• Wang Q, Hashemian M, Sepanlou SG, et al. Dietary quality using four dietary indices and lung cancer risk: the Golestan Cohort Study (GCS). Cancer Causes Control. 2021;32(5):493–503. https://doi.org/10.1007/s10552-021-01400-w. This is the latest study examaining the association between different dietary quality indices and lung cancer risk using a prospective cohort design.
Park SY, Boushey CJ, Shvetsov YB, et al. Diet quality and risk of lung cancer in the multiethnic cohort study. Nutrients. 2021;13(5):1614. https://doi.org/10.3390/nu13051614.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. https://doi.org/10.1016/j.ijsu.2010.02.007.
Wells GA, Shea B, O’Connell Da, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. In.: Oxford; 2000.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88. https://doi.org/10.1016/0197-2456(86)90046-2.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. https://doi.org/10.1002/sim.1186.
Gnagnarella P, Maisonneuve P, Bellomi M, et al. Red meat, Mediterranean diet and lung cancer risk among heavy smokers in the COSMOS screening study. Ann Oncol. 2013;24(10):2606–11. https://doi.org/10.1093/annonc/mdt302.
Tsai YY, McGlynn KA, Hu Y, et al. Genetic susceptibility and dietary patterns in lung cancer. Lung Cancer. 2003;41(3):269–81. https://doi.org/10.1016/s0169-5002(03)00238-1.
Balder HF, Goldbohm RA, van den Brandt PA. Dietary patterns associated with male lung cancer risk in the Netherlands Cohort Study. Cancer Epidemiol Biomarkers Prev. 2005;14(2):483–90. https://doi.org/10.1158/1055-9965.EPI-04-0353.
Mai V, Kant AK, Flood A, et al. Diet quality and subsequent cancer incidence and mortality in a prospective cohort of women. Int J Epidemiol. 2005;34(1):54–60. https://doi.org/10.1093/ije/dyh388.
De Stefani E, Boffetta P, Ronco AL, et al. Nutrient patterns and risk of lung cancer: a factor analysis in Uruguayan men. Lung Cancer. 2008;61(3):283–91. https://doi.org/10.1016/j.lungcan.2008.01.004.
De Stefani E, Deneo-Pellegrini H, Boffetta P, et al. Dietary patterns and risk of cancer: a factor analysis in Uruguay. Int J Cancer. 2009;124(6):1391–7. https://doi.org/10.1002/ijc.24035.
De Stefani E, Ronco AL, Deneo-Pellegrini H, et al. Dietary patterns and risk of adenocarcinoma of the lung in males: a factor analysis in Uruguay. Nutr Cancer. 2011;63(5):699–706. https://doi.org/10.1080/01635581.2011.563033.
Gorlova OY, Weng SF, Hernandez L, et al. Dietary patterns affect lung cancer risk in never smokers. Nutr Cancer. 2011;63(6):842–9. https://doi.org/10.1080/01635581.2011.589958.
Gnagnarella P, Maisonneuve P, Bellomi M, et al. Nutrient intake and nutrient patterns and risk of lung cancer among heavy smokers: results from the COSMOS screening study with annual low-dose CT. Eur J Epidemiol. 2013;28(6):503–11. https://doi.org/10.1007/s10654-013-9803-1.
Anic GM, Park Y, Subar AF, et al. Index-based dietary patterns and risk of lung cancer in the NIH-AARP diet and health study. Eur J Clin Nutr. 2016;70(1):123–9. https://doi.org/10.1038/ejcn.2015.122.
Hodge AM, Bassett JK, Shivappa N, et al. Dietary inflammatory index, Mediterranean diet score, and lung cancer: a prospective study. Cancer Causes Control. 2016;27(7):907–17. https://doi.org/10.1007/s10552-016-0770-1.
Maisonneuve P, Shivappa N, Hebert JR, et al. Dietary inflammatory index and risk of lung cancer and other respiratory conditions among heavy smokers in the COSMOS screening study. Eur J Nutr. 2016;55(3):1069–79. https://doi.org/10.1007/s00394-015-0920-3.
Tu H, Heymach JV, Wen CP, et al. Different dietary patterns and reduction of lung cancer risk: a large case-control study in the U.S. Sci Rep. 2016;6:26760. https://doi.org/10.1038/srep26760
He F, Xiao RD, Lin T, et al. Dietary patterns, BCMO1 polymorphisms, and primary lung cancer risk in a Han Chinese population: a case-control study in Southeast China. BMC Cancer. 2018;18(1):445. https://doi.org/10.1186/s12885-018-4361-2.
Kane-Diallo A, Srour B, Sellem L, et al. Association between a pro plant-based dietary score and cancer risk in the prospective NutriNet-sante cohort. Int J Cancer. 2018;143(9):2168–76. https://doi.org/10.1002/ijc.31593.
Hawrysz I, Wadolowska L, Slowinska MA, et al. Adherence to prudent and mediterranean dietary patterns is inversely associated with lung cancer in moderate but not heavy male polish smokers: a case-control study. Nutrients. 2020;12(12). https://doi.org/10.3390/nu12123788
Cai H, Sobue T, Kitamura T, et al. Low-carbohydrate diet and risk of cancer incidence: the Japan Public Health Center-based prospective study. Cancer Sci. 2022;113(2):744–55. https://doi.org/10.1111/cas.15215.
Zhang Y, Zhong G, Zhu M, et al. Association between diabetes risk reduction diet and lung cancer risk in 98,159 participants: results from a prospective study. Front Oncol. 2022;12:855101. https://doi.org/10.3389/fonc.2022.855101
Deschasaux M, Huybrechts I, Murphy N, et al. Nutritional quality of food as represented by the FSAm-NPS nutrient profiling system underlying the Nutri-Score label and cancer risk in Europe: Results from the EPIC prospective cohort study. PLoS Med. 2018;15(9):e1002651. https://doi.org/10.1371/journal.pmed.1002651
Myneni AA, Giovino GA, Millen AE, et al. Indices of diet quality and risk of lung cancer in the women’s health initiative observational study. J Nutr. 2021;151(6):1618–27. https://doi.org/10.1093/jn/nxab033.
Sadeghi A, Parastouei K, Seifi S, et al. Inflammatory potential of diet and odds of lung cancer: a case-control study. Nutr Cancer. 2022;74(8):2859–67. https://doi.org/10.1080/01635581.2022.2036770.
Wei X, Zhu C, Ji M, et al. Diet and risk of incident lung cancer: a large prospective cohort study in UK biobank. Am J Clin Nutr. 2021;114(6):2043–51. https://doi.org/10.1093/ajcn/nqab298.
Willemsen RF, McNeil J, Heer E, et al. Dietary patterns with combined and site-specific cancer incidence in Alberta’s Tomorrow Project cohort. Eur J Clin Nutr. 2022;76(3):360–72. https://doi.org/10.1038/s41430-021-00958-7.
Vieira AR, Abar L, Vingeliene S, et al. Fruits, vegetables and lung cancer risk: a systematic review and meta-analysis. Ann Oncol. 2016;27(1):81–96. https://doi.org/10.1093/annonc/mdv381.
Angelino D, Godos J, Ghelfi F, et al. Fruit and vegetable consumption and health outcomes: an umbrella review of observational studies. Int J Food Sci Nutr. 2019;70(6):652–67. https://doi.org/10.1080/09637486.2019.1571021.
Huang Y, Cao D, Chen Z, et al. Red and processed meat consumption and cancer outcomes: umbrella review. Food Chem. 2021;356:129697. https://doi.org/10.1016/j.foodchem.2021.129697
Miller V, Webb P, Micha R, et al. Defining diet quality: a synthesis of dietary quality metrics and their validity for the double burden of malnutrition. Lancet Planet Health. 2020;4(8):e352–70. https://doi.org/10.1016/s2542-5196(20)30162-5.
Greten FR, Grivennikov SI. Inflammation and cancer: triggers, mechanisms, and consequences. Immunity. 2019;51(1):27–41. https://doi.org/10.1016/j.immuni.2019.06.025.
Marx W, Veronese N, Kelly JT, et al. The dietary inflammatory index and human health: an umbrella review of meta-analyses of observational studies. Adv Nutr. 2021;12(5):1681–90. https://doi.org/10.1093/advances/nmab037.
Fowler ME, Akinyemiju TF. Meta-analysis of the association between dietary inflammatory index (DII) and cancer outcomes. Int J Cancer. 2017;141(11):2215–27. https://doi.org/10.1002/ijc.30922.
Subramaniam S, Selvaduray KR, Radhakrishnan AK. Bioactive compounds: natural defense against cancer? Biomolecules. 2019;9(12):758. https://doi.org/10.3390/biom9120758.
Yang JJ, Yu D, Xiang YB, et al. Association of dietary fiber and yogurt consumption with lung cancer risk: a pooled analysis. JAMA Oncol. 2020;6(2):e194107. https://doi.org/10.1001/jamaoncol.2019.4107
Gomes M, Teixeira AL, Coelho A, et al. The role of inflammation in lung cancer. Adv Exp Med Biol. 2014;816:1–23. https://doi.org/10.1007/978-3-0348-0837-8_1.
Abid Z, Cross AJ, Sinha R. Meat, dairy, and cancer. Am J Clin Nutr. 2014;100(Suppl 1):386S-393S. https://doi.org/10.3945/ajcn.113.071597.
Ward HA, Whitman J, Muller DC, et al. Haem iron intake and risk of lung cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Eur J Clin Nutr. 2019;73(8):1122–32. https://doi.org/10.1038/s41430-018-0271-2.
Heydari G, Heidari F, Yousefifard M, et al. Smoking and diet in healthy adults: a cross-sectional study in tehran, iran, 2010. Iran J Public Health. 2014;43(4):485–91.
Alkerwi A, Baydarlioglu B, Sauvageot N, et al. Smoking status is inversely associated with overall diet quality: Findings from the ORISCAV-LUX study. Clin Nutr. 2017;36(5):1275–82. https://doi.org/10.1016/j.clnu.2016.08.013.
MacLean RR, Cowan A, Vernarelli JA. More to gain: dietary energy density is related to smoking status in US adults. BMC Public Health. 2018;18(1):365. https://doi.org/10.1186/s12889-018-5248-5.
Polanski J, Chabowski M, Jankowska-Polanska B, et al. Histological subtype of lung cancer affects acceptance of illness, severity of pain, and quality of life. J Pain Res. 2018;11:727–33. https://doi.org/10.2147/JPR.S155121.
Acknowledgements
We acknowledge authors of the original studies that included in our systematic review and meta-analyses.
Author information
Authors and Affiliations
Contributions
Study conception and design: LZ and SS; study protocol: LZ and SS; literature research and data extraction: LZ and BK; data analyses: LZ and BK; results interpretation: LZ, BK, JZ, and SS; draft: LZ; review and critical revision: LZ, BK, JZ, and SS; read and approved the version of the manuscript being submitted: LZ, BK, JZ, and SS.
Corresponding author
Ethics declarations
Conflict of Interest
All authors have no conflict of interest to declare.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, L., Kase, B., Zheng, J. et al. Dietary Patterns and Risk of Lung Cancer: A Systematic Review and Meta-Analyses of Observational Studies. Curr Nutr Rep 12, 338–357 (2023). https://doi.org/10.1007/s13668-023-00469-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-023-00469-w