Abstract
Aims
Cachexia, the wasting disorder associated with a wide range of serious illnesses including cancer, is a major cause of morbidity and mortality. There is currently no widely approved therapeutic agent for treating or preventing cancer-associated cachexia. Colorectal cancer and non-small cell lung cancer have relatively high incidences of cachexia, approximately 28% and 34%, respectively. Neurohormonal overactivity has been implicated in the genesis and progression of cachexia and beta receptor antagonism has been proposed as a potential therapy. MT-102, a novel anabolic/catabolic transforming agent, has a multi-functional effect upon three potential pharmacological targets in cancer cachexia, namely reduced catabolism through non-selective β-blockade, reduced fatigue, and thermogenesis through central 5-HT1a antagonism and increased anabolism through partial β-2 receptor agonism.
Methods
At least 132 male and female patients, aged between 25 and 80 years with a confirmed diagnosis of late-stage non-small cell lung cancer or colorectal cancer, with cachexia will be randomised to either one of the two MT-102 doses or placebo in a 3:1:2 ratio (MT-102 10 mg BD−1/MT-102 2.5 mg BD/placebo). Patients will continue on study treatment for maximally 16 weeks. The primary endpoint, to be analysed by assigned treatment group, will be body weight change over 16 weeks. For this endpoint, the study has 85% power (0.05% significance level) to detect per 4-week period a mean change of −0.8 kg in the placebo group and 0 kg in the high-dose MT-102 arm. The first patient was randomised in February 2011 and patient recruitment is expected to continue until mid-2012.
Perspective
The ACT-ONE trial is designed to test whether the anabolic/catabolic transforming agent MT-102 will positively impact on the rate of change of body weight in cancer cachexia, thereby evaluating a novel therapeutic strategy in this hitherto poorly treatable condition. A separate ACT-TWO trial will recruit patients who complete the ACT-ONE trial and remain on randomised double-blind medication. Participants in ACT-TWO will be followed for an additional period with a separate primary endpoint.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cachexia, defined as weight loss, associated with a chronic underlying disease, of at least 5% in 12 months or less is associated with significant morbidity and mortality [1]. Cachexia is known to accompany a wide range of serious illnesses, including cancer, chronic heart failure, COPD and chronic renal failure [2]. It is associated with significant muscle wasting (myopenia [3]), loss of muscle strength, fatigue [4] and anorexia [5], in additional to neurohormonal and biochemical abnormalities [6]. Its pathophysiology is characterized by a negative protein and energy balance driven by a variable combination of reduced food intake and abnormal metabolism.
Cachexia occurs in about a third of all cancer patients and has been estimated to be the direct cause of death in 20% to 40% of all cancer-related deaths [2]. As for other solid tumours, colorectal cancer (CRC) and non-small cell lung cancer (NSCLC) have relatively high incidences of cachexia, approximately 28% and 34%, respectively, and cachexia is known to be associated with poor outcomes and increased mortality in these cancers. Presently no therapy is widely approved for the treatment of cancer-associated cachexia. It would be very attractive to use relatively inexpensive non-toxic, non-cytotoxic agents to treat cachexia in this patient group.
MT-102 is an anabolic/catabolic transforming agent with properties including non-specific beta-1 and beta-2 adrenergic receptor blocking activity and intrinsic sympathomimetic activity (ISA). In addition to its β-blocking and ISA activity, MT-102 is a highly potent antagonist of 5-HT1a receptors and binds to 5-HT 1a receptors in the brain. MT-102 augments and decreases the time to onset of selective serotonin reuptake inhibitor therapy via blockade of 5-HT1a receptors. Through its combined pharmacological actions, MT-102 has a multi-functional effect upon three potential pharmacological targets, each of which is relevant for cancer cachexia, as follows:
-
Reduced catabolism, through non-selective β-blockade,
-
Reduced fatigue and thermogenesis, through central 5-HT1a antagonism,
-
Increased anabolism, through partial β2-receptor agonism,
This triad of pharmacological effects renders MT-102 a unique and highly advantaged candidate for development in cancer cachexia.
In the Yoshida hepatoma rat model, of cancer cachexia, MT-102 demonstrates superior efficacy, relative to any other agent tested, including other β-blockers [7]. In this model, MT-102 administration leads to a dose-dependent increase in weight, lean body mass and functional activity. Furthermore, it has been shown to enhance the survival of animals in this model in a dose-dependent manner. This heightened efficacy is presumed to be due to the unique multi-functional pharmacological activity of this particular agent.
The ACT-ONE trial will assess the potential efficacy of two different doses of MT-102 in patients with cachexia due to two common forms of cancer. Data from this study, along with that of the ACT-TWO study, will allow the design and conduct of appropriate phase III clinical studies to confirm the utility of MT-102 for this indication. The ACT-ONE study is powered to establish an effect of the higher dose of MT-102 upon the rate of change of body weight; which is the cardinal factor in the definition of cachexia, whereas the ACT-TWO study will be powered for patients' clinical status. Both studies will also examine the effect of MT-102 upon a number of measures of performance and quality of life.
2 Methods
2.1 Study objectives
The primary objective of the ACT-ONE trial is to investigate, compared to placebo, the effect of a 10 mg/BD dose of MT-102 in comparison to placebo on the rate of change of body weight over a 16-week period in patients with cachexia related to underlying stages III and IV colorectal or non-small cell lung cancer. Secondary objectives will investigate, compared to placebo, the dose response effects of two different doses of MT-102 in comparison to placebo over a 16-week period on:
-
the slope of weight change
-
the short physical performance battery test(SPPB)
-
the six-minute walk test (SMWT)
-
hand grip strength (HGS)
-
measures of quality of life (QOL)
-
change of body composition according to dual energy X-ray absorbitometry (DEXA)
-
all cause mortality
-
the adverse event profile
-
inflammatory, neuroendocrine and catabolic/anabolic biomarkers
2.2 Overall design and planning
The ACT-ONE trial is a multicentre, international randomised, double-blind, placebo-controlled, dose-finding phase II clinical study which will investigate patients with cachexia related to non-small cell lung cancer or colorectal cancer. It is planned to recruit 132 male or female patients who will be treated with MT-102 or placebo for a period of 16 weeks. All patients will receive standard of care chemotherapy, radiotherapy and supportive care throughout the study at the discretion of their treating physician. The physicians will be instructed to plan the chemotherapy cycles and the functional assessment visits in such a manner that chemotherapy does not interfere with the performance of the functional assessments by the patients.
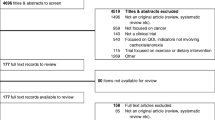
Potentially eligible patients will undergo screening assessments which will include a set of performance tests [stair climbing power (SCP), HGS, short physical performance battery test and the SMWT]. In addition, patients will be given a 7-day course of placebo tablets (one tablet twice daily). Patients able to complete the performance tests as required by the protocol selection criteria and who are at least 80% compliant with the placebo run-in phase will then be randomised to either MT-102 2.5 or 10 mg BD or placebo. All patients will be seen weekly for the first month after randomisation and thereafter every 4 weeks, up to a maximum of 16 weeks. The schedule of visits, examinations and investigations is summarised in the study schematic shown in Fig. 1. The dose of investigational product will be escalated by the investigator in a blinded fashion. The maximum period of drug titration is 4 weeks and the minimum is 2 weeks. Patients will be required to attend study visits at 1-week intervals after the start of the titration phase until completion of dose escalation.
The study will be conducted in accordance with the principles stated in the Declaration of Helsinki (1996), International Conference on Harmonisation Good Clinical Practice, and local and national regulations. Written informed consent will be obtained for all patients prior to any study-related procedures.
2.3 Patient selection
The complete patient selection criteria are shown in Table 1. Briefly, male and female patients aged between 25 and 80 years with a confirmed diagnosis of non-curative stage III or IV CRC or NSCLC, not suitable for surgery and with a life expectancy of at least 3 months will be potentially eligible to participate in the ACT-ONE study if, in addition, to the criteria listed in Table 1 they are suffering from cachexia with ongoing weight loss that in the opinion of the investigator is due to the underlying cancer.
2.4 Randomisation
It is planned that in total, 132 patients who comply with the protocol selection criteria will be randomised in a 3:1:2 ratio as follows: 66 patients will be randomised to receive high-dose MT-102 (i.e. 10 mg/BD), 22 patients will be randomised to receive low-dose MT-102 (i.e. 2.5 mg/BD), and 44 patients will be randomised to receive placebo.
The first patient was randomised in February 2011 and patient recruitment is expected to continue until mid 2012.
2.5 Treatment regimens
MT-102 or placebo will be administered over a 16-week period. The treatment regimens for the study are summarised in Table 2.
3 Assessments
3.1 Functional evaluations
The SMWT will be conducted as described by Paul L. Enright (Respiratory Care, August 2003 vol. 48 no. 8) [8]. The SCP test will be modified from that described by Bean et al. (Arch Phys Med Rehabil vol. 88, May 2007) [9] to account for the different stairway configurations at the investigational sites. Results will be analysed as a normalised power per kilogramme according to the methods of Bean et al. [9]. An SPPB test will be conducted as described by Guralnik et al. (Journal of Gerontology 1994, vol. 49, no. 2) [10]. A HGS test will be modified from that described by Bassey (1990; NIH, 1990) [11].
QoL will be assessed using the EQ-5D instrument on days at days 0, 28, 56, 84 and 112. The EQ-5D questionnaire will be administered by the investigator using the relevant validated instrument and using the patient's preferred language. The patient's answers will be recorded directly into the CRF by the investigator. The patient will be asked to complete the visual analogue scale section of the EQ-5D directly on the CRF. DEXA scans will be performed at selected DEXA scan centres on days at day −1, 56 and 112.
3.2 Biomarker studies
Samples from selected sites will be stored at −70° centigrade and then analysed after completion of the study. A panel of nutritional, inflammatory cardiovascular and neurohormonal biomarkers will be conducted on these retained samples. Depending upon the clinical outcomes observed in this study, the constituents of this panel will be selected from: total cholesterol, low-density lipoprotein, high-density lipoprotein, triglycerides, pre-albumin, cortisol, high-sensitivity C-reactive protein, interleukin-6, tumour necrosis factor (TNF), soluble TNF-receptors, pro-calcitonin, adrenaline, nor-adrenaline, aldosterone, cortisol, hehydroepiandrosterone, free testosterone, matrix metalloproteinase-2,matrix metalloproteinase-9, growth hormone, insulin-like growth factor-1, leptin, allantoin, B-type natriuretic peptide (BNP), N-terminal BNP, atrial natriuretic peptide (ANP), mid-region pro-ANP, co-peptin, pro-adrenomedulin and s-pindolol. The biomarker panel will be used to examine for potential correlates of safety and efficacy for future clinical examination and research.
3.3 Pharmaco-vigilance and safety assessments
As defined by the ICH Guideline for Good Clinical Practice (CPMP/ICH/135/95), adverse events, serious adverse events and serious unexpected suspected adverse reactions will be captured and reported for this study. The ACT-ONE Trial has appointed independent medical monitors (IMMs) with experience in the conduct and review of multicentre phase II or III oncology studies to review cumulative safety surveillance data on a regular basis throughout the study and make recommendations regarding further conduct of the study. The IMMs will also review safety data judged to be medically significant by the medical monitor. The IMMs will review blinded safety surveillance data reported to the sponsor, but may request to be unblinded if necessary to make safety assessments and study recommendations provided that no study or sponsor personnel shall be unblinded in this process. The IMMs will make recommendations to the sponsor to stop study entry and dosing if they deem it necessary.
3.4 Sample size and statistical considerations
The underlying hypothesis for this trial is that high dose (i.e. 20 mg) of MT-102, relative to placebo, favourably affects the primary endpoint. Sample size calculations were therefore based on:
-
the null-hypothesis (Ho) that there is no difference in the mean weight loss rate between high-dose MT-102 and placebo,
-
a two-sided significance test for the rejection of Ho with a level α of 0.05,
-
a power of 85%,
-
an expected mean weight change per 4-week period of −0.8 kg in the placebo group and a mean weight change per 4-week period of 0 kg in the high-dose MT-102 arm,
-
a standard deviation of 1.2 kg per 4-week period,
-
an allocation ratio of 3:2:1, i.e. MT-102 10 mg BD/MT-102 2.5 mg BD/placebo.
The size of the primary modified intention-to-treat (mITT) analysis population for this trial has been set to 102 patients randomised in a 3:1:2 ratio (active high-dose MT-102/active low-dose MT-102/placebo). To allow for 20% of recruited patients who do not comply with the criteria for inclusion in the mITT population, 132 patients in total will be started on study treatment (66 patients in the active high dose, 22 patients in the active low dose and 44 patients in the placebo arm). The sample size considerations for this study were based on the results of the Randomized Clinical Trial of Adenosine 5-Triphosphate in Patients With Advanced Non-Small-Cell Lung Cancer (Journal of the National Cancer Institute, Vol. 92, No. 4, February 16, 2000) [12]. In this randomised trial, the weight loss rate in patients allocated to adenosine 5-triphosphate was compared to patients allocated to placebo. Patients included in this trial had stage IIIb or IV NSCLC and were followed for 28 weeks with a weight assessment every 4 weeks. In the placebo group, the mean weight change per 4-week period was −1 kg (95% confidence interval [CI] = −1.5 to −0.5, n = 24). The corresponding standard deviation is 1.2 kg per 4-week period. In the same study, patients considered to be cachexic (i.e., weight loss >5% of weight before illness) had a mean weight loss rate of −1.6 kg per 4-week period.
Based on the above assumptions, a mean weight change per 4-week period of −0.8 kg in the placebo group versus no weight loss in the high-dose-treated group will be used for the MT-102 trial and a standard deviation of 1.2 kg per 4 weeks.
3.5 Statistical and analytical plan
Demographics and baseline characteristics will be documented by descriptive statistics on the ITT and modified ITT populations. The safety analysis will be performed by treatment received. The efficacy criteria will be displayed by treatment arm, by dose and time point for the following assessments:
-
body weight and body weight changes;
-
DEXA scan
-
stair climbing power;
-
six-minute walk test;
-
short physical performance battery test;
-
hand grip strength;
-
EQ-5D QoL data.
The safety analyses will be based on the safety analysis population. Descriptive statistics will include means, standard deviations, medians and ranges for continuous variables (including changes), and frequency distributions for discrete variables. Time-to-event data will be analysed by Kaplan–Meier plots and appropriate event rates using person-time “at risk” denominators will be given. Details of the analyses to be performed will be described in the statistical analysis plan.
4 Discussion
The ACT-ONE trial investigates a novel approach to the therapy of cancer-related cachexia. The primary endpoint of change in the rate of weight loss is clinically relevant, as weight loss is both a defining feature of cachexia and a major complaint of sufferers. Given the importance of loss of lean tissue to the symptoms of cachexia including fatigue and loss of functional capacity, it is highly plausible that a reduction in the rate of further weight loss may be associated with improvements in both symptoms and objective functional capacity, measures of which have therefore been incorporated as secondary efficacy assessment endpoints in this study.
There have been very few trials of drug therapies to reduce weight loss in cancer cachexia. The ACE inhibitor imidapril has been trialled in 200 patients with one of three cancer types and has been reported to have improved weight in two (Colorectal and non-small cell lung cancer) but neither in the third-type studied (pancreatic) nor in the pre-specified analysis of all three cancer types taken together (http://www.biotech-intelligence.com/html/html/2a462148882a297c8eafbeafbaeff7ff.html). Ostarine, an investigational selective androgen receptor modulator enhanced lean body mass and muscle performance in a phase II clinical trial in patients with cancer cachexia. Ostarine led to significant increase in the primary endpoint of lean body mass (LBM) change with an associated improvement in muscle performance measured by stair climb in patients with cancer cachexia. The change from baseline in LBM for the placebo, 1- and 3-mg treatment groups was 0.1, 1.5 (p = 0.001) and 1.3 kg (p = 0.045), respectively, at the end of the 16-week trial (http://www.pharmaceutical-business-review.com/news/gtxs_phaseii_cancer_cachexia_trial_meets_primary_endpoint_090611). Infliximab was studied in 89 patients with pancreatic cancer-related cachexia and did not show a statistically significant effect on lean body mass [13]. Etanercept (a dimeric fusion protein inhibitor of TNF) was tested in 63 evaluable patients with cancer-related weight loss and achieved no significant benefit in terms of weight gain or reduced weight loss [14].
In a phase II clinical study, the orally administered grehlin agonist anamorelin was shown to produce an improvement in total body mass and a trend towards increased lean mass over a 12-week period in patients with cancer, but without any improvement in quality of life [15]. Anamorelin is now being examined in phase III clinical trials for patients with cachexia due to non-small cell lung cancer.
Other ongoing phase II trials in cancer cachexia include interventions such as the immunomodulator OHR/AVR118 in 30 cancer cachexia patients (http://www.marketwire.com/press-release/ohr-pharmaceutical-enrolls-first-three-patients-new-clinical-site-ongoing-phase-2b-cachexia-1368449.htm), a pilot study of APD209 (an oral fixed-dose combination of a progestin and a selective β2-agonist) in cancer cachexia in 16 patients (http://clinicaltrials.gov/show/NCT00895726) and lenalidomide (an immunodulatory derivate of thalidomide) in 60 patients with cancer cachexia (http://clinicaltrials.gov/ct2/show/NCT01127386?term=cachexia&rank=1).
Cachexia, despite being very common in many solid tumour cancers, remains a poorly studied, under-diagnosed and largely untreated complication that causes severe symptomatic limitation and predisposes to in increased mortality. The ACT-ONE trial will help evaluate the potential role of an interesting approach to its management.
The ACT-ONE trial is part of a programme to evaluate the role of MT-102 in cancer cachexia. Participants in ACT-ONE who complete the 16-week treatment period still taking randomised double-blind trial medication will be offered the opportunity to join the ACT-TWO trial. The ACT-TWO trial will continue the same randomised treatment allocations for the period up to that last patient in ACT-ONE having completed all investigations of the ACT-ONE trial and the 16-week period of trial medication. The ACT-TWO trial will be the subject of a separate protocol and design paper and will be separately powered with a different primary endpoint, which will include observations made during the period of double-blind therapy of ACT-ONE as well as the period of double-blind trial medication in ACT-TWO.
References
Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, Guttridge D, et al. Cachexia: a new definition. Clin Nutr. 2008;27:793–9.
von Haehling S, Anker SD. Cachexia as a major underestimated and unmet medical need: facts and numbers. J Cachexia Sarcopenia Muscle. 2010;1:1–5.
Fearon K, Evans WJ, Anker SD. Myopenia-a new universal term for muscle wasting. J Cachexia Sarcopenia Muscle. 2011;2:1–3.
Kilgour RD, Vigano A, Trutschnigg B, Hornby L, Lucar E, Bacon SL, et al. Cancer-related fatigue: the impact of skeletal muscle mass and strength in patients with advanced cancer. J Cachexia Sarcopenia Muscle. 2010;1:177–85.
Braun TP, Marks DL. Pathophysiology and treatment of inflammatory anorexia in chronic disease. J Cachexia Sarcopenia Muscle. 2010;1:135–45.
Akamizu T, Kangawa K. Ghrelin for cachexia. J Cachexia Sarcopenia Muscle. 2010;1:169–76.
Kung T, Springer J, Doehner W, Anker SD, von Haehling S. Novel treatment approaches to cachexia and sarcopenia: highlights from the 5th Cachexia Conference. Expert Opin Investig Drugs. 2010;19:579–85.
Enright PL. The six-minute walk test. Respir Care. 2003;48:783–5. Review.
Bean JF, Kiely DK, LaRose S, Alian J, Frontera WR. Is stair climb power a clinically relevant measure of leg power impairments in at-risk older adults? Arch Phys Med Rehabil. 2007;88:604–9.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94.
Bassey EJ, Harries UJ. Normal values for handgrip strength in 920 men and women aged over 65 years, and longitudinal changes over 4 years in 620 survivors. Clin Sci (Lond). 1993;84:331–7.
Agteresch HJ, Dagnelie PC, van der Gaast A, Stijnen T, Paul Wilson JH. Sample size considerations—randomised clinical trial of adenosine 5-triphosphate in patients with advanced non-small-cell lung cancer. Journal of the National Cancer Institute. 2000;92:321–8.
Wiedenmann B, Malfertheiner P, Friess H, Ritch P, Arseneau J, Mantovani G, et al. A multicenter, phase II study of infliximab plus gemcitabine in pancreatic cancer cachexia. J Support Oncol. 2008;6:18–25.
Jatoi A, Dakhil SR, Nguyen PL, Sloan JA, Kugler JW, Rowland Jr KM, et al. A placebo-controlled double blind trial of etanercept for the cancer anorexia/weight loss syndrome: results from N00C1 from the North Central Cancer Treatment Group. Cancer. 2007;110:1396–403.
Garcia et al. Measuring inconsistency in meta-analyses. Journal of Clinical Oncology, 2007 ASCO Annual Meeting Proceedings Part I. 2007;Vol 25, No 18S, 9133.
von Haehling S, Morley JE, Coats AJ, Anker SD. Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle. J Cachexia Sarcopenia Muscle. 2010;1:7–8.
Acknowledgement
The authors of this manuscript certify that they comply with the Principles of Ethical Publishing in the Journal of Cachexia, Sarcopenia, and Muscle [16].
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Stewart Coats, A.J., Srinivasan, V., Surendran, J. et al. The ACT-ONE trial, a multicentre, randomised, double-blind, placebo-controlled, dose-finding study of the anabolic/catabolic transforming agent, MT-102 in subjects with cachexia related to stage III and IV non-small cell lung cancer and colorectal cancer: study design. J Cachexia Sarcopenia Muscle 2, 201–207 (2011). https://doi.org/10.1007/s13539-011-0046-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13539-011-0046-2