Abstract
In an effort to increase the oral bioavailability of Amphotericin B (AmB), a pH-sensitive drug carrier composed of Tragacanth (Trag) and acrylic acid (AAc) was prepared using γ-irradiation. The swelling behavior of (Trag/AAc) hydrogels was characterized as a function of pH and ionic strength of the swelling medium. The obtained swelling indices revealed the ability of the prepared hydrogel to protect a loaded drug in stomach-simulated medium (Fickian behavior) and to release such drug in intestinal-simulated medium (non-Fickian behavior). In vitro release studies of the antifungal (AmB) were performed to evaluate the hydrogel potential as a drug carrier. The antifungal activity of the prepared oral formulation was investigated in a mouse model of systemic candidiasis. Data revealed that (Trag/AAc)-AmB has a potent antifungal efficacy as demonstrated by prolonging the survival time and reducing the tissue fungal burden, serum antibody titers, as well as inflammatory cytokines in kidney and liver tissues. Furthermore, in vivo toxicity of (Trag/AAc)-AmB was assessed via measuring kidney and liver functions, and results displayed the safety of this novel AmB formulation which was confirmed by histopathological examination. Overall, results indicated that the prepared (Trag/AAc)-AmB is an effective oral delivery system for AmB with better bioavailability and minimal toxicity and could represent a promising approach for improving the therapeutic index of the drug.










Similar content being viewed by others
References
Diro E, van Griensven J, Mohammed R, Colebunders R, Asefa M, Hailu A, et al. Atypical manifestations of visceral leishmaniasis in patients with HIV in north Ethiopia: a gap in guidelines for the management of opportunistic infections in resource poor settings. Lancet Infect Dis. 2015;15(1):122–9. https://doi.org/10.1016/s1473-3099(14)70833-3.
Hussain A, Samad A, Singh SK, Ahsan MN, Haque MW, Faruk A, et al. Nanoemulsion gel-based topical delivery of an antifungal drug: in vitro activity and in vivo evaluation. Drug Deliv. 2016;23(2):652–67. https://doi.org/10.3109/10717544.2014.933284.
Messori A, Fadda V, Maratea D, Trippoli S, Marinai C. Nephrotoxicity of different formulations of amphotericin B: summarizing evidence by network meta-analysis. Clin Infect Dis. 2013;57(12):1783–4. https://doi.org/10.1093/cid/cit588.
Volmer AA, Szpilman AM, Carreira EM. Synthesis and biological evaluation of amphotericin B derivatives. Nat Prod Rep. 2010;27(9):1329–49. https://doi.org/10.1039/b820743g.
Park K. Controlled drug delivery systems: past forward and future back. J Control Release. 2014;190:3–8. https://doi.org/10.1016/j.jconrel.2014.03.054.
Anwar H, Ahmad M, Minhas MU, Rehmani S. Alginate-polyvinyl alcohol based interpenetrating polymer network for prolonged drug therapy, optimization and in-vitro characterization. Carbohydr Polym. 2017;166:183–94. https://doi.org/10.1016/j.carbpol.2017.02.080.
Peppas NA. Devices based on intelligent biopolymers for oral protein delivery. Int J Pharm. 2004;277(1–2):11–7. https://doi.org/10.1016/j.ijpharm.2003.03.001.
Ostroha J, Pong M, Lowman A, Dan N. Controlling the collapse/swelling transition in charged hydrogels. Biomaterials. 2004;25(18):4345–53. https://doi.org/10.1016/j.biomaterials.2003.11.019.
Seeli DS, Prabaharan M. Guar gum oleate-graft-poly(methacrylic acid) hydrogel as a colon-specific controlled drug delivery carrier. Carbohydr Polym. 2017;158:51–7. https://doi.org/10.1016/j.carbpol.2016.11.092.
Ghayempour S, Montazer M, Mahmoudi Rad M. Tragacanth gum as a natural polymeric wall for producing antimicrobial nanocapsules loaded with plant extract. Int J Biol Macromol. 2015;81:514–20. https://doi.org/10.1016/j.ijbiomac.2015.08.041.
Ranjbar-Mohammadi M, Rabbani S, Bahrami SH, Joghataei MT, Moayer F. Antibacterial performance and in vivo diabetic wound healing of curcumin loaded gum tragacanth/poly(ε-caprolactone) electrospun nanofibers. Mater Sci Eng C. 2016;69:1183–91. https://doi.org/10.1016/j.msec.2016.08.032.
Tavakol M, Dehshiri S, Vasheghani-Farahani E. Electron beam irradiation crosslinked hydrogels based on tyramine conjugated gum tragacanth. Carbohydr Polym. 2016;152:504–9. https://doi.org/10.1016/j.carbpol.2016.07.044.
Balaghi S, Mohammadifar MA, Zargaraan A. Physicochemical and rheological characterization of gum Tragacanth exudates from six species of Iranian Astragalus. Food Biophys. 2010;5(1):59–71. https://doi.org/10.1007/s11483-009-9144-5.
Zohuriaan MJ, Shokrolahi F. Thermal studies on natural and modified gums. Polym Test. 2004;23(5):575–9. https://doi.org/10.1016/j.polymertesting.2003.11.001.
Verbeken D, Dierckx S, Dewettinck K. Exudate gums: occurrence, production, and applications. Appl Microbiol Biotechnol. 2003;63(1):10–21. https://doi.org/10.1007/s00253-003-1354-z.
Zafar R, Zia KM, Tabasum S, Jabeen F, Noreen A, Zuber M. Polysaccharide based bionanocomposites, properties and applications: a review. Int J Biol Macromol. 2016;92:1012–24. https://doi.org/10.1016/j.ijbiomac.2016.07.102.
Kiani A, Asempour H. Hydrogel membranes based on gum tragacanth with tunable structures and properties. II. Comprehensive characterization of the swelling behavior. J Appl Polym Sci. 2012;126(S1):E478–E85. https://doi.org/10.1002/app.36782.
Singh B, Varshney L, Francis S, Rajneesh. Designing tragacanth gum based sterile hydrogel by radiation method for use in drug delivery and wound dressing applications. Int J Biol Macromol. 2016;88:586–602. https://doi.org/10.1016/j.ijbiomac.2016.03.051.
Ranjbar-Mohammadi M, Prabhakaran MP, Bahrami SH, Ramakrishna S. Gum tragacanth/poly(l-lactic acid) nanofibrous scaffolds for application in regeneration of peripheral nerve damage. Carbohydr Polym. 2016;140:104–12. https://doi.org/10.1016/j.carbpol.2015.12.012.
Fattahi A, Sadrjavadi K, Golozar MA, Varshosaz J, Fathi M-H, Mirmohammad-Sadeghi H. Preparation and characterization of oligochitosan–tragacanth nanoparticles as a novel gene carrier. Carbohydr Polym. 2013;97(2):277–83. https://doi.org/10.1016/j.carbpol.2013.04.098.
Kiani A, Shahbazi M, Asempour H. Hydrogel membranes based on gum tragacanth with tunable structure and properties. I. Preparation method using Taguchi experimental design. J Appl Polym Sci. 2012;124(1):99–108. https://doi.org/10.1002/app.35038.
Luo K, Li J, Li L, Li J. A facile method for preparing 3D graphene/Ag aerogel via gamma-ray irradiation. Fullerenes, Nanotubes Carbon Nanostruct. 2016;24(11):720–4. https://doi.org/10.1080/1536383x.2016.1224855.
Maggi L, Segale L, Ochoa Machiste E, Faucitano A, Buttafava A, Conte U. Polymers-gamma ray interaction. Effects of gamma irradiation on modified release drug delivery systems for oral administration. Int J Pharm. 2004;269(2):343–51. https://doi.org/10.1016/j.ijpharm.2003.09.027.
Chapiro A. Radiation chemistry of polymers, basic mechanisms in the radiation chemistry of aqueous media. Radiat Res Suppl. 1964;4:451–55. https://doi.org/10.2307/3583578.
Santos DA, Hamdan JS. Evaluation of broth microdilution antifungal susceptibility testing conditions for Trichophyton rubrum. J Clin Microbiol. 2005;43(4):1917–20. https://doi.org/10.1128/JCM.43.4.1917-1920.2005.
Takemoto K, Yamamoto Y, Ueda Y, Sumita Y, Yoshida K, Niki Y. Comparative study on the efficacy of AmBisome and Fungizone in a mouse model of pulmonary aspergillosis. J Antimicrob Chemother. 2006;57(4):724–31. https://doi.org/10.1093/jac/dkl005.
Cocchetto DM, Bjornsson TD. Methods for vascular access and collection of body-fluids from the laboratory rat. J Pharm Sci. 1983;72(5):465–92. https://doi.org/10.1002/jps.2600720503.
Montgomery H, Dymock JF. Determination of nitrite in water. Analyst. 1961;86(102):414-&.
Chen Y, Tang H, Liu Y, Tan H. Preparation and study on the volume phase transition properties of novel carboxymethyl chitosan grafted polyampholyte superabsorbent polymers. J Taiwan Inst Chem Eng. 2016;59:569–77. https://doi.org/10.1016/j.jtice.2015.09.011.
Muthukumar M. Theory of counter-ion condensation on flexible polyelectrolytes: adsorption mechanism. J Chem Phys. 2004;120(19):9343–50. https://doi.org/10.1063/1.1701839.
Eichenbaum GM, Kiser PF, Simon SA, Needham D. pH and ion-triggered volume response of anionic hydrogel microspheres. Macromolecules. 1998;31(15):5084–93. https://doi.org/10.1021/ma970897t.
Drozdov AD, Christiansen JD. Modeling the effects of pH and ionic strength on swelling of anionic polyelectrolyte gels. Model Simul Mater Sci Eng. 2015;23(5):055005. https://doi.org/10.1088/0965-0393/23/5/055005.
Lu H, Du S. A phenomenological thermodynamic model for the chemo-responsive shape memory effect in polymers based on Flory-Huggins solution theory. Polym Chem. 2014;5(4):1155–62. https://doi.org/10.1039/C3PY01256E.
Lin C-C, Metters AT. Hydrogels in controlled release formulations: network design and mathematical modeling. Adv Drug Deliv Rev. 2006;58(12):1379–408. https://doi.org/10.1016/j.addr.2006.09.004.
Glockner A. Treatment and prophylaxis of invasive candidiasis with anidulafungin, caspofungin and micafungin—review of the literature. Eur J Med Res. 2011;16(4):167–79. https://doi.org/10.1186/2047-783X-16-4-167.
Ibrahim F, Gershkovich P, Sivak O, Wasan EK, Bartlett K, Wasan KM. Efficacy and toxicity of a tropically stable lipid-based formulation of amphotericin B (iCo-010) in a rat model of invasive candidiasis. Int J Pharm. 2012;436(1–2):318–23. https://doi.org/10.1016/j.ijpharm.2012.06.062.
Sant VP, Smith D, Leroux J-C. Novel pH-sensitive supramolecular assemblies for oral delivery of poorly water soluble drugs: preparation and characterization. J Control Release. 2004;97(2):301–12. https://doi.org/10.1016/j.jconrel.2004.03.026.
Torosantucci A, Bromuro C, Chiani P, De Bernardis F, Berti F, Galli C, et al. A novel glyco-conjugate vaccine against fungal pathogens. J Exp Med. 2005;202(5):597–606. https://doi.org/10.1084/jem.20050749.
Lopez-Ribot JL, Casanova M, Murgui A, Martinez JP. Antibody response to Candida albicans cell wall antigens. FEMS Immunol Med Microbiol. 2004;41(3):187–96. https://doi.org/10.1016/j.femsim.2004.03.012.
Clancy CJ, Nguyen ML, Cheng SJ, Huang H, Fan GX, Jaber RA, et al. Immunoglobulin G responses to a panel of Candida albicans antigens as accurate and early markers for the presence of systemic candidiasis. J Clin Microbiol. 2008;46(5):1647–54. https://doi.org/10.1128/jcm.02018-07.
Li WQ, Hu XC, Zhang XH, Ge YP, Zhao SN, Hu Y, et al. Immunisation with the glycolytic enzyme enolase confers effective protection against Candida albicans infection in mice. Vaccine. 2011;29(33):5526–33. https://doi.org/10.1016/j.vaccine.2011.05.030.
Dinarello CA. Proinflammatory cytokines. Chest. 2000;118(2):503–8. https://doi.org/10.1378/chest.118.2.503.
Ferrante A. Tumor necrosis factor alpha potentiates neutrophil antimicrobial activity—increased fungicidal activity against torulopsis-glabrata and candida-albicans and associated increases in oxygen radical production and lysosomal-enzyme release. Infect Immun. 1989;57(7):2115–22.
Kumar V, Sharma A. Neutrophils: Cinderella of innate immune system. Int Immunopharmacol. 2010;10(11):1325–34. https://doi.org/10.1016/j.intimp.2010.08.012.
Spellberg B, Ibrahim AS, Edwards JE, Filler SG. Mice with disseminated candidiasis die of progressive sepsis. J Infect Dis. 2005;192(2):336–43. https://doi.org/10.1086/430952.
Dantas AD, Day A, Ikeh M, Kos I, Achan B, Quinn J. Oxidative stress responses in the human fungal pathogen, Candida albicans. Biomol Ther. 2015;5(1):142–65. https://doi.org/10.3390/biom5010142.
MacCallum DM, Odds FC. Temporal events in the intravenous challenge model for experimental Candida albicans infections in female mice. Mycoses. 2005;48(3):151–61. https://doi.org/10.1111/j.1439-0507.2005.01121.x.
Chin VK, Foong KJ, Maha A, Rusliza B, Norhafizah M, Chong PP. Multi-step pathogenesis and induction of local immune response by systemic Candida albicans infection in an intravenous challenge mouse model. Int J Mol Sci. 2014;15(8):14848–67. https://doi.org/10.3390/ijms150814848.
Yamamoto Y, Klein TW, Friedman H. Involvement of mannose receptor in cytokine interleukin-1 beta (IL-1 beta), IL-6, and granulocyte-macrophage colony-stimulating factor responses, but not in chemokine macrophage inflammatory protein 1 beta (MIP-1 beta), MIP-2, and KC responses, caused by attachment of Candida albicans to macrophages. Infect Immun. 1997;65(3):1077–82.
Netea MG, Brown GD, Kullberg BJ, Gow NAR. An integrated model of the recognition of Candida albicans by the innate immune system. Nat Rev Microbiol. 2008;6(1):67–78. https://doi.org/10.1038/nrmicro1815.
MacCallum DM, Castillo L, Brown AJP, Gow NAR, Odds FC. Early-expressed chemokines predict kidney immunopathology in experimental disseminated Candida albicans infections. PLoS One. 2009;4(7):e6420. https://doi.org/10.1371/journal.pone.0006420.
Motoyoshi A, Nakajima H, Takano K, Moriyama M, Kannan Y, Nakamura Y. Effects of Amphotericin B on the expression of neurotoxic and neurotrophic factors in cultured microglia. Neurochem Int. 2008;52(6):1290–6. https://doi.org/10.1016/j.neuint.2008.01.012.
Tonomura Y, Yamamoto E, Kondo C, Itoh A, Tsuchiya N, Uehara T, et al. Amphotericin B-induced nephrotoxicity: characterization of blood and urinary biochemistry and renal morphology in mice. Hum Exp Toxicol. 2009;28(5):293–300. https://doi.org/10.1177/0960327109105404.
Italia JL, Yahya MM, Singh D, Kumar M. Biodegradable nanoparticles improve oral bioavailability of Amphotericin B and show reduced nephrotoxicity compared to intravenous FungizoneA (R). Pharm Res. 2009;26(6):1324–31. https://doi.org/10.1007/s11095-009-9841-2.
Sawaya BP, Briggs JP, Schnermann J. Amphotericin-b nephrotoxicity—the adverse consequences of altered membrane-properties. J Am Soc Nephrol. 1995;6(2):154–64.
Radwan MA, AlQuadeib BT, Siller L, Wright MC, Horrocks B. Oral administration of amphotericin B nanoparticles: antifungal activity, bioavailability and toxicity in rats. Drug Deliv. 2017;24(1):40–50. https://doi.org/10.1080/10717544.2016.1228715.
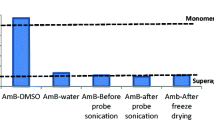
Adams ML, Kwon GS. Relative aggregation state and hemolytic activity of amphotericin B encapsulated by poly(ethylene oxide)-block-poly(N-hexyl-L-aspartamide)-acyl conjugate micelles: effects of acyl chain length. J Control Release. 2003;87(1–3):23–32. https://doi.org/10.1016/s0168-3659(02)00347-4.
Acknowledgements
The authors are very grateful to Prof. Dr. Kawkab A. Ahmed (Pathology Department, Faculty of Veterinary Medicine, Cairo University, Egypt) for her assistance in examining and interpreting histopathologic aspects this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mohamed, H.A., Radwan, R.R., Raafat, A.I. et al. Antifungal activity of oral (Tragacanth/acrylic acid) Amphotericin B carrier for systemic candidiasis: in vitro and in vivo study. Drug Deliv. and Transl. Res. 8, 191–203 (2018). https://doi.org/10.1007/s13346-017-0452-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-017-0452-x