Abstract
Leptomeningeal metastases arise from cancer cell entry into the subarachnoid space, inflicting significant neurologic morbidity and mortality across a wide range of malignancies. The modern era of cancer therapeutics has seen an explosion of molecular-targeting agents and immune-mediated strategies for patients with breast, lung, and melanoma malignancies, with meaningful extracranial disease control and improvement in patient survival. However, the clinical efficacy of these agents in those with leptomeningeal metastases remains understudied, due to the relative rarity of this patient population, the investigational challenges associated with studying this dynamic disease state, and brisk disease pace. Nevertheless, retrospective studies, post hoc analyses, and small prospective trials in the last two decades provide a glimmer of hope for patients with leptomeningeal metastases, suggesting that several cancer-directed strategies are not only active in the intrathecal space but also improve survival against historical odds. The continued development of clinical trials devoted to patients with leptomeningeal metastases is critical to establish robust efficacy outcomes in this patient population, define drug pharmacokinetics in the intrathecal space, and uncover new avenues for treatment in the face of leptomeningeal therapeutic resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
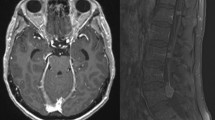
Leptomeningeal metastases (LM) represent an aggressive, advanced stage of cancer with substantial neurologic morbidity and a grim survival of 2–5 months [1, 2]. Also known as leptomeningeal carcinomatosis or neoplastic meningitis, LM occurs when cancer cells gain access to the cerebrospinal fluid (CSF) that surrounds the brain and spinal cord, either through hematogenous dissemination via the choroid plexus, retrograde venous extension, or direct seeding from parenchymal metastases across the glia limitans [3,4,5]. Upon entry, LM adopts two phenotypic states: adherent plaques to the brain and spinal cord visualized with contrast-enhanced magnetic resonance imaging (MRI), and free-floating cells within the spinal fluid detected via CSF cytology [6]. As such, diagnosis and surveillance of LM require full neuraxial MRI and CSF analysis to fully stage the burden of disease [7, 8]. The estimated incidence of LM from systemic malignancies is approximately 5–20% based on population and autopsy data [9,10,11,12]; the true incidence of LM is likely higher owing to insensitivity of CSF cytology and asymptomatic leptomeningeal seeding [13].
Conventional treatment of LM includes intrathecal chemotherapy for those with adequate performance status, whole brain radiation therapy (WBRT) to cranial disease and/or involved-field radiation therapy (RT) to disease of the spinal cord and cauda equina, and systemic chemotherapies with adequate central nervous system (CNS) penetration (Fig. 1). Symptoms referrable to increased intracranial pressure can be ameliorated with palliative ventriculoperitoneal shunting [14]. For those without abnormal CSF flow dynamics, commonly used intrathecal therapy options include methotrexate [15,16,17], thiotepa [18], and topotecan [19]. No single intrathecal chemotherapy has emerged as providing a significant survival benefit, and their use is associated with increased neurotoxicity risk [20,21,22].
Anatomic considerations and conventional therapeutic strategies for leptomeningeal metastases. This illustration outlines the two phenotypic states of leptomeningeal metastases (LM), existing as both free-floating disseminated cells and adherent plaques to the brain and spinal cord. The three pillars of conventional therapies are shown, including intrathecal therapy (blue dots) through an Ommaya reservoir, systemic therapy (yellow dots) entering the cerebrospinal fluid (CSF) via the blood-CSF barrier of the choroid plexus, and involved-field radiation therapy (yellow beam) directed here against the adherent cells of the conus medullaris and cauda equina
While modern targeted therapies and immunotherapy have resulted in meaningful prolongation of survival among certain cancer subtypes, the influence of such agents in the treatment of LM remains largely unexplored. Several challenges explain this investigational discordance. Patients with CNS metastases have long been excluded from clinical trials, perpetuating a pattern of poor outcomes and limited evidence-based data for this patient population. Part of this discrepancy lies in uncertainty regarding drug access to different CNS compartments. The blood–brain barrier (BBB) and blood-CSF barrier (BCSFB) represent two distinct vascular niches with differential pharmacologic permeability [23]; dedicated CSF pharmacokinetic monitoring is essential to understand access and durability of novel drugs into the intrathecal space. Recent neuro-oncologic advocacy has resulted in additional investigational protocols for patients with parenchymal brain metastases; however, LM overwhelmingly remains an exclusion criterion. Furthermore, genetic divergence between brain and extracranial sites of cancer highlights an important mechanism of therapeutic resistance, and intracranial sampling can uncover targetable, oncogenic drivers that are distinct from primary tumor [24, 25]. Basket trials matching intracranial oncogenes with targeted agents aim to capitalize on this principle for those with parenchymal brain metastases (NCT03994796). Genomic characterization of CSF in patients with LM may be similarly capable of providing therapeutic insights [26,27,28]; however, the clinical relevance of this data has not yet been recapitulated in prospective trials. As a result of these limitations, evidence supporting the use of modern targeted therapeutics in patients with LM relies heavily on retrospective reports, post hoc analyses, and small prospective studies (Table 1). Nevertheless, these insights collectively shed light on opportunity for this patient population and have inspired several novel LM-directed therapies currently in development (Table 2).
Radiation Therapy
RT has long been one of the pillars of treatment of LM, typically in the form of WBRT for cranial and involved-field RT for spinal sites of disease [29]. Such strategies aim to provide both palliative and therapeutic effect, primarily to regions of bulky, adherent LM that are less amenable to systemic or intrathecal therapies [30, 31]. However, persistence of dynamic, suspended cancer cells throughout the intrathecal compartment limits the therapeutic durability of focal RT. Without simultaneous inclusion of CSF-penetrant systemic therapies to target disseminated disease, focally radiated sites are at a great risk of reseeding, and the “cytoreduction” benefit afforded by this approach is minimal. Consequently, survival benefit of conventional RT for LM has not been demonstrated in prospective studies, and observational studies are mixed with respect to the prognostic role of WBRT [31].
Unlike involved-field RT with its inherent risks of leaving sites of the CNS untreated, craniospinal irradiation (CSI) offers the ability to radiate the entire neuraxial compartment. The efficacy of photon CSI has been established in many pediatric tumors with leptomeningeal dissemination, such as medulloblastoma, ependymoma, and select hematologic malignancies [31]. However, photon CSI is not without considerable short-term and long-term risks related to exposure of the entire spinal column and visceral organs to radiation, namely myelosuppression, mucositis, endocrine dysfunction, stunted growth in children, and neurotoxicity [32]. These side effects limit the widespread applicability of photon CSI to adults with solid tumor LM, despite potential palliative benefits [33].
Proton craniospinal irradiation (pCSI) largely circumvents the issue of off-target radiation toxicity. The chief advantage of proton over proton radiation is the ability to conform to a narrower range of treatment depth without sacrificing treatment dose, thereby maximizing therapeutic effect and minimizing unintended side-scatter [34, 35]. The safety of hypofractionated pCSI in adults with solid tumor LM has been recently demonstrated in a phase 1b dose-expansion trial [36]. Of 20 evaluable patients treated with dose of 30 Gy in 10 fractions, the most common toxicities of any grade included fatigue (95%) and lymphopenia (90%), both of which were self-limiting in the majority of patients. No grade 3 gastrointestinal toxicities or cytopenias requiring blood transfusions were reported, suggesting more tolerable toxicity as compared to photon CSI. Importantly, treatment with pCSI was effective for both newly diagnosed and recurrent LM. Median overall survival (OS) was 8 months (95% CI: 6-NR) with a median CNS progression-free survival (PFS) of 7 months (95% CI: 5–13).
While small patient numbers and a mixed cancer population limits a more robust efficacy analysis of pCSI, the durability of disease control, seemingly agnostic to cancer type or mutational status, marks pCSI as deserving of further study. More investigation is needed to compare outcomes of pCSI to more conventional photon RT techniques for LM, determine optimal patient selection, and better characterize the short- and long-term toxicities associated with pCSI. A phase II study of pCSI versus involved-field photon RT in patients with solid tumor LM is ongoing (NCT04343573).
Immunotherapy
Immune checkpoint inhibitors have demonstrated efficacy in the treatment of parenchymal brain metastases from melanoma [37, 38], lung adenocarcinoma [39,40,41], renal cell carcinoma [42,43,44], and to a lesser extent breast cancer [45, 46]. However, the activity of these agents within the leptomeningeal compartment appears less robust. While LM is marked by leukocytic pleocytosis, little is known about the migration of peripheral T-cells into intrathecal space [47]. T-lymphocytes within the leptomeninges in patients with LM are also immunologically distinct from matched brain metastases and generally harbor a more immunosuppressive phenotype [48]. Greater numbers of exhausted or dysfunctional CD4 and CD8 cells have been identified in the CSF in patients and animal models harboring LM, which therefore may not respond as consistently to immune checkpoint blockade [48, 49]. In fact, melanoma immunotherapy “non-responders” had consistently elevated numbers of inactivated T-lymphocytes despite changes in the myeloid cells, implying that while PD-1 therapy may alter the leptomeningeal microenvironment, this does not always translate to anti-tumor immunity [48].
Several studies have been conducted to define the role of intravenous immune checkpoint inhibition in patients with LM [50,51,52,53,54]. A phase II study tested intravenous pembrolizumab in 20 patients in LM from solid tumor malignancies [50]. While this study met its pre-specified primary endpoint with a median OS of 3.6 months (90% CI: 2.2–5.2 months), best CNS response was stable disease in 11 individuals with no patients demonstrating reduction in their LM burden. Combination ipilimumab and nivolumab for LM has also recently been studied in a phase II study of 18 patients, with a slightly shorter median OS of 2.9 months (90% CI: 1.6–5.0 months). However, this combination resulted in a complete response in 1 patient and stable disease in 8 patients [51]. Pooled CSF analysis from a subset of patients in these two trials revealed an increase in CD8+ T-lymphocytes and interferon-gamma signaling following immunotherapy administration [55]. This cytotoxic and antigen-processing signature tended to decrease with time, which may provide clues as to the relatively short duration of LM control. Further investigation is warranted to better understand the dynamic changes in the CSF following immune checkpoint inhibitor therapy, the relationship of these fluctuations with treatment response, and the factors that drive CSF T-lymphocytes into an activated rather than exhausted state. Additionally, both studies were enriched in patients with breast cancer. Analysis of these compounds in a higher number of patients with more immunotherapy-responsive malignancies, such as melanoma, might have revealed more durable outcomes. Combinatorial strategies to augment the bioactivity of immunotherapy in the leptomeningeal space are under investigation, including incorporation of WBRT (NCT03719768) [56] or targeted therapies (NCT04729348, NCT04511013, NCT04833205) into the treatment regimen.
There are multiple potential advantages of intrathecal as opposed to intravenous administration of these agents. First, if able to be administered into the intrathecal space safely, direct activation of CSF lymphocytes may provide a more potent and durable cytotoxic destruction of malignant cells in the spinal fluid. Second, directed immunotherapy may help to minimize the systemic autoimmune toxicities inherent to immune checkpoint blockade [57]. The concept of leptomeningeal-delivered immunotherapy has been previously studied in the form of intrathecal IL-2, a potent driver of effector T-cell differentiation [58]. Forty-three patients with melanoma LM treated with intrathecal IL-2 were found retrospectively to have a median survival of 7.8 months (range, 0.4–90.8 months), although treatment-related elevations in intracranial pressure were reported in all patients. Intrathecal administration of nivolumab is currently under investigation, both in combination with intravenous nivolumab in patients with melanoma LM (NCT03025256) and as monotherapy for patients with any solid tumor LM (NCT05112549). Intrathecal human epidermal growth factor receptor 2 (HER2)-chimeric antigen receptor (CAR) T cells, combining molecular targeting with immune-mediated therapy, is another potentially promising strategy still in the early phases of investigation (NCT03696030).
Cancer-Specific Approaches
Systemic treatments of metastatic cancer have evolved considerably in the last two decades due to the incorporation of molecularly targeted treatments into first-line therapy, such as epidermal growth factor receptor (EGFR), anaplastic lymphoma kinase (ALK), and mesenchymal-epithelial transition (MET) pathway inhibitors for non-small-cell lung cancer (NSCLC) and HER2-active treatments for breast cancer. The extrapolation of such data to patients with CNS metastases has been largely limited to post hoc analyses in patients with stable or treated parenchymal brain metastases that were included in clinical trials. Less is known regarding the efficacy of such agents in patients with LM, though bioactivity and potential benefit has been suggested in several small reports.
EGFR-Mutant NSCLC
Activating mutations in the EGFR gene, predominantly exon 19 deletions and exon 21 L858R mutations, are targetable oncogenic drivers of NSCLC [59, 60]. Patients harboring EGFR-mutant NSCLC are more likely to be never-smokers and are at increased risk of both brain and leptomeningeal metastases compared to EGFR-wildtype counterparts.
First- and second-generation EGFR tyrosine kinase inhibitors (TKIs), such as erlotinib, gefitinib, and afatinib, demonstrated activity in LM with detectable CSF concentrations at adequate dosing; however, durability of disease control was short-lived and partially explained by an acquired T790M resistance mutation [61,62,63]. Osimertinib, a third-generation TKI, selectively and irreversibly inhibits many EGFR mutations (including ex19del, L858R, T790M) and is now first-line therapy for patients with EGFR-mutant NSCLC irrespective of T790M status [64]. Osimertinib also demonstrates superior intracranial disease control and has shown promise in multiple clinical trials for patients with LM [65,66,67,68]. The AURA program allowed for inclusion of patients with asymptomatic or stable LM, and retrospectively calculated a LM-objective response rate (ORR) of 55% (95% CI: 32–76) to osimertinib 80 mg daily [65]. The BLOOM study, using a double dose of 160 mg daily to achieve higher CSF concentrations, prospectively determined a slightly higher LM-ORR of 62% (95% CI: 45–78) with a median OS of 11.0 months (95% CI: 8.0–18.0) [66]. A separate phase II analysis also indicated that LM progression while on osimertinib 80 mg may be halted with dose increase to 160 mg, though patient numbers were small and duration of response not reported [67]. To augment both intracranial and extracranial disease control, osimertinib is currently under investigation in combination with pemetrexed and platinum-based therapy (NCT04035486), which will include patients with brain metastases. Osimertinib in combination with bevacizumab, a vascular endothelial growth factor (VEGF) inhibitor, is also under investigation specifically in patients with LM (NCT04425681). Given the impressive disease control of TKIs in select NSCLC patients with targetable mutations, first-line TKI therapy has helped to postpone or even prevent CNS radiation in patients with LM. Despite durable responses of LM to third-generation EGFR inhibitors, acquired resistance inevitably occurs through both EGFR-dependent and EGFR-independent mechanisms [69]. Second-line therapies capable of overcoming osimertinib resistance are needed, with dedicated trials designed for patients with CNS metastases.
MET Genomic Alterations in NSCLC
MET gene amplification is the most frequently encountered alternate bypass pathway conferring EGFR-TKI resistance, seen in 7–15% of patients with progression on first-line osimertinib [69]. To target this mechanism of resistance, combination of amivantamab, an EGFR-MET bispecific antibody with immune cell-directing activity, and lazertinib, a third-generation brain-penetrant EGFR inhibitor, is currently under investigation in both the newly diagnosed (MARIPOSA, NCT04487080) and recurrent (CHRYSALIS, NCT02609776) settings. While data from these trials are not yet mature [70], encouraging preliminary findings have led to the adaptation of combination amivantamab and lazertinib in patients with new or progressive CNS metastases harboring somatic activating EGFR mutations (NCT04965090). This phase II trial has been designed to enroll patients with parenchymal and leptomeningeal metastases in separate arms so as to best define the efficacy of this combination in different CNS compartments.
MET exon 14 skipping mutations occur in 3–4% of patients with NSCLC and are considered mutually exclusive with other oncogenic driver mutations, such as EGFR, HER2, and KRAS [71]. Capmatinib and tepotinib, highly selective inhibitors of the MET receptor, are both FDA-approved for patients with NSCLC harboring MET exon 14 skipping mutations and have demonstrated intracranial responses in clinical trials [72, 73]. Dramatic radiographic leptomeningeal responses have also been suggested in case reports of these two agents, with disease control for at least 5 months in one patient [74, 75].
ALK-Rearranged NSCLC
EML4-ALK fusion mutations are identified in 3–13% of patients with NSCLC and are also enriched in the young, non-smoker population [76, 77]. The brain represents a common site of disease both at initial presentation and relapse; however, only approximately 5% of patients are known to develop LM as a delayed complication [78]. Both second-generation (ceritinib [79], alectinib [80], brigatinib [81]) and third-generation (lorlatinib [82,83,84,85,86]) ALK inhibitors have established superior intracranial efficacy compared to the first-generation ALK inhibitor (crizotinib [87]), though few protocols have specifically studied LM response rates of these individual agents. Improved intracranial control with later generation ALK inhibitors are a consequence of improved BBB and BCSFB penetration, with CSF concentrations approaching 75% that of plasma in the case of lorlatinib [88]. Lorlatinib, with dual ALK and ROS1 inhibition, gained FDA-approval for first line treatment of ALK-rearranged NSCLC following the interim results of the phase III CROWN study, confirming an intracranial ORR of 82% (95% CI: 57–96) among lorlatinib-treated TKI-naïve patients with measurable brain metastases [84].
Prospective data is sparse regarding the duration of LM control with lorlatinib treatment. A prospective phase II study of lorlatinib in patients previously treated with TKIs enrolled 2 patients with ALK+ LM at baseline: one achieved a complete intracranial response for 21.9 months and the second achieved a partial intracranial response for 11 months [83]. The largest dataset of lorlatinib activity in patients with LM comes from an international early/expanded access program of 95 patients, including 13 patients with LM (11 ALK+ and 2 ROS1+) who had progressed on prior TKI therapy [89]. Intracranial ORR in the LM cohort was 45% (95% CI: 17–77) with a disease control rate of 91% (95% CI: 59–100) among 11 evaluable patients. Two patients in the ALK+ cohort had a complete response intracranially. Median PFS was 9.3 months (95% CI: 1.0–NR) in the entire LM cohort. Investigation of a German early access program revealed a partial response rate of 77.8% among 9 patients with LM, but did not provide further details regarding duration of response [90]. While these expanded access datasets are limited due to their retrospective nature and lack of protocolized neuraxial assessments, they complement a number of case reports demonstrating improvement of both LM disease burden and neurologic symptoms following lorlatinib treatment [91,92,93].
HER2-Positive Breast Cancer
Targeted therapies for patients with LM from breast cancer have been mainly restricted to HER2-active agents with adequate CNS penetration. Trastuzumab, while the backbone of combination therapy in patients with HER2+ breast cancer, has negligible CNS penetration which results in high rates of intracranial relapse in this patient population [94]. Approximately 25–50% of HER2+ patients treated with trastuzumab will develop brain metastases and 6–7% will develop LM [95].
While an intrathecal formulation of trastuzumab seems to be well-tolerated across a number of prospective and retrospective studies, conclusions regarding its efficacy have been mixed. A multicenter phase I/II trial determined intrathecal trastuzumab to have minimal toxicity with disease control in 69% of patients with HER2+ breast cancer and LM [96, 97]. However, the primary endpoint (25% RR) was not met and the median PFS was 2.4 months (95% CI 1.0–5.5). A single institution retrospective review of breast cancer LM treatments found a 6-month CNS-PFS of 44% for intrathecal trastuzumab, 18% for intrathecal chemotherapy, and 26% for WBRT. OS was also longer among the intrathecal trastuzumab cohort (54% alive at 12 months compared to 10% for intrathecal chemotherapy and 19% for WBRT, respectively), although confounded by the enrichment of systemic disease and triple-negative breast cancer among the intrathecal chemotherapy and WBRT cohorts [98]. A subsequent meta-analysis of intrathecal trastuzumab across 24 articles calculated a CNS-PFS of 5.2 months (N = 39) and median OS of 13.2 months (N = 54) [99]. Further randomized controlled studies are needed to fully validate the clinical efficacy of intrathecal trastuzumab. The use of WBRT and/or focal RT followed by intrathecal trastuzumab and pertuzumab is currently being investigated in HER2+ LM patients (NCT04588545).
Small molecule HER2-TKIs, namely lapatinib, neratinib, and tucatinib, offer an orally available adjuvant treatment to HER2+ breast cancer patients at the development of brain metastases. Lapatinib and neratinib each confer better intracranial control when in combination with capecitabine compared to monotherapy [100,101,102,103,104]. A few pharmacokinetic series have reported very low concentrations of neratinib and lapatinib in the CSF relative to plasma [105, 106]. Nevertheless, small prospective studies and case reports suggest possible activity of these combinations in patients with LM [103, 104, 107]. A single phase II study investigating neratinib and capecitabine, including 3 patients with LM, found stable and partial responses in 2 patients with disease control of 4 and 7 months, respectively [103]. A phase I study series of intermittent high-dose lapatinib plus capecitabine included 5 patients with LM [104]. Of the 4 patients who completed at least 1 cycle of treatment, 2 patients achieved partial and stable responses and remained on study for at least 6 months.
Tucatinib, a highly-selective third-generation HER2-TKI, demonstrated compelling intracranial activity in the HER2CLIMB trial, which evaluated tucatinib or placebo in combination with trastuzumab and capecitabine in patients with previously-treated HER2+ breast cancer [108]. Exploratory analysis of patients enrolled with active or stable brain metastases revealed a significant improvement in CNS-PFS (9.9 months versus 4.2 month) and median OS (18.1 versus 12.0 months) with the addition of tucatinib [109]. While patients with LM were excluded from this study, these encouraging results prompted the development of a phase II trial of combination tucatinib, trastuzumab, and capecitabine in patients with HER2+ breast cancer and LM (NCT03501979) [110]. Preliminary mass spectrometric analysis of paired CSF and blood samples from this patient cohort suggests detection of both tucatinib and its metabolite, ONT-993, in the CSF [111].
Two FDA-approved antibody–drug conjugates, trastuzumab emtansine (T-DM1) and trastuzumab deruxtecan (T-DXd), facilitate receptor-mediated endocytosis of cytotoxic payloads into HER2+ cells. Exploratory analysis of patients with baseline brain metastases in the phase IIIb KAMILLA and phase III EMILIA studies of T-DM1 found a median PFS of 5.5–5.9 months and median OS of approximately 2 years [112, 113]; however, no results regarding leptomeningeal activity were discussed and only 1 case report to date comments on the activity of T-DM1 in combination with WBRT in a patient with intracranial LM [114]. T-DXd, conversely, offers more potent cytotoxic activity with a higher drug-antibody ratio, use of a potent topoisomerase I compared to a microtubule inhibitor, and a membrane-permeable payload capable of “bystander” activity against HER2-negative or HER2-low cells [115]. While data regarding T-DXd efficacy in LM is not available, an encouraging median PFS of 18.1 months (95% CI: 6.7–18.1) was calculated among patients with brain metastases in the phase II DESTINY-Breast01 study [116]. Several clinical trials of T-DXd for HER2+ cancers are now underway, including the phase II TUXEDO-1 (NCT04752059) [117], DEBBRAH (NCT04420598), and DESTINY-B12 (NCT04739761) studies designed for patients with brain metastases. Importantly, the DEBBRAH study includes a cohort specifically for patients with LM.
Hormone Receptor-Positive Breast Cancer
While endocrine therapy is routinely employed in breast cancer patients with estrogen and progesterone receptor positivity, data regarding hormonal agents in LM are lacking. No prospective clinical trial addresses this question directly for patients with hormone receptor (HR)-positive breast cancer. There is evidence that tamoxifen can concentrate within parenchymal brain metastases; it is also detected at very low levels in the CSF [118, 119]. Preclinical models suggest that letrozole, and to a lesser extent, anastrozole, penetrate the BBB, but it is unknown whether either agent accesses the CSF [120]. This distinction may not be clinically relevant in the case of aromatase inhibitors, as these agents act on peripheral estrogen production as opposed to direct blockade of estrogen receptors. Despite the uncertainty regarding tumor-directed efficacy of hormonal agents in LM, it is worth noting that the use of endocrine therapy after brain or leptomeningeal metastasis diagnosis has been associated with prolonged survival, with no difference identified between choice of endocrine therapy employed [121]. This finding is supported also by a number of case reports suggesting durable response of LM to several hormonal agents, with most cases describing success with letrozole, exemestane, and tamoxifen [122,123,124,125,126].
Resistance to endocrine therapies can occur through both cell-cycle dysregulation and upregulation of the phosphatidylinositol 3-kinase (PI3K)/protein kinase B (AKT)/mammalian target of rapamycin (mTOR) pathway [127]. Combining hormonal agents with an inhibitor of these pathways represents an attractive option mechanistically with meaningful systemic disease control [128,129,130,131]. The bioactivity of such regimens against HR+ brain and leptomeningeal metastases has been suggested in small prospective studies and case reports, although objective responses tend to be small. In phase II study of abemaciclib, a CNS-penetrant cyclin-dependent kinase (CDK) 4/6 inhibitor, with or without endocrine therapy in patients with HR+ breast cancer brain and leptomeningeal metastases, abemaciclib concentrations were roughly equivalent in the plasma and CSF [132]. The intracranial benefit rate was 24% among HR+ HER2− patients. In the LM cohort, 3 of 7 patients with HR+ LM achieved stable disease as best response, with 1 patient experiencing disease control for > 6 months. Combined PFS was 5.9 months (95% CI: 0.7–8.6) and median OS was 8.4 months (95% CI: 3.3–23.5) for the HR+ HER2− LM patients.
No clinical trials to date have reported on the use of PI3K/AKT/mTOR inhibition in patients with breast cancer LM. Alpelisib, an FDA-approved selective PI3Kα inhibitor, has shown modest brain metastasis control in case reports, despite a paucity of data regarding BBB and BCSFB penetration [133]. The brain- and CSF-penetrant pan-PI3K inhibitor, buparlisib, has also demonstrated brain metastasis activity, but its use has been limited by toxicities including transaminitis and hypergylcemia [134,135,136,137]. Paxalisib, a dual PI3K and mTOR inhibitor, is currently under investigation in combination with radiation in patients with LM (NCT04192981).
Triple Negative Breast Cancer
The treatment of CNS metastases from triple negative breast cancer (TNBC) is fraught with challenges, both due to the paucity of targetable agents for these patients and the high frequency with which metastatic disease to the CNS occurs in this population [138]. Consequently, patients with TNBC with brain and leptomeningeal metastases suffer inferior outcomes [139].
Breast cancer patients harboring germline BRCA1 mutations are more likely to express the triple-negative phenotype than those with BRCA2 mutations or BRCA-noncarriers [140, 141]. BRCA1-mutant patients also tend toward higher nuclear grade and tumor burden [140, 141]. Olaparib and talazoparib, two FDA-approved poly ADP ribose polymerase (PARP) inhibitors for breast cancer patients with germline BRCA mutations [142, 143], demonstrate clinical activity against brain metastases [144, 145]. While there are limited data regarding CSF penetration of these agents, durable near-complete responses of LM to olaparib monotherapy have been reported, with disease control lasting >12 months [146,147,148]. Additionally, olaparib resulted in improvement in symptoms and quality of life in these heavily pre-treated patients.
Repurposing of existing chemotherapies to augment brain and CSF penetration is another potential mechanism to improve disease control in TNBC LM patients. For example, paclitaxel has very poor BBB penetration. However, when conjugated with Angiopep-2, an amino acid sequence that binds low-density lipoprotein receptor-related protein-1 at the BBB and BCSFB, paclitaxel demonstrates improved intrathecal penetration [149]. This agent, termed ANG1005 (paclitaxel trevatide), was studied in a phase II trial in patients with breast cancer brain and leptomeningeal metastases, demonstrating an intracranial ORR of 17% (95% CI: 4.7–37.4), intracranial clinical benefit rate of 79% (95% CI: 57.8–92.9), and median PFS of 14.9 weeks (95% CI: 12.7–23.4) among those with LM [149]. Survival rate varied by breast cancer subtype, with a median OS of 9.0 months (95% CI: 5.4–15.2) for HER2+ LM, 7.6 months (95% CI: 1.4–9.4) for HER2− LM, and 2.8 months (95% CI: 0.8–8.7) for TNBC LM. A phase III study of ANG1005 in HER2− breast cancer patients has been designed (NCT03613181).
Finally, capecitabine is an oral prodrug metabolized into the antimetabolite, 5-fluorouracil, and therefore is agnostic to HR and HER2 status in its mechanism of action. Case reports suggest activity of capecitabine against both HR+ and TNBC LM [150,151,152,153]. Intravenous high-dose methotrexate can also be considered for patients with adequate organ function and can obviate the need for intrathecal methotrexate [154].
Melanoma
Melanoma is notorious for CNS dissemination, estimated to occur in 50–75% of patients as per autopsy series [155, 156]. In fact, patients with de novo metastatic melanoma have the highest incidence of brain metastases at diagnosis than any other malignancy [157]. The frequency of LM in melanoma patients ranges from 5 to 30% [158, 159]. Immunotherapy has revolutionized the treatment of melanoma brain metastases, resulting in a 3-year survival of 72% and 37% for those with baseline asymptomatic and symptomatic metastases, respectively [37, 38]. Approximately 40% of melanoma patients harbor a BRAF V600 driver mutation, making them attractive targets of BRAF and MEK inhibitors upon immunotherapy failure. Combination dabrafenib/trametinib and encorafenib/binimetinib both achieve intracranial disease control in patients with melanoma brain metastases, although the duration of intracranial responses tends to be short-lived [160, 161].
The combination of immune checkpoint inhibitors with LM-directed radiation have resulted in durable melanoma LM control in a few case reports [162,163,164,165], but these results have not been recapitulated in prospective studies. One phase II study of ipilimumab and nivolumab in patients with melanoma CNS metastases included 4 patients with LM, none of whom achieved a response [166]. Data regarding intrathecal administration of nivolumab in patients with melanoma is not yet mature (NCT03025256) [167], but if proven successful, might circumvent many of the systemic toxicities associated with immune checkpoint blockade. Other intrathecal immunotherapeutic approaches have achieved durable responses of melanoma LM, including tumor-infiltrating lymphocytes [168] and cytotoxic T-lymphocytes [169]. Prospective clinical investigations are needed to better evaluate these methods in a larger cohort of patients.
There have been no prospective trials to date regarding the efficacy of BRAF and MEK inhibition for melanoma LM. A number of case reports suggest that these agents may be effective against LM, either alone, in combination with immunotherapy, or following LM-directed radiation [165, 170,171,172,173,174,175]. However, despite clear intracranial activity of a number of BRAF and MEK inhibitors, these agents are often substrates to the P-glycoprotein and breast cancer resistance protein drug efflux pumps, with suboptimal intracranial penetration the likely result [176]. The CSF penetration of these agents has not been well characterized. For example, the BRAF inhibitor, vemurafenib, has a low CSF penetration rate with high interindividual variability and no clear correlation with plasma levels [177]. Further exploration of the CSF activity of these agents, and development of reliably CNS-penetrant BRAF/MEK inhibitors, is needed. A phase I first-in-human study of a novel CNS-penetrant BRAF inhibitor, PF-07284890, in combination with binimetinib is underway in patients with intracranial BRAF V600 mutant solid tumor (NCT04543188). Encouragingly, this basket trial includes a cohort for patients with LM. A phase II study of encorafenib, binimetinib, and nivolumab versus ipilimumab and nivolumab in BRAF V600 mutant melanoma patients with brain and leptomeningeal metastases is also currently recruiting (NCT04511013).
Novel Treatments
One of the principal barriers in treating LM is the paucity of knowledge on cancer cell survival in the nutrient-sparse CSF [178]. Unlike metastases to other sites of the body, LM thrive in an anatomic compartment devoid of a blood-tumor capillary network and therefore must acquire nutrients by other means. Identification and depletion of these critical micronutrients in the CSF would place further constraints on LM metabolism and might provide a unique, targeted mechanism of LM treatment. Free iron within the CSF is one such nutrient, found in higher concentrations in the CSF of LM patients compared to non-LM controls [179]. Cancer cells in the CSF uniquely employ a single iron-binding transporter and receptor, lipocalin-2 and SLC22A17, to scavenge iron and sustain their metabolic needs. Exploitation of cancer cell’s dependency on iron using intrathecal administration of an iron chelator, deferoxamine, in preclinical LM models resulted in reduction in CSF iron and diminished LM growth. Furthermore, this reduction in LM burden correlated with significant prolongation of survival in mice. IT-DFO was well tolerated in these preclinical studies, without undue neurologic toxicity. A phase 1a/b dose escalation and expansion study of intrathecal deferoxamine is currently underway in patients with LM from solid tumor malignancies (NCT05184816).
Targeted radioimmunotherapy represents another unique treatment modality for LM, thus far tested most heavily in pediatric patients [180]. 177Lu-omburtamab-DTPA is an intrathecally-administered monoclonal B7H3 antibody labeled with lutetium-177 to deliver focused radioimmunotherapy to tumor cells. B7H3 belongs to the B7 family of immune checkpoint molecules, and its aberrant overexpression in many tumor tissues is a newly recognized marker for metastatic progression [181]. This investigational compound was granted rare pediatric disease designation in 2021 by the FDA, and is currently being evaluated in children with recurrent or refractory medulloblastoma (NCT04167618).
Brachytherapy using liposomally encapsulated radionucleotides is another strategy under investigation for both solid tumor LM and recurrent glioblastoma. Rhenium-186 NanoLiposomes (186RNL), either through intraventricular administration or convection-enhanced delivery, allow for the delivery of beta-emitting radiation with high specificity for CNS tumors and with relative sparing of normal brain tissue [182, 183]. The ReSPECT-LM trial, a phase I dose-finding study of intraventricularly-administered 186RNL in patients with LM, is currently open and enrolling (NCT05034497).
Considerations in LM Clinical Trial Design
The scientific community and organizations responsible for improving outcomes in patients with cancer have made tremendous progress in advocating for CNS-directed clinical trials. Continued development of protocols designed specifically for patients with LM is essential to moving the needle for this underserved population, particularly as the incidence of LM is expected to increase. Important nuances regarding clinical trial design for patients with LM require thoughtful consideration.
First, clinical protocols investigating LM lack standardization and response assessments tend to be unvalidated and time-consuming. Discordant changes in cytologic and radiographic responses can occur, complicated even further by the poor sensitivity of CSF cytology and inability to sufficiently quantify smooth linear leptomeningeal deposits. Most protocols employ modifications of the Response Assessment in Neuro-Oncology (RANO) and European Association of Neuro-Oncology—European Society for Medical Oncology (EANO-ESMO) consensus guidelines [7, 8]. Continued collaborative efforts between consensus groups such as these are essential to provide uniformity and validity to LM response assessments.
Proper clinical endpoint selection in LM clinical trial design is critical in making accurate conclusions regarding therapeutic benefit. Determination of objective responses in LM is challenging due to reasons listed above and may be unreliable in the context of multimodal response assessments. As a result, many clinical protocols choose the primary endpoint of OS in effort to maintain stringency in clinical trial reporting, with comparison to historical control survival data as a marker of success. However, as modern therapies in the last decade improve patient survival, particularly among those with available molecular targets, the historical survival benchmark of 3–4 months may not be the best comparator for all LM subtypes. Furthermore, inclusion of patient-reported outcomes and quality of life assessments are essential to ensure that emerging treatments are not only efficacious but also ameliorate neurologic morbidity.
Finally, CSF circulating tumor cell (CTC) enumeration and circulating tumor DNA analyses represent important quantitative and qualitative biomarkers of LM [97, 184,185,186]. These techniques aim to improve diagnostic sensitivity, identify molecular drivers of site-specific progression and therapeutic resistance, and provide important prognostic and predictive insights [97]. Incorporation of these techniques into clinical trial design may help to optimize patient selection and finesse LM response assessments.
While optimal enrollment strategies, endpoint determination, and biomarker selection in patients with LM require continued refinement, the expansion of LM-directed clinical trials in the last decade is highly encouraging. Clinicians must consider that most conventional treatments for this patient population, such as WBRT and intrathecal therapy, have failed to demonstrate a survival benefit in controlled prospective studies. Therefore, enrollment into therapeutic protocols is paramount to adequately investigate newer translational approaches, and clinical trials should be prioritized whenever possible.
Conclusion
The recent emergence of clinical trials designed specifically for both brain and leptomeningeal metastasis patients is an encouraging testament to scientific progress and patient advocacy. Proton CSI is safe and effective in the treatment of LM, and several modern therapies demonstrate bioactivity in the CSF in small prospective studies and case reports. Discordant drug responses between the brain and leptomeningeal compartments should trigger further investigation, including dedicated clinical protocols designed for LM, pharmacokinetic monitoring to ensure adequate CSF penetration, and biomarker analysis for potential pathways of therapeutic resistance. Further characterizations of the leptomeningeal immune microenvironment and the molecular mechanisms that underlie LM progression have the potential to uncover novel treatments for this underserved patient population.
References
Le Rhun E, Devos P, Weller J, et al. Prognostic validation and clinical implications of the EANO ESMO classification of leptomeningeal metastasis from solid tumors. Neuro Oncol. 2021;23(7):1100–12.
Clarke JL, Perez HR, Jacks LM, Panageas KS, Deangelis LM. Leptomeningeal metastases in the MRI era. Neurology. 2010;74(18):1449–54.
Boire A, Zou Y, Shieh J, et al. Complement component 3 adapts the cerebrospinal fluid for leptomeningeal metastasis. Cell. 2017;168(6):1101-1113.e13.
Kokkoris CP. Leptomeningeal carcinomatosis. How does cancer reach the pia-arachnoid? Cancer. 1983;51(1):154–60.
Yao H, Price TT, Cantelli G, et al. Leukaemia hijacks a neural mechanism to invade the central nervous system. Nature. 2018;560(7716):55–60.
Remsik J, Chi Y, Tong X, et al. Leptomeningeal metastatic cells adopt two phenotypic states. Cancer Rep. 2020:e1236.
Le Rhun E, Weller M, Brandsma D, et al. EANO-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of patients with leptomeningeal metastasis from solid tumours. Ann Oncol. 2017;28(suppl_4):iv84–99.
Chamberlain M, Junck L, Brandsma D, et al. Leptomeningeal metastases: a RANO proposal for response criteria. Neuro Oncol. 2016;19(4):484–92.
Patchell RA, Posner JB. Neurologic complications of systemic cancer. Neurol Clin. 1985;3(4):729–50.
Jeyapalan SA, Batchelor TT. Diagnostic evaluation of neurologic metastases. Cancer Invest. 2000;18(4):381–94.
Glass JP, Melamed M, Chernik NL, Posner JB. Malignant cells in cerebrospinal fluid (CSF): the meaning of a positive CSF cytology. Neurology. 2011;77(20):1793.
Kesari S, Batchelor TT. Leptomeningeal metastases. Neurol Clin. 2003;21(1):25–66.
Glantz MJ, Cole BF, Glantz LK, et al. Cerebrospinal fluid cytology in patients with cancer. Cancer. 1998;82(4):733–9.
Bander ED, Yuan M, Reiner AS, et al. Cerebrospinal fluid diversion for leptomeningeal metastasis: palliative, procedural and oncologic outcomes. J Neurooncol. 2021;154(3):301–13.
Grossman SA, Finkelstein DM, Ruckdeschel JC, et al. Randomized prospective comparison of intraventricular methotrexate and thiotepa in patients with previously untreated neoplastic meningitis Eastern Cooperative Oncology Group. J Clin Oncol. 1993;11(3):561–9.
Glantz MJ, Jaeckle KA, Chamberlain MC, et al. A randomized controlled trial comparing intrathecal sustained-release cytarabine (DepoCyt) to intrathecal methotrexate in patients with neoplastic meningitis from solid tumors. Clin Cancer Res. 1999;5(11):3394–402.
Hitchins RN, Bell DR, Woods RL, Levi JA. A prospective randomized trial of single-agent versus combination chemotherapy in meningeal carcinomatosis. J Clin Oncol. 1987;5(10):1655–62.
Gutin PH, Levi JA, Wiernik PH, Walker MD. Treatment of malignant meningeal disease with intrathecal thioTEPA: a phase II study. Cancer Treat Rep. 1977;61(5):885–7.
Groves MD, Glantz MJ, Chamberlain MC, et al. A multicenter phase II trial of intrathecal topotecan in patients with meningeal malignancies. Neuro Oncol. 2008;10(2):208–15.
Le Rhun E, Wallet J, Mailliez A, et al. Intrathecal liposomal cytarabine plus systemic therapy versus systemic chemotherapy alone for newly diagnosed leptomeningeal metastasis from breast cancer. Neuro Oncol. 2020;22(4):524–38.
Boogerd W, van den Bent MJ, Koehler PJ, et al. The relevance of intraventricular chemotherapy for leptomeningeal metastasis in breast cancer: a randomised study. Eur J Cancer. 2004;40(18):2726–33.
Bokstein F, Lossos A, Siegal T. Leptomeningeal metastases from solid tumors: a comparison of two prospective series treated with and without intra-cerebrospinal fluid chemotherapy. Cancer. 1998;82(9):1756–63.
Jacus MO, Daryani VM, Harstead KE, et al. Pharmacokinetic properties of anticancer agents for the treatment of central nervous system tumors: update of the literature. Clin Pharmacokinet. 2016;55(3):297–311.
Brastianos PK, Carter SL, Santagata S, et al. Genomic characterization of brain metastases reveals branched evolution and potential therapeutic targets. Cancer Discov. 2015;5(11):1164–77.
Brastianos PK, Kim AE, Wang N, et al. Palbociclib demonstrates intracranial activity in progressive brain metastases harboring cyclin-dependent kinase pathway alterations. Nature Cancer. 2021;2(5):498–502.
Deng Z, Cui L, Li P, et al. Genomic comparison between cerebrospinal fluid and primary tumor revealed the genetic events associated with brain metastasis in lung adenocarcinoma. Cell Death Dis. 2021;12(10):935.
Li YS, Jiang BY, Yang JJ, et al. Unique genetic profiles from cerebrospinal fluid cell-free DNA in leptomeningeal metastases of EGFR-mutant non-small-cell lung cancer: a new medium of liquid biopsy. Ann Oncol. 2018;29(4):945–52.
Smalley I, Law V, Wyatt C, et al. Proteomic analysis of CSF from patients with leptomeningeal melanoma metastases identifies signatures associated with disease progression and therapeutic resistance. Clin Cancer Res. 2020;26(9):2163.
Nabors LB, Portnow J, Ahluwalia M, et al. central nervous system cancers, version 3.2020, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2020;18(11):1537–70.
El Shafie RA, Böhm K, Weber D, et al. Palliative radiotherapy for leptomeningeal carcinomatosis–analysis of outcome, prognostic factors, and symptom response. Front Oncol. 2019;8.
Buszek SM, Chung C. Radiotherapy in leptomeningeal disease: a systematic review of randomized and non-randomized trials. Front Oncol. 2019;9:1224.
Fossati P, Ricardi U, Orecchia R. Pediatric medulloblastoma: toxicity of current treatment and potential role of protontherapy. Cancer Treat Rev. 2009;35(1):79–96.
Devecka M, Duma MN, Wilkens JJ, et al. Craniospinal irradiation(CSI) in patients with leptomeningeal metastases: risk-benefit-profile and development of a prognostic score for decision making in the palliative setting. BMC Cancer. 2020;20(1):501.
Brown AP, Barney CL, Grosshans DR, et al. Proton beam craniospinal irradiation reduces acute toxicity for adults with medulloblastoma. Int J Radiat Oncol Biol Phys. 2013;86(2):277–84.
Hopper AB, Chou B, Elster J, et al. A comparison of acute toxicities between vertebral-body-sparing proton craniospinal irradiation and standard photon CSI in pediatric patients. Int J Radiat Oncol Biol Phys. 2019;105(1):E625.
Yang TJ, Wijetunga NA, Yamada J, et al. Clinical trial of proton craniospinal irradiation for leptomeningeal metastases. Neuro Oncol. 2021;23(1):134–43.
Tawbi HA, Forsyth PA, Algazi A, et al. Combined nivolumab and ipilimumab in melanoma metastatic to the brain. N Engl J Med. 2018;379(8):722–30.
Tawbi HA, Forsyth PA, Hodi FS, et al. Long-term outcomes of patients with active melanoma brain metastases treated with combination nivolumab plus ipilimumab (CheckMate 204): final results of an open-label, multicentre, phase 2 study. Lancet Oncol. 2021;22(12):1692–704.
Gauvain C, Vauléon E, Chouaid C, et al. Intracerebral efficacy and tolerance of nivolumab in non–small-cell lung cancer patients with brain metastases. Lung Cancer. 2018;116:62–6.
Li S, Zhang H, Liu T, Chen J, Dang J. The effect of asymptomatic and/or treated brain metastases on efficacy of immune checkpoint inhibitors in metastatic non–small cell lung cancer: a meta-analysis. Front Oncol. 2021;11.
Nadal E, Massuti B, Huidobro G, et al. OA09.02 Atezo-Brain: single arm phase II study of atezolizumab plus chemotherapy in stage IV NSCLC with untreated brain metastases. J Thorac Oncol. 2021;16(10):S863.
Uezono H, Nam D, Kluger HM, et al. Outcomes of stereotactic radiosurgery and immunotherapy in renal cell carcinoma patients with brain metastases. Am J Clin Oncol. 2021;44(9).
Flippot R, Dalban C, Laguerre B, et al. Safety and efficacy of nivolumab in brain metastases from renal cell carcinoma: results of the GETUG-AFU 26 NIVOREN multicenter phase II study. J Clin Oncol. 2019;37(23):2008–16.
Emamekhoo H, Olsen MR, Carthon BC, et al. Safety and efficacy outcomes with nivolumab plus ipilimumab in patients with advanced renal cell carcinoma and brain metastases: results from the CheckMate 920 trial. J Clin Oncol. 2021;39(15_suppl):4515–4515.
Emens LA, Adams S, Barrios CH, et al. First-line atezolizumab plus nab-paclitaxel for unresectable, locally advanced, or metastatic triple-negative breast cancer: IMpassion130 final overall survival analysis. Ann Oncol. 2021;32(8):983–93.
Bailleux C, Eberst L, Bachelot T. Treatment strategies for breast cancer brain metastases. Br J Cancer. 2021;124(1):142–55.
Strazielle N, Creidy R, Malcus C, Boucraut J, Ghersi-Egea JF. T-lymphocytes traffic into the brain across the blood-CSF barrier: evidence using a reconstituted choroid plexus epithelium. PLoS ONE. 2016;11(3):e0150945.
Smalley I, Chen Z, Phadke M, et al. Single-cell characterization of the immune microenvironment of melanoma brain and leptomeningeal metastases. Clin Cancer Res. 2021;27(14):4109–25.
Remsik J, Tong X, Sener U, et al. Abstract 1751: Decoding the immune system response to leptomeningeal metastasis. Can Res. 2021;81(13 Supplement):1751–1751.
Brastianos PK, Lee EQ, Cohen JV, et al. Single-arm, open-label phase 2 trial of pembrolizumab in patients with leptomeningeal carcinomatosis. Nat Med. 2020;26(8):1280–4.
Brastianos PK, Strickland MR, Lee EQ, et al. Phase II study of ipilimumab and nivolumab in leptomeningeal carcinomatosis. Nat Commun. 2021;12(1):5954.
Naidoo J, Schreck KC, Fu W, et al. Pembrolizumab for patients with leptomeningeal metastasis from solid tumors: efficacy, safety, and cerebrospinal fluid biomarkers. J Immunother Cancer. 2021;9(8):e002473.
Remon J, Castro-Henriques M, Esteller L, Vives J. Combination of atezolizumab, bevacizumab, and chemotherapy (IMpower 150) in a patient with NSCLC having leptomeningeal metastases. JTO Clin Res Rep. 2021;2(1).
Arias Ron D, Labandeira CM, Areses Manrique MC, et al. Dramatic response of leptomeningeal carcinomatosis to nivolumab in PD-L1 highly expressive non-small cell lung cancer: a case report. Front Oncol. 2019;9.
Prakadan SM, Alvarez-Breckenridge CA, Markson SC, et al. Genomic and transcriptomic correlates of immunotherapy response within the tumor microenvironment of leptomeningeal metastases. Nat Commun. 2021;12(1):5955.
Pina Y, Chen A, Arrington J, et al. LMD-05. Phase 1B study of avelumab and whole brain radiotherapy (WBRT) in patients with leptomeningeal disease (LMD): preliminary results. Neuro-Oncol Adv. 2021;3(Supplement_3):iii8.
Brahmer JR, Lacchetti C, Schneider BJ, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2018;36(17):1714–68.
Glitza IC, Rohlfs M, Guha-Thakurta N, et al. Retrospective review of metastatic melanoma patients with leptomeningeal disease treated with intrathecal interleukin-2. ESMO Open. 2018;3(1):e000283.
Ge M, Zhuang Y, Zhou X, et al. High probability and frequency of EGFR mutations in non-small cell lung cancer with brain metastases. J Neurooncol. 2017;135(2):413–8.
Li YS, Jiang BY, Yang JJ, et al. Leptomeningeal metastases in patients with NSCLC with EGFR mutations. J Thorac Oncol. 2016;11(11):1962–9.
Lee E, Keam B, Kim DW, et al. Erlotinib versus gefitinib for control of leptomeningeal carcinomatosis in non-small-cell lung cancer. J Thorac Oncol. 2013;8(8):1069–74.
Jackman DM, Cioffredi LA, Jacobs L, et al. A phase I trial of high dose gefitinib for patients with leptomeningeal metastases from non-small cell lung cancer. Oncotarget. 2015;6(6):4527–36.
Tamiya A, Tamiya M, Nishihara T, et al. Cerebrospinal fluid penetration rate and efficacy of afatinib in patients with EGFR mutation-positive non-small cell lung cancer with leptomeningeal carcinomatosis: a multicenter prospective study. Anticancer Res. 2017;37(8):4177–82.
Soria J-C, Ohe Y, Vansteenkiste J, et al. Osimertinib in untreated EGFR-mutated advanced non–small-cell lung cancer. N Engl J Med. 2017;378(2):113–25.
Ahn MJ, Chiu CH, Cheng Y, et al. Osimertinib for patients with leptomeningeal metastases associated with EGFR T790M-positive advanced NSCLC: the AURA leptomeningeal metastases analysis. J Thorac Oncol. 2020;15(4):637–48.
Yang JCH, Kim SW, Kim DW, et al. Osimertinib in patients with epidermal growth factor receptor mutation-positive non-small-cell lung cancer and leptomeningeal metastases: the BLOOM study. J Clin Oncol. 2020;38(6):538–47.
Park S, Lee MH, Seong M, et al. A phase II, multicenter, two cohort study of 160 mg osimertinib in EGFR T790M-positive non-small-cell lung cancer patients with brain metastases or leptomeningeal disease who progressed on prior EGFR TKI therapy. Ann Oncol. 2020;31(10):1397–404.
Nanjo S, Hata A, Okuda C, et al. Standard-dose osimertinib for refractory leptomeningeal metastases in T790M-positive EGFR-mutant non-small cell lung cancer. Br J Cancer. 2018;118(1):32–7.
Leonetti A, Sharma S, Minari R, et al. Resistance mechanisms to osimertinib in EGFR-mutated non-small cell lung cancer. Br J Cancer. 2019;121(9):725–37.
Park K, Haura EB, Leighl NB, et al. Amivantamab in EGFR exon 20 insertion-mutated non-small-cell lung cancer progressing on platinum chemotherapy: initial results from the CHRYSALIS phase I study. J Clin Oncol. 2021;39(30):3391–402.
Tong JH, Yeung SF, Chan AW, et al. MET amplification and exon 14 splice site mutation define unique molecular subgroups of non-small cell lung carcinoma with poor prognosis. Clin Cancer Res. 2016;22(12):3048–56.
Wolf J, Seto T, Han J-Y, et al. Capmatinib in MET exon 14–mutated or MET-amplified non–small-cell lung cancer. N Engl J Med. 2020;383(10):944–57.
Paik PK, Felip E, Veillon R, et al. Tepotinib in non–small-cell lung cancer with MET exon 14 skipping mutations. N Engl J Med. 2020;383(10):931–43.
Cravero P, Vaz N, Ricciuti B, et al. Leptomeningeal response to capmatinib after progression on crizotinib in a patient with MET exon 14-mutant NSCLC. JTO Clin Res Rep. 2020;1(4):100072–100072.
Ninomaru T, Okada H, Fujishima M, et al. Lazarus response to tepotinib for leptomeningeal metastases in a patient with MET exon 14 skipping mutation–positive lung adenocarcinoma: case report. JTO Clinical and Research Reports. 2021;2(3):100145.
Soda M, Choi YL, Enomoto M, et al. Identification of the transforming EML4–ALK fusion gene in non-small-cell lung cancer. Nature. 2007;448(7153):561–6.
Shaw AT, Yeap BY, Mino-Kenudson M, et al. Clinical features and outcome of patients with non–small-cell lung cancer who harbor EML4-ALK. J Clin Oncol. 2009;27(26):4247–53.
Gainor JF. Ou S-HI, Logan J, Borges LF, and Shaw AT, The central nervous system as a sanctuary site in ALK-positive non–small-cell lung cancer. J Thorac Oncol. 2013;8(12):1570–3.
Crinò L, Ahn MJ, De Marinis F, et al. Multicenter phase II study of whole-body and intracranial activity with ceritinib in patients with ALK-rearranged non-small-cell lung cancer previously treated with chemotherapy and crizotinib: results from ASCEND-2. J Clin Oncol. 2016;34(24):2866–73.
Gadgeel SM, Shaw AT, Govindan R, et al. Pooled analysis of CNS response to alectinib in two studies of pretreated patients with ALK-positive non-small-cell lung cancer. J Clin Oncol. 2016;34(34):4079–85.
Camidge DR, Kim DW, Tiseo M, et al. Exploratory analysis of brigatinib activity in patients with anaplastic lymphoma kinase-positive non-small-cell lung cancer and brain metastases in two clinical trials. J Clin Oncol. 2018;36(26):2693–701.
Shaw AT, Felip E, Bauer TM, et al. Lorlatinib in non-small-cell lung cancer with ALK or ROS1 rearrangement: an international, multicentre, open-label, single-arm first-in-man phase 1 trial. Lancet Oncol. 2017;18(12):1590–9.
Bauer TM, Shaw AT, Johnson ML, et al. Brain penetration of lorlatinib: cumulative incidences of CNS and non-CNS progression with lorlatinib in patients with previously treated ALK-positive non-small-cell lung cancer. Target Oncol. 2020;15(1):55–65.
Shaw AT, Bauer TM, de Marinis F, et al. First-line lorlatinib or crizotinib in advanced ALK-positive lung cancer. N Engl J Med. 2020;383(21):2018–29.
Solomon BJ, Besse B, Bauer TM, et al. Lorlatinib in patients with ALK-positive non-small-cell lung cancer: results from a global phase 2 study. Lancet Oncol. 2018;19(12):1654–67.
Felip E, Shaw AT, Bearz A, et al. Intracranial and extracranial efficacy of lorlatinib in patients with ALK-positive non-small-cell lung cancer previously treated with second-generation ALK TKIs. Ann Oncol. 2021;32(5):620–30.
Costa DB, Shaw AT, Ou SH, et al. Clinical experience with crizotinib in patients with advanced ALK-rearranged non-small-cell lung cancer and brain metastases. J Clin Oncol. 2015;33(17):1881–8.
Bauer T, Shaw A, Johnson M, et al. MA08.05 brain penetration of lorlatinib and cumulative incidence rates for CNS and non CNS progression from a phase 1/2 study. J Thorac Oncol. 2018;13(10):S382–3.
Zhu VW, Lin Y-T, Kim D-W, et al. An international real-world analysis of the efficacy and safety of lorlatinib through early or expanded access programs in patients with tyrosine kinase inhibitor–refractory ALK-positive or ROS1-positive NSCLC. J Thorac Oncol. 2020;15(9):1484–96.
Frost N, Christopoulos P, Kauffmann-Guerrero D, et al. Lorlatinib in pretreated ALK- or ROS1-positive lung cancer and impact of TP53 co-mutations: results from the German early access program. Ther Adv Med Oncol. 2021;13:1758835920980558.
Li Z, Li P, Yan B, et al. Sequential ALK inhibitor treatment benefits patient with leptomeningeal metastasis harboring non-EML4-ALK rearrangements detected from cerebrospinal fluid: a case report. Thorac Cancer. 2020;11(1):176–80.
Sun MG, Kim IY, Kim YJ, et al. Lorlatinib therapy for rapid and dramatic control of brain and spinal leptomeningeal metastases from ALK-positive lung adenocarcinoma. Brain Tumor Res Treat. 2021;9(2):100–5.
Gafer H, de Waard Q, Compter A, van den Heuvel M. Rapid regression of neurological symptoms in patients with metastasised ALK+ lung cancer who are treated with lorlatinib: a report of two cases. BMJ Case Rep. 2019;12(7).
Lower EE, Drosick DR, Blau R, et al. Increased rate of brain metastasis with trastuzumab therapy not associated with impaired survival. Clin Breast Cancer. 2003;4(2):114–9.
Bendell JC, Domchek SM, Burstein HJ, et al. Central nervous system metastases in women who receive trastuzumab-based therapy for metastatic breast carcinoma. Cancer. 2003;97(12):2972–7.
Kumthekar P, Gradishar W, Lin N, et al. CMET-22. Intrathecal (It) Traztuzumab (T) for the treatment of leptomeningeal metastases (LM) in patients (pts) with human epidermal growth factor receptor 2-positive (HER2+) cancer: a multicenter phase 1/2 study. Neuro Oncol. 2018;20(suppl_6):vi58.
Malani R, Fleisher M, Kumthekar P, et al. Cerebrospinal fluid circulating tumor cells as a quantifiable measurement of leptomeningeal metastases in patients with HER2 positive cancer. J Neurooncol. 2020;148(3):599–606.
Figura NB, Rizk VT, Mohammadi H, et al. Clinical outcomes of breast leptomeningeal disease treated with intrathecal trastuzumab, intrathecal chemotherapy, or whole brain radiation therapy. Breast Cancer Res Treat. 2019;175(3):781–8.
Zagouri F, Zoumpourlis P, Le Rhun E, et al. Intrathecal administration of anti-HER2 treatment for the treatment of meningeal carcinomatosis in breast cancer: a metanalysis with meta-regression. Cancer Treat Rev. 2020;88:102046.
Lin NU, Diéras V, Paul D, et al. Multicenter phase II study of lapatinib in patients with brain metastases from HER2-positive breast cancer. Clin Cancer Res. 2009;15(4):1452–9.
Bachelot T, Romieu G, Campone M, et al. Lapatinib plus capecitabine in patients with previously untreated brain metastases from HER2-positive metastatic breast cancer (LANDSCAPE): a single-group phase 2 study. Lancet Oncol. 2013;14(1):64–71.
Shawky H, Tawfik H. All-oral combination of lapatinib and capecitabine in patients with brain metastases from HER2-positive breast cancer–a phase II study. J Egypt Natl Canc Inst. 2014;26(4):187–94.
Freedman RA, Gelman RS, Anders CK, et al. TBCRC 022: a phase II trial of neratinib and capecitabine for patients with human epidermal growth factor receptor 2-positive breast cancer and brain metastases. J Clin Oncol. 2019;37(13):1081–9.
Morikawa A, de Stanchina E, Pentsova E, et al. Phase I study of intermittent high-dose lapatinib alternating with capecitabine for HER2-positive breast cancer patients with central nervous system metastases. Clin Cancer Res. 2019;25(13):3784–92.
Gori S, Lunardi G, Inno A, et al. Lapatinib concentration in cerebrospinal fluid in two patients with HER2-positive metastatic breast cancer and brain metastases. Ann Oncol. 2014;25(4):912–3.
Freedman RA, Gelman RS, Agar NYR, et al. Pre- and postoperative neratinib for HER2-positive breast cancer brain metastases: translational breast cancer research consortium 022. Clin Breast Cancer. 2020;20(2):145-151.e2.
Nakao T, Okuda T, Fujita M, Kato A. A case of leptomeningeal metastases of human epidermal growth factor receptor 2-positive breast cancer that responded well to lapatinib plus capecitabine. Surg Neurol Int. 2019;10:131.
Murthy RK, Loi S, Okines A, et al. Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N Engl J Med. 2019;382(7):597–609.
Lin NU, Borges V, Anders C, et al. Intracranial efficacy and survival with tucatinib plus trastuzumab and capecitabine for previously treated HER2-positive breast cancer with brain metastases in the HER2CLIMB trial. J Clin Oncol. 2020;38(23):2610–9.
Murthy RK, O’Brien B, Berry DA, et al. Abstract PD4–02: safety and efficacy of a tucatinib-trastuzumab-capecitabine regimen for treatment of leptomeningeal metastasis (LM) in HER2-positive breast cancer: Results from TBCRC049, a phase 2 non-randomized study. Cancer Res. 2022;82(4_Supplement):PD4-02.
Stringer-Reasor EM, O’Brien BJ, Topletz-Erickson A, et al. Pharmacokinetic (PK) analyses in CSF and plasma from TBCRC049, an ongoing trial to assess the safety and efficacy of the combination of tucatinib, trastuzumab and capecitabine for the treatment of leptomeningeal metastasis (LM) in HER2 positive breast cancer. J Clin Oncol. 2021;39(15_suppl):1044.
Montemurro F, Delaloge S, Barrios CH, et al. Trastuzumab emtansine (T-DM1) in patients with HER2-positive metastatic breast cancer and brain metastases: exploratory final analysis of cohort 1 from KAMILLA, a single-arm phase IIIb clinical trial☆. Ann Oncol. 2020;31(10):1350–8.
Krop IE, Lin NU, Blackwell K, et al. Trastuzumab emtansine (T-DM1) versus lapatinib plus capecitabine in patients with HER2-positive metastatic breast cancer and central nervous system metastases: a retrospective, exploratory analysis in EMILIA. Ann Oncol. 2015;26(1):113–9.
Ricciardi GRR, Russo A, Franchina T, et al. Efficacy of T-DM1 for leptomeningeal and brain metastases in a HER2 positive metastatic breast cancer patient: new directions for systemic therapy - a case report and literature review. BMC Cancer. 2018;18(1):97.
Ferraro E, Drago JZ, Modi S. Implementing antibody-drug conjugates (ADCs) in HER2-positive breast cancer: state of the art and future directions. Breast Cancer Res. 2021;23(1):84.
Modi S, Saura C, Yamashita T, et al. Trastuzumab deruxtecan in previously treated HER2-positive breast cancer. N Engl J Med. 2019;382(7):610–21.
Bartsch R, Berghoff AS, Furtner J, et al. 280P Intracranial activity of trastuzumab-deruxtecan (T-DXd) in HER2-positive breast cancer patients with active brain metastases: results from the first stage of the phase II TUXEDO-1 trial. Ann Oncol. 2021;32:S486.
Lien EA, Wester K, Lønning PE, Solheim E, Ueland PM. Distribution of tamoxifen and metabolites into brain tissue and brain metastases in breast cancer patients. Br J Cancer. 1991;63(4):641–5.
Lien EA, Solheim E, Lea OA, et al. Distribution of 4-hydroxy-N-desmethyltamoxifen and other tamoxifen metabolites in human biological fluids during tamoxifen treatment. Cancer Res. 1989;49(8):2175–83.
Miyajima M, Kusuhara H, Takahashi K, et al. Investigation of the effect of active efflux at the blood-brain barrier on the distribution of nonsteroidal aromatase inhibitors in the central nervous system. J Pharm Sci. 2013;102(9):3309–19.
Bergen ES, Berghoff AS, Medjedovic M, et al. Continued endocrine therapy is associated with improved survival in patients with breast cancer brain metastases. Clin Cancer Res. 2019;25(9):2737–44.
Ozdogan M, Samur M, Bozcuk HS, et al. Durable remission of leptomeningeal metastasis of breast cancer with letrozole: a case report and implications of biomarkers on treatment selection. Jpn J Clin Oncol. 2003;33(5):229–31.
Navarro Martín LM, Fernández AO, Rodríguez Sánchez CA, Martín IR, Cruz Hernández JJ. Durable clinical benefit with exemestane in leptomeningeal metastasis of breast cancer. Clin Transl Oncol. 2005;7(8):358–60.
Boogerd W, Dorresteijn LD, van Der Sande JJ, de Gast GC, Bruning PF. Response of leptomeningeal metastases from breast cancer to hormonal therapy. Neurology. 2000;55(1):117–9.
Zoghi B, Elledge R. Endocrine therapy for leptomeningeal metastases from ER-positive breast cancer: case report and a review of the literature. Breast J. 2016;22(2):218–23.
Fernandes L, Matos LVD, Cardoso D, et al. Endocrine therapy for the treatment of leptomeningeal carcinomatosis in luminal breast cancer: a comprehensive review. CNS Oncology. 2020;9(4):CNS65.
Presti D, Quaquarini E. The PI3K/AKT/mTOR and CDK4/6 pathways in endocrine resistant HR+/HER2- metastatic breast cancer: biological mechanisms and new treatments. Cancers (Basel). 2019;11(9).
Goetz MP, Toi M, Campone M, et al. MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol. 2017;35(32):3638–46.
Rugo HS, Lerebours F, Ciruelos E, et al. Alpelisib plus fulvestrant in PIK3CA-mutated, hormone receptor-positive advanced breast cancer after a CDK4/6 inhibitor (BYLieve): one cohort of a phase 2, multicentre, open-label, non-comparative study. Lancet Oncol. 2021;22(4):489–98.
Jones RH, Casbard A, Carucci M, et al. Fulvestrant plus capivasertib versus placebo after relapse or progression on an aromatase inhibitor in metastatic, oestrogen receptor-positive breast cancer (FAKTION): a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 2020;21(3):345–57.
Baselga J, Campone M, Piccart M, et al. Everolimus in postmenopausal hormone-receptor–positive advanced breast cancer. N Engl J Med. 2011;366(6):520–9.
Tolaney SM, Sahebjam S, Le Rhun E, et al. A phase II study of abemaciclib in patients with brain metastases secondary to hormone receptor–positive breast cancer. Clin Cancer Res. 2020;26(20):5310.
Batalini F, Moulder SL, Winer EP, et al. Response of brain metastases from PIK3CA-mutant breast cancer to alpelisib. JCO Precis Oncol. 2020;4.
de Gooijer MC, Zhang P, Buil LCM, et al. Buparlisib is a brain penetrable pan-PI3K inhibitor. Sci Rep. 2018;8(1):10784.
Di Leo A, Johnston S, Lee KS, et al. Buparlisib plus fulvestrant in postmenopausal women with hormone-receptor-positive, HER2-negative, advanced breast cancer progressing on or after mTOR inhibition (BELLE-3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2018;19(1):87–100.
Grommes C, Pentsova E, Nolan C, et al. Phase II study of single agent buparlisib in recurrent/refractory primary (PCNSL) and secondary CNS lymphoma (SCNSL). Ann Oncol. 2016;27:vi106.
Pistilli B, Pluard T, Urruticoechea A, et al. Phase II study of buparlisib (BKM120) and trastuzumab in patients with HER2+ locally advanced or metastatic breast cancer resistant to trastuzumab-based therapy. Breast Cancer Res Treat. 2018;168(2):357–64.
Jin J, Gao Y, Zhang J, et al. Incidence, pattern and prognosis of brain metastases in patients with metastatic triple negative breast cancer. BMC Cancer. 2018;18(1):446.
Niwińska A, Murawska M, Pogoda K. Breast cancer brain metastases: differences in survival depending on biological subtype, RPA RTOG prognostic class and systemic treatment after whole-brain radiotherapy (WBRT). Ann Oncol. 2010;21(5):942–8.
Atchley DP, Albarracin CT, Lopez A, et al. Clinical and pathologic characteristics of patients with BRCA-positive and BRCA-negative breast cancer. J Clin Oncol. 2008;26(26):4282–8.
Chen H, Wu J, Zhang Z, et al. Association between BRCA status and triple-negative breast cancer: a meta-analysis. Front Pharmacol. 2018;9:909–909.
Robson M, Im S-A, Senkus E, et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377(6):523–33.
Litton JK, Rugo HS, Ettl J, et al. Talazoparib in patients with advanced breast cancer and a germline BRCA mutation. N Engl J Med. 2018;379(8):753–63.
Litton JK, Ettl J, Hurvitz SA, et al. Clinical outcomes in patients (pts) with a history of central nervous system (CNS) metastases receiving talazoparib (TALA) or physician’s choice of chemotherapy (PCT) in the phase 3 EMBRACA trial. J Clin Oncol. 2021;39(15_suppl):1090.
Pascual T, Gonzalez-Farre B, Teixidó C, et al. Significant clinical activity of olaparib in a somatic BRCA1-mutated triple-negative breast cancer with brain metastasis. JCO Precis Oncol. 2019;3:1–6.
Exman P, Mallery RM, Lin NU, Parsons HA. Response to olaparib in a patient with germline BRCA2 mutation and breast cancer leptomeningeal carcinomatosis. NPJ Breast Cancer. 2019;5(1):46.
Bangham M, Goldstein R, Walton H, Ledermann JA. Olaparib treatment for BRCA-mutant ovarian cancer with leptomeningeal disease. Gynecol Oncol Rep. 2016;18:22–4.
Favier L, Truc G, Boidot R, Bengrine-Lefevre L. Long-term response to olaparib in carcinomatous meningitis of a BRCA2 mutated ovarian cancer: a case report. Mol Clin Oncol. 2020;13(1):73–5.
Kumthekar P, Tang S-C, Brenner AJ, et al. ANG1005, a brain-penetrating peptide–drug conjugate, shows activity in patients with breast cancer with leptomeningeal carcinomatosis and recurrent brain metastases. Clin Cancer Res. 2020;26(12):2789–99.
Ekenel M, Hormigo AM, Peak S, Deangelis LM, Abrey LE. Capecitabine therapy of central nervous system metastases from breast cancer. J Neurooncol. 2007;85(2):223–7.
Maur M, Omarini C, Piacentini F, et al. Metronomic capecitabine effectively blocks leptomeningeal carcinomatosis from breast cancer: a case report and literature review. Am J Case Rep. 2017;18:208–11.
Rogers LR, Remer SE, Tejwani S. Durable response of breast cancer leptomeningeal metastasis to capecitabine monotherapy. Neuro Oncol. 2004;6(1):63–4.
Tham YL, Hinckley L, Teh BS, Elledge R. Long-term clinical response in leptomeningeal metastases from breast cancer treated with capecitabine monotherapy: a case report. Clin Breast Cancer. 2006;7(2):164–6.
Glantz MJ, Cole BF, Recht L, et al. High-dose intravenous methotrexate for patients with nonleukemic leptomeningeal cancer: is intrathecal chemotherapy necessary? J Clin Oncol. 1998;16(4):1561–7.
Patel JK, Didolkar MS, Pickren JW, Moore RH. Metastatic pattern of malignant melanoma: a study of 216 autopsy cases. Am J Surg. 1978;135(6):807–10.
Posner JB, Chernik NL. Intracranial metastases from systemic cancer. Adv Neurol. 1978;19:579–92.
Cagney DN, Martin AM, Catalano PJ, et al. Incidence and prognosis of patients with brain metastases at diagnosis of systemic malignancy: a population-based study. Neuro Oncol. 2017;19(11):1511–21.
Raizer JJ, Hwu W-J, Panageas KS, et al. Brain and leptomeningeal metastases from cutaneous melanoma: survival outcomes based on clinical features. Neuro Oncol. 2008;10(2):199–207.
Groves MD, Hess KR, Puduvalli VK, et al. Biomarkers of disease: cerebrospinal fluid vascular endothelial growth factor (VEGF) and stromal cell derived factor (SDF)-1 levels in patients with neoplastic meningitis (NM) due to breast cancer, lung cancer and melanoma. J Neurooncol. 2009;94(2):229–34.
Davies MA, Saiag P, Robert C, et al. Dabrafenib plus trametinib in patients with BRAF(V600)-mutant melanoma brain metastases (COMBI-MB): a multicentre, multicohort, open-label, phase 2 trial. Lancet Oncol. 2017;18(7):863–73.
Holbrook K, Lutzky J, Davies MA, et al. Intracranial antitumor activity with encorafenib plus binimetinib in patients with melanoma brain metastases: a case series. Cancer. 2020;126(3):523–30.
Marinova AM, Reilly JL, Wong V, Weiss S, Olszanski AJ. Metastatic melanoma with leptomeningeal disease. J Adv Pract Oncol. 2021;12(1):79–83.
Bot I, Blank CU, Brandsma D. Clinical and radiological response of leptomeningeal melanoma after whole brain radiotherapy and ipilimumab. J Neurol. 2012;259(9):1976–8.
Glitza IC, Bucheit AD. Clincial response of central nervous system melanoma to anti-PD1 therapy in 2 melanoma patients. Arch Immunol. 2017;1(1).
Arasaratnam M, Hong A, Shivalingam B, et al. Leptomeningeal melanoma—a case series in the era of modern systemic therapy. Pigment Cell Melanoma Res. 2018;31(1):120–4.
Long GV, Atkinson V, Lo S, et al. Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: a multicentre randomised phase 2 study. Lancet Oncol. 2018;19(5):672–81.
Glitza IC, Phillips S, Brown C, et al. Single-center phase I/Ib study of concurrent intrathecal (IT) and intravenous (IV) nivolumab (N) for metastatic melanoma (MM) patients (pts) with leptomeningeal disease (LMD). J Clin Oncol. 2020;38(15_suppl):10008.
Glitza IC, Haymaker C, Bernatchez C, et al. Intrathecal administration of tumor-infiltrating lymphocytes is well tolerated in a patient with leptomeningeal disease from metastatic melanoma: a case report. Cancer Immunol Res. 2015;3(11):1201–6.
Clemons-Miller AR, Chatta GS, Hutchins L, et al. Intrathecal cytotoxic T-cell immunotherapy for metastatic leptomeningeal melanoma. Clin Cancer Res. 2001;7(3 Suppl):917s–24s.
Floudas CS, Chandra AB, Xu Y. Vemurafenib in leptomeningeal carcinomatosis from melanoma: a case report of near-complete response and prolonged survival. Melanoma Res. 2016;26(3):312–5.
Glitza IC, Ferguson SD, Guha-Thakurta N. Rapid resolution of leptomeningeal disease with targeted therapy in a metastatic melanoma patient. J Neurooncol. 2017;133(3):663–5.
Kim DW, Barcena E, Mehta UN, et al. Prolonged survival of a patient with metastatic leptomeningeal melanoma treated with BRAF inhibition-based therapy: a case report. BMC Cancer. 2015;15(1):400.
Lee JM, Mehta UN, Dsouza LH, et al. Long-term stabilization of leptomeningeal disease with whole-brain radiation therapy in a patient with metastatic melanoma treated with vemurafenib: a case report. Melanoma Res. 2013;23(2):175–8.
Schäfer N, Scheffler B, Stuplich M, et al. Vemurafenib for leptomeningeal melanomatosis. J Clin Oncol. 2013;31(11):e173–4.
Wilgenhof S, Neyns B. Complete cytologic remission of V600E BRAF-mutant melanoma-associated leptomeningeal carcinomatosis upon treatment with dabrafenib. J Clin Oncol. 2015;33(28):e109–11.
Vaidhyanathan S, Mittapalli RK, Sarkaria JN, Elmquist WF. Factors influencing the CNS distribution of a novel MEK-1/2 inhibitor: implications for combination therapy for melanoma brain metastases. Drug Metab Dispos. 2014;42(8):1292–300.
Sakji-Dupré L, Le Rhun E, Templier C, et al. Cerebrospinal fluid concentrations of vemurafenib in patients treated for brain metastatic BRAF-V600 mutated melanoma. Melanoma Res. 2015;25(4):302–5.
Spector R, Robert Snodgrass S, Johanson CE. A balanced view of the cerebrospinal fluid composition and functions: focus on adult humans. Exp Neurol. 2015;273:57–68.
Chi Y, Remsik J, Kiseliovas V, et al. Cancer cells deploy lipocalin-2 to collect limiting iron in leptomeningeal metastasis. Science. 2020;369(6501):276–82.
Kramer K, Cheung NK, Humm JL, et al. Targeted radioimmunotherapy for leptomeningeal cancer using (131)I-3F8. Med Pediatr Oncol. 2000;35(6):716–8.
Dong P, Xiong Y, Yue J, Hanley SJB, Watari H. B7H3 as a promoter of metastasis and promising therapeutic target. Front Oncol. 2018;8.
Phillips WT, Goins B, Bao A, et al. Rhenium-186 liposomes as convection-enhanced nanoparticle brachytherapy for treatment of glioblastoma. Neuro Oncol. 2012;14(4):416–25.
Brenner A, Bao A, Phillips W, et al. CTNI-29. Safety and feasibility of rhenium-186 nanoliposome (186RNL) in recurrent glioma: the ReSPECT™ phase 1 trial. Neuro Oncol. 2021;23(Supplement_6):vi65–6.
Nevel KS, Wilcox JA, Robell LJ, Umemura Y. The utility of liquid biopsy in central nervous system malignancies. Curr Oncol Rep. 2018;20(8):60.
Nevel KS, DiStefano N, Lin X, et al. A retrospective, quantitative assessment of disease burden in patients with leptomeningeal metastases from non-small-cell lung cancer. Neuro Oncol. 2020;22(5):675–83.
Lin X, Fleisher M, Rosenblum M, et al. Cerebrospinal fluid circulating tumor cells: a novel tool to diagnose leptomeningeal metastases from epithelial tumors. Neuro Oncol. 2017;19(9):1248–54.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wilcox, J.A., Li, M.J. & Boire, A.A. Leptomeningeal Metastases: New Opportunities in the Modern Era. Neurotherapeutics 19, 1782–1798 (2022). https://doi.org/10.1007/s13311-022-01261-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-022-01261-4