Abstract
Objective
To determine the risk factors for developing primary postoperative pulmonary complications (PPC) in patients undergoing minimally invasive colorectal surgery (MIS) for the treatment of cancer and to identify the potential indicators for more extensive preoperative evaluation.
Materials and methods
The ACS-NSQIP® database was interrogated to capture patients who had elective colon or rectal cancer and underwent MIS between 2012 and 2017. Patients who had primary PPC including pneumonia, unplanned intubation and/or failure to wean from mechanical ventilation for > 48 h were compared to patients without PPC. Significant risk factors for PPC were retained to build a predictive risk model through logistic regression analysis. The model was then internally validated using 2018 data.
Results
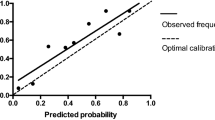
Of 50,150 patients identified, 637 (1.3%) had PPC. The final risk prediction model included six variables: history of chronic obstructive pulmonary disease, age, smoking status, functional health status, pre-operative congestive heart failure, and American Society of Anesthesiology class ≥ 3. The model achieved good calibration (Hosmer–Lemeshow goodness-of-fit test, p = 0.614) and discrimination (c statistics = 0.757). Internal validation achieved similar discrimination (c statistics = 0.798).
Conclusion
Primary postoperative pulmonary complications affected 1.3% of patients undergoing MIS for colon or rectal cancer. The novel predictive risk score showed good discrimination and may help to identify patients who may benefit from perioperative optimization.

Similar content being viewed by others
References
Jurt J, Hubner M, Pache B, Hahnloser D, Demartines N, Grass F (2018) Respiratory complications after colorectal surgery: avoidable or fate? World J Surg 42(9):2708–2714. https://doi.org/10.1007/s00268-018-4699-2
Miskovic A, Lumb AB (2017) Postoperative pulmonary complications. Br J Anaesth 118(3):317–334. https://doi.org/10.1093/bja/aex002
Haines KJ, Skinner EH, Berney S (2013) Association of postoperative pulmonary complications with delayed mobilisation following major abdominal surgery: an observational cohort study. Physiotherapy 99(2):119–125. https://doi.org/10.1016/j.physio.2012.05.013
Zogg CK, Najjar P, Diaz AJ, Zogg DL, Tsai TC, Rose JA Jr, Scott JW, Gani F, Alshaikh H, Canner JK, Schneider EB, Goldberg JE, Haider AH (2016) Rethinking priorities: cost of complications after elective colectomy. Ann Surg 264(2):312–322. https://doi.org/10.1097/sla.0000000000001511
Rauh R, Hemmerling TM, Rist M, Jacobi KE (2001) Influence of pneumoperitoneum and patient positioning on respiratory system compliance. J Clin Anesth 13(5):361–365. https://doi.org/10.1016/s0952-8180(01)00286-0
O'Malley C, Cunningham AJ (2001) Physiologic changes during laparoscopy. Anesthesiol Clin N Am 19(1):1–19. https://doi.org/10.1016/s0889-8537(05)70208-x
Milone M, Elmore U, Vignali A, Mellano A, Gennarelli N, Manigrasso M, Milone F, De Palma GD, Muratore A, Rosati R (2017) Pulmonary complications after surgery for rectal cancer in elderly patients: evaluation of laparoscopic versus open approach from a multicenter study on 477 consecutive cases. Gastroenterol Res Pract 2017:5893890. https://doi.org/10.1155/2017/5893890
Li Y, Wang S, Gao S, Yang C, Yang W, Guo S (2016) Laparoscopic colorectal resection versus open colorectal resection in octogenarians: a systematic review and meta-analysis of safety and efficacy. Tech Coloproctol 20(3):153–162. https://doi.org/10.1007/s10151-015-1419-x
Abd El Aziz MA, Grass F, Behm KT, Shawki S, D'Angelo AL, Mathis KL, Larson DW (2020) Trends of complications and innovative techniques' utilization for colectomies in the United States. Updates Surg. https://doi.org/10.1007/s13304-020-00862-y
Abd El Aziz MA, Grass F, Perry W, Behm KT, Shawki SF, Larson DW, Mathis KL (2020) Colectomy for patients with super obesity: current practice and surgical morbidity in the United States. Surg Obes Relat Dis. https://doi.org/10.1016/j.soard.2020.06.033
Sujatha-Bhaskar S, Alizadeh RF, Inaba CS, Koh CY, Jafari MD, Mills SD, Carmichael JC, Stamos MJ, Pigazzi A (2018) Respiratory complications after colonic procedures in chronic obstructive pulmonary disease: does laparoscopy offer a benefit? Surg Endosc 32(3):1280–1285. https://doi.org/10.1007/s00464-017-5805-5
Antoniou SA, Antoniou GA, Koch OO, Kohler G, Pointner R, Granderath FA (2015) Laparoscopic versus open obesity surgery: a meta-analysis of pulmonary complications. Dig Surg 32(2):98–107. https://doi.org/10.1159/000371749
Lee CZ, Kao LT, Lin HC, Wei PL (2015) Comparison of clinical outcome between laparoscopic and open right hemicolectomy: a nationwide study. World J Surg Oncol 13:250. https://doi.org/10.1186/s12957-015-0666-7
Bablekos GD, Michaelides SA, Analitis A, Charalabopoulos KA (2014) Effects of laparoscopic cholecystectomy on lung function: a systematic review. World J Gastroenterol 20(46):17603–17617. https://doi.org/10.3748/wjg.v20.i46.17603
Jiang L, Yang KH, Guan QL, Cao N, Chen Y, Zhao P, Chen YL, Yao L (2013) Laparoscopy-assisted gastrectomy versus open gastrectomy for resectable gastric cancer: an update meta-analysis based on randomized controlled trials. Surg Endosc 27(7):2466–2480. https://doi.org/10.1007/s00464-012-2758-6
Schiphorst AH, Verweij NM, Pronk A, Borel Rinkes IH, Hamaker ME (2015) Non-surgical complications after laparoscopic and open surgery for colorectal cancer—a systematic review of randomised controlled trials. Eur J Surg Oncol 41(9):1118–1127. https://doi.org/10.1016/j.ejso.2015.04.007
Hall JC, Tarala RA, Hall JL, Mander J (1991) A multivariate analysis of the risk of pulmonary complications after laparotomy. Chest 99(4):923–927. https://doi.org/10.1378/chest.99.4.923
Kapoor A, Nassir A, Chew B, Gillis A, Luke P, Whelan P (2004) Comparison of laparoscopic radical renal surgery in morbidly obese and non-obese patients. J Endourol 18(7):657–660. https://doi.org/10.1089/end.2004.18.657
Gupta H, Gupta PK, Schuller D, Fang X, Miller WJ, Modrykamien A, Wichman TO, Morrow LE (2013) Development and validation of a risk calculator for predicting postoperative pneumonia. Mayo Clin Proc 88(11):1241–1249. https://doi.org/10.1016/j.mayocp.2013.06.027
Arozullah AM, Daley J, Henderson WG, Khuri SF (2000) Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg 232(2):242–253. https://doi.org/10.1097/00000658-200008000-00015
Gupta H, Gupta PK, Fang X, Miller WJ, Cemaj S, Forse RA, Morrow LE (2011) Development and validation of a risk calculator predicting postoperative respiratory failure. Chest 140(5):1207–1215. https://doi.org/10.1378/chest.11-0466
Canet J, Sabate S, Mazo V, Gallart L, de Abreu MG, Belda J, Langeron O, Hoeft A, Pelosi P (2015) Development and validation of a score to predict postoperative respiratory failure in a multicentre European cohort: a prospective, observational study. Eur J Anaesthesiol 32(7):458–470. https://doi.org/10.1097/eja.0000000000000223
Hua M, Brady JE, Li G (2012) A scoring system to predict unplanned intubation in patients having undergone major surgical procedures. Anesth Analg 115(1):88–94. https://doi.org/10.1213/ANE.0b013e318257012b
Blum JM, Stentz MJ, Dechert R, Jewell E, Engoren M, Rosenberg AL, Park PK (2013) Preoperative and intraoperative predictors of postoperative acute respiratory distress syndrome in a general surgical population. Anesthesiology 118(1):19–29. https://doi.org/10.1097/ALN.0b013e3182794975
Kor DJ, Warner DO, Alsara A, Fernandez-Perez ER, Malinchoc M, Kashyap R, Li G, Gajic O (2011) Derivation and diagnostic accuracy of the surgical lung injury prediction model. Anesthesiology 115(1):117–128. https://doi.org/10.1097/ALN.0b013e31821b5839
Jeong BH, Shin B, Eom JS, Yoo H, Song W, Han S, Lee KJ, Jeon K, Um SW, Koh WJ, Suh GY, Chung MP, Kim H, Kwon OJ, Woo S, Park HY (2014) Development of a prediction rule for estimating postoperative pulmonary complications. PLoS ONE 9(12):e113656. https://doi.org/10.1371/journal.pone.0113656
Wong DH, Weber EC, Schell MJ, Wong AB, Anderson CT, Barker SJ (1995) Factors associated with postoperative pulmonary complications in patients with severe chronic obstructive pulmonary disease. Anesth Analg 80(2):276–284. https://doi.org/10.1097/00000539-199502000-00013
Canet J, Gallart L, Gomar C, Paluzie G, Valles J, Castillo J, Sabate S, Mazo V, Briones Z, Sanchis J (2010) Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology 113(6):1338–1350. https://doi.org/10.1097/ALN.0b013e3181fc6e0a
Mazo V, Sabate S, Canet J, Gallart L, de Abreu MG, Belda J, Langeron O, Hoeft A, Pelosi P (2014) Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology 121(2):219–231. https://doi.org/10.1097/aln.0000000000000334
Bare M, Monton C, Mora L, Redondo M, Pont M, Escobar A, Sarasqueta C, Fernandez de Larrea N, Briones E, Quintana JM (2017) COPD is a clear risk factor for increased use of resources and adverse outcomes in patients undergoing intervention for colorectal cancer: a nationwide study in Spain. Int J Chronic Obstr Pulmon Dis 12:1233–1241. https://doi.org/10.2147/copd.S130377
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M (2014) Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg 38(6):1531–1541. https://doi.org/10.1007/s00268-013-2416-8
Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N, McNaught CE, Macfie J, Liberman AS, Soop M, Hill A, Kennedy RH, Lobo DN, Fearon K, Ljungqvist O (2013) Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS((R))) Society recommendations. World J Surg 37(2):259–284. https://doi.org/10.1007/s00268-012-1772-0
Funding
This research did not receive any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interst.
Ethical approval
Institutional Review Board approval was not required for this study.
Research involving human participants and/or animals
This article does not contain any experimental studies with human participants or animals performed by any of the authors.
Informed consent
For this study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abd El Aziz, M.A., Perry, W.R., Grass, F. et al. Predicting primary postoperative pulmonary complications in patients undergoing minimally invasive surgery for colorectal cancer. Updates Surg 72, 977–983 (2020). https://doi.org/10.1007/s13304-020-00892-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00892-6